نظرة عامة
الورم النجمي
الورم النجمي
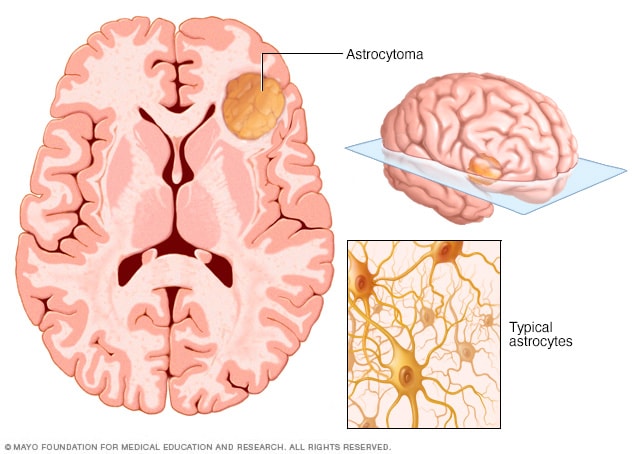
يُعد الورم النجمي نوعًا من السرطان يتكون في الدماغ أو الحبل النخاعي. ويبدأ الورم النجمي في خلايا تسمى الخلايا النجمية التي تدعم الخلايا العصبية. وبعض الأورام النجمية تنمو ببطء شديد وبعض آخر يمكن أن يكون سرطانات عدوانية تنمو سريعًا.
الورم النجمي أحد أنواع ورم الدماغ أو ورم الحبل النخاعي، وينشأ في خلايا تُسمى الخلايا النجمية. إذ تساعد هذه الخلايا نجمية الشكل في الحفاظ على سلامة الخلايا العصبية وعملها كما يجب.
تعتمد أعراض الورم النجمي على مكان نمو الورم. يمكن أن يسبب الورم النجمي في الدماغ نوبات صداع أو نوبات صرع أو غثيان أو تغيرات في المزاج أو السلوك. قد يسبب الورم النجمي في الحبل النخاعي ضعفًا أو صعوبة في تحريك الذراعين أو الساقين.
يمكن أن تتفاوت طبيعة الأورام النجمية بطرق مختلفة. إذ ينمو بعضها ببطء أكبر ويكون أقل عدوانية، في حين ينمو بعضها الآخر وينتشر بسرعة أكبر. غالبًا ما يختبر الأطباء جينات الورم أو سماته الجزيئية للمساعدة في اختيار أفضل علاج.
الورم النجمي جزءٌ من مجموعة أكبر من الأورام الدماغية تُسمى الأورام الدبقية. تنشأ هذه الأورام في الخلايا التي تساعد في دعم الخلايا العصبية. تُصنَّف درجات الأورام النجمية من الأولى إلى الرابعة بناءً على سرعة نموها. يُصنَّف الورم النجمي من الدرجة الرابعة، الذي يُسمى أيضًا الورم الأرومي الدبقي، على أنه الأسرع نموًا والأكثر عدوانية. عادة ما تنمو الأورام النجمية الأقل درجة، أي التي من الدرجة الأولى إلى الثالثة، ببطء أكبر. وتتسم في أغلب الأحيان بفرص نجاة أعلى مقارنة بالورم الأرومي الدبقي. يعتمد العلاج ومآل المرض على درجة الورم وحجمه وموقعه وسماته الجزيئية.
المنتجات والخدمات
الأعراض
غالبًا ما تكون أعراض الورم النجمي خفيفة في البداية. وتعتمد شدة الأعراض على مكان الورم في الدماغ أو الحبل النخاعي. يمكن أن تتغير أعراض ورم الدماغ هذه مع نمو الورم. تحدث الأعراض المبكرة نتيجة لحدوث التهاب في أنسجة محددة قريبة من الدماغ. تحدث الأعراض اللاحقة مع نمو ورم الدماغ وزيادة الضغط داخل الدماغ أو القناة النخاعية.
يمكن أن يزداد نمو الأورام النجمية منخفضة الدرجة أكثر قبل ظهور أعراضها، بينما قد تسبب أعراض أورام الدماغ عالية الدرجة ظهور الأعراض في وقت أبكر.
الأعراض المبكرة للإصابة بالورم النجمي
- الإصابة الحديثة بنوبات صرع، غالبًا ما تكون أول مؤشر للأورام بطيئة النمو.
- تغيرات طفيفة في التفكير أو المزاج أو الذاكرة.
