Descripción general
Electrocardiograma
Electrocardiograma
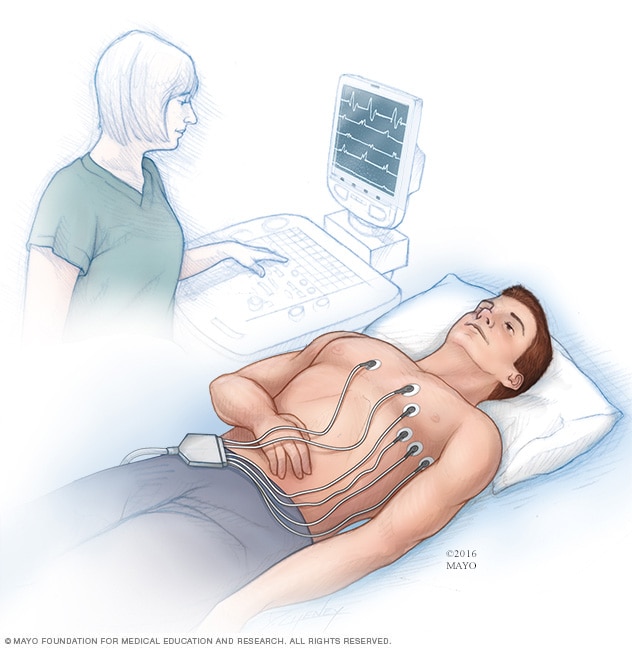
Un electrocardiograma registra las señales eléctricas del corazón y muestra cómo late. Se colocan electrodos, que son sensores, en el pecho para registrar las señales eléctricas del corazón. Las señales se muestran como ondas en un monitor o en una impresora conectados a una computadora.
Un electrocardiograma (o electrocardiografía) es una prueba rápida en la que se revisan los latidos cardíacos y se registran las señales eléctricas del corazón. Los resultados de la prueba pueden ayudar a diagnosticar ataques cardíacos y arritmias, que son latidos cardíacos irregulares.
El aparato para hacer electrocardiogramas se puede encontrar en consultorios, hospitales, quirófanos y ambulancias. Algunos dispositivos personales, como los relojes inteligentes, pueden realizar electrocardiogramas simples. Pregúntale al profesional de atención médica si esta podría ser una opción para ti.
Productos y servicios
Tipos
Por qué se realiza
Un electrocardiograma (o electrocardiografía) se realiza para revisar los latidos cardíacos. Muestra cuán rápido o cuán lento late el corazón. Los resultados de un electrocardiograma pueden ayudar a tu equipo de atención médica a diagnosticar:
- Arritmias, que son ritmos cardíacos irregulares.
- Un ataque cardíaco anterior.
- La causa del dolor en el pecho. Por ejemplo, puede mostrar signos de arterias cardíacas obstruidas o estrechas.
Un electrocardiograma también puede realizarse para saber si un marcapasos o los tratamientos contra una enfermedad cardíaca están funcionando bien.
Es posible que necesites un electrocardiograma si tienes:
- Dolor en el pecho
- Mareos, aturdimiento o confusión
- Latidos cardíacos palpitantes, entrecortados o con aleteo
- Pulso acelerado
- Falta de aire
- Debilidad o fatiga
- Menor capacidad para hacer ejercicio
Si tienes antecedentes familiares de enfermedades cardíacas, puede que necesites un electrocardiograma para detectar enfermedades cardíacas, aunque no tengas síntomas. La Asociación Americana del Corazón afirma que las personas con bajo riesgo para enfermedades cardíacas en general pueden considerar que les hagan un electrocardiograma, aunque no presenten síntomas. La mayoría de los cardiólogos consideran que un electrocardiograma es una herramienta básica en la detección de enfermedades cardíacas, aunque su uso debe ser personalizado.
Si los síntomas suelen aparecer y desaparecer, puede que no se encuentre un cambio en los latidos cardíacos en un electrocardiograma regular. El equipo de atención médica puede recomendarte usar un monitor de electrocardiograma en casa. Existen muchos tipos de dispositivos para electrocardiogramas portátiles.
- Monitor Holter. Este pequeño dispositivo portátil para electrocardiogramas se usa durante un día, o más, para registrar la actividad del corazón. Se usa mientras estás en casa y durante las actividades diarias.
- Monitor de eventos. Este dispositivo es como el monitor Holter, pero registra información solamente en momentos determinados y durante algunos minutos por vez. Por lo general, debes usarlo por aproximadamente 30 días y presionar un botón cada vez que tienes síntomas. Algunos dispositivos registran datos automáticamente cuando se presenta un ritmo cardíaco irregular.