- نوبات صداع خفيفة.
- صعوبة في استحضار الكلمات المناسبة للتعبير.
- تغيرات في الرؤية.
- كُلال في أحد جانبي الجسم.
- ألم في الرقبة أو الظهر يبدأ ببطء.
- وخز أو خَدَر ينتقل إلى إحدى الذراعين أو الساقين.
الأعراض اللاحقة للورم النجمي مع نمو الورم
- نوبات صداع تتفاقم، خصوصًا في الصباح أو مع السعال أو الإجهاد.
- الغثيان والقيء، اللذان قد يحدثان نتيجة لزيادة الضغط.
- زيادة الضعف.
- مشكلات في الكلام أو الرؤية.
- الانحدار الإدراكي، ويُقصد به التغيرات في الذاكرة أو التفكير أو التركيز.
- تفاقم مشكلة التوازن.
- تغيرات في حركة الأمعاء أو المثانة.
أعراض الورم النجمي حسب موقع الورم
قد ينشأ الورم النجمي في الدماغ أو الحبل النخاعي. غالبًا ما تبدو مؤشرات المرض والأعراض مختلفة وذلك حسب موقع الورم.
الجزء الخلفي والسفلي من الدماغ
- مشكلة في التوازن والتناسق الحركي مثل التعثر أو الحركات المرتعشة.
- الصداع والغثيان والقيء نتيجة للضغط الموجود في الدماغ.
جذع الدماغ
- ازدواج الرؤية أو مشكلات أخرى في حركة العين.
- ضعف الوجه أو عدم وجود إحساس بالوجه.
- صعوبة التحدث أو البلع.
- صعوبة المشي والاتزان.
- الضعف.
الحبل النخاعي
- ألم في الظهر أو الرقبة يتفاقم ببطء.
- ألم ينتشر في إحدى الذراعين أو الساقين.
- الخَدَر والوخز.
- الضعف.
- ضعف التوازن والسقوط وفقدان الثبات أثناء المشي.
- تغيرات في حركة الأمعاء أو المثانة قد تحدث في وقت لاحق.
لا تقتصر هذه الأعراض بالضرورة على الورم النجم؛ إذ قد تحدث مع الكثير من أنواع أورام الدماغ. يجب على اختصاصي الرعاية الصحية التحقق من الأعراض الجديدة أو الأعراض المتفاقمة. تشمل هذه الأعراض حدوث نوبة صرع لأول مرة أو تغيرات في الرؤية أو صعوبة في الكلام أو ضعف أو نوبات صداع في جانب واحد من الوجه وتتفاقم في الصباح.
هل يمكن أن تسبب الوذمة أو التورم تفاقم الأعراض؟
نعم. تشير الوذمة المحيطة بالورم إلى تورم أنسجة الدماغ الموجودة حول الورم. وقد تؤدي إلى تفاقم الأعراض أو ظهور أعراض جديدة. قد تشمل هذه الأعراض نوبات الصداع أو الضعف أو صعوبة في الكلام أو تغيرات في الرؤية. يؤدي التورم إلى زيادة الضغط داخل الجمجمة وقد يسبب تمديد مسارات الدماغ القريبة أو تهيُّجها. وقد يسبب ذلك بدوره تفاقم الأعراض الشائعة. يمكن استخدام أدوية ستيرويدية لفترات قصيرة لتقليل التورم وتخفيف الأعراض.
تحدث الوذمة بشكل أكبر في حالات الأورام النجمية عالية الدرجة وتسهم في ظهور الأعراض حتى إذا لم يكن الورم نفسه كبيرًا جدًا.
كيف تختلف أعراض الورم النجمي شعري الخلايا لدى الأطفال عن أعراضه لدى البالغين؟
الأورام النجمية شعرية الخلايا أحد أشكال الأورام النجمية الأكثر شيوعًا بين الأطفال والمراهقين. ويمكن أن يصاب البالغون بهذه الأورام، ولكنها نادرة الحدوث. نظرًا إلى أن الأورام النجمية شعرية الخلايا تنمو ببطء، عادة ما تتطور الأعراض تدريجيًا على مدار أسابيع أو أشهر.
قد يصاب الأطفال بالأعراض التالية:
- نوبات صداع، وخاصة في الصباح.
- مشكلات في الاتزان أو الكُلال إذا كان الورم في المخيخ.
- الغثيان أو القيء أو سهولة الاستثارة بسبب وجود ضغط في الدماغ.