Algunos dispositivos personales, como los relojes inteligentes, tienen aplicaciones de electrocardiograma. Pregúntale a tu equipo de atención médica si esta podría ser una opción para ti.
 Electrocardiograma en un helicóptero médico
Electrocardiograma en un helicóptero médico
Una persona se somete a un electrocardiograma mientras está en un helicóptero de transporte médico.
Más información
Riesgos
No existe ningún riesgo de choque eléctrico durante un electrocardiograma. Los electrodos son sensores que no dan electricidad.
Algunas personas pueden presentar un sarpullido leve en el lugar donde se les colocaron los electrodos. Algunas personas pueden sentir un poco de incomodidad al quitar los parches. Es similar a quitarse un vendaje.
Cómo prepararse
No debes hacer nada para prepararte para un electrocardiograma (o electrocardiografía). Informa al equipo de atención médica todos los medicamentos que tomas, incluidos los adquiridos sin receta médica. Algunos medicamentos y suplementos pueden afectar los resultados de la prueba.
Lo que puedes esperar
Un electrocardiograma (o electrocardiografía) se puede realizar en un consultorio médico o en un hospital. La prueba también se puede realizar en una ambulancia u otro vehículo de emergencia.
Antes
Antes de que te realicen un electrocardiograma, puede que te pidan que te pongas una bata de hospital. Un miembro del equipo de atención médica podría afeitar el vello del área donde colocan el electrodo. Esto ayuda a que el parche se pegue mejor a la piel.
Una vez que estés listo, por lo general, te acuestas en una mesa o camilla de exploración.
Durante
Durante un electrocardiograma, se adhieren hasta 12 electrodos, que son parches adhesivos, al pecho y a veces a los brazos y las piernas. Los parches se conectan a una computadora mediante cables. La computadora imprime o muestra los resultados. Los resultados se muestran como ondas. Las ondas son las señales que viajan por el corazón en cada latido cardíaco.
Puedes respirar durante el electrocardiograma, aunque no debes moverte ni hablar, ya que el movimiento puede interferir con los resultados de la prueba.
Después
A menos que tengas un problema cardíaco que requiera tratamiento inmediato, por lo general, podrás retomar tus actividades diarias después de un electrocardiograma.
Resultados
El profesional de atención médica puede hablar contigo sobre los resultados del electrocardiograma (o electrocardiografía) el mismo día que te hizo la prueba. A veces te comparten los resultados en la cita siguiente.
Un profesional de atención médica busca patrones de señales cardíacas en los resultados del electrocardiograma. Al hacerlo, obtiene información sobre la salud del corazón, por ejemplo:
- Frecuencia cardíaca. La frecuencia cardíaca es la cantidad de veces que el corazón late por minuto. Puedes medirla al comprobar tu pulso. Sin embargo, un electrocardiograma resulta útil si es difícil detectar el pulso o si este es muy irregular como para contabilizarlo con precisión. Los resultados de un electrocardiograma pueden ayudar a diagnosticar la taquicardia, que es una frecuencia cardíaca inusualmente acelerada, o la bradicardia, que es una frecuencia cardíaca inusualmente lenta.
- Ritmo cardíaco. El ritmo del corazón es el tiempo que transcurre entre cada latido cardíaco. También es el patrón de señales entre cada latido. Un electrocardiograma puede mostrar si tienes arritmias, que son ritmos cardíacos irregulares. Entre ellas están la fibrilación auricular y el aleteo auricular.
- Ataque cardíaco. Un electrocardiograma puede diagnosticar un ataque cardíaco en curso o que ya hayas tenido. Los patrones en los resultados del electrocardiograma pueden ayudar a un profesional de atención médica a saber qué parte del corazón está dañada.
- Suministro de sangre y oxígeno al corazón. Un electrocardiograma realizado mientras ocurren los síntomas de dolor en el pecho puede ayudar al equipo de atención médica a saber si la causa es una reducción del flujo sanguíneo hacia el corazón.
- Cambios en la estructura cardíaca. Los resultados de un electrocardiograma pueden brindar indicios sobre un agrandamiento del corazón, defectos congénitos del corazón y otras afecciones cardíacas.
Si los resultados muestran un cambio en los latidos cardíacos, puede que necesites más pruebas. Por ejemplo, es posible que te realicen una ecografía del corazón, es decir, un ecocardiograma.
Estudios clínicos
Explora los estudios de Mayo Clinic de pruebas y procedimientos para ayudar a prevenir, detectar, tratar o controlar las afecciones.
Aug. 20, 2024