- مشكلات في الرؤية إذا أثر الورم على المسار البصري.
بالنسبة إلى الأطفال في سن مبكرة، قد يلاحظ الأهل تغيرات في التناسق الحركي أو التحصيل الدراسي أو السلوك.
وبالنسبة إلى البالغين، من المرجح الإصابة بالأورام النجمية في منطقة مختلفة من الدماغ. قد تسبب هذه الأورام أعراضًا مبكرة، مثل الإصابة بنوبات صرع جديدة أو مشكلات في الكلام أو تغيرات في التفكير أو الشخصية.
نظام تصنيف الورم النجمي
تُصنَّف الأورام النجمية إلى درجات حسب كيفية ظهور الخلايا وسلوكها تحت المجهر. أنشأت منظمة الصحة العالمية (WHO) نظام التصنيف هذا للمساعدة في التنبؤ بمدى السرعة التي قد ينمو بها الورم أو ينتشر لتوجيه قرارات العلاج.
| الدرجة |
الاسم |
السلوك |
ملاحظات |
| 1 |
الورم النجمي شعري الخلايا |
أقل الأنواع عدوانية. ينمو ببطء وعادة ما تكون حوافه واضحة. |
غالبًا ما ينجح علاجه بالجراحة وحدها. يُصنَّف على أنه ورم حميد. يُعالَج معظم المصابين به بالجراحة ويعيشون حياة طبيعية. |
| 2 |
الورم النجمي المنتشر |
ينمو ببطء وفي أغلب الأحيان ينمو في أنسجة الدماغ القريبة، ما قد يجعل الاستئصال بالكامل أمرًا صعبًا. |
تبدو الخلايا مختلفة قليلاً عن الخلايا الطبيعية تحت المجهر. يتضمن العلاج عادة الجراحة لاستئصال أكبر قدر ممكن من الورم بأمان قدر الإمكان، ثم الإشعاع أو العلاج الكيميائي أو كليهما. يتراوح متوسط البقاء على قيد الحياة بين 7 و8 أعوام. |
| 3 |
الورم النجمي الكشمي |
عالي الدرجة. ينمو بشكل أسرع من الدرجة 2 ويتسم بخطورة أكبر. |
يتطلب علاجًا أكثر شدة. يتضمن العلاج عادة الجراحة لاستئصال أكبر قدر ممكن من الورم بأمان قدر الإمكان، ثم العلاج الإشعاعي والعلاج الكيميائي. يبلغ متوسط البقاء على قيد الحياة بوجه عام 5 أعوام أو أكثر حسب نوع الورم. |
| 4 |
الورم الأرومي الدبقي |
أكثر الأنواع عدوانية. يمكن أن ينشأ من ورم ذي درجة منخفضة أو يظهر في صورة مرض ذي درجة عالية. |
يكون أكثر شيوعًا بين البالغين. يبدأ العلاج عادة بالجراحة ثم العلاج الإشعاعي والعلاج الكيميائي. يبلغ متوسط البقاء على قيد الحياة نحو 15 شهرًا. |
مقارنة بين الأورام محددة الحواف والأورام المنتشرة
يُشار إلى بعض الأورام النجمية على أنها محددة الحواف، بينما تُصنَّف الأنواع الأخرى على أنها منتشرة. يُقصد بمحددة الحواف أن الورم ذو شكل محدد ومتمركز في منطقة معينة. في حين تنتقل الأورام النجمية المنتشرة إلى أنسجة الدماغ القريبة. تعمل الأورام النجمية محددة الحواف على تحديد نمط نمو الورم والفئة التي ينتمي إليها، لكنها لا تحدد الدرجة. يُصنَّف الورم النجمي متعدد الأشكال (PXA) وشعري الخلايا على أنه ورم محدد الحواف. ويُصنَّف بشكل منفصل عن الأورام النجمية المنتشرة.
الأورام المرتبطة بجين نازعة هيدروجين الإيزوسيترات
تُعرف نازعة هيدروجين الإيزوسيترات بأنها جين موجود داخل الخلايا. يوجد نوعان من هذا الجين: IDH1 وIDH2. إذا كان الورم عبارة عن نازعة هيدروجين الإيزوسيترات من النمط البري، فهذا يعني أن جين IDH يبدو سليمًا ولم تطرأ عليه أي تغيرات في خلايا الورم. الورم الأرومي الدبقي أحد أشكال الأورام التي تحتوي على جين نازعة هيدروجين الإيزوسيترات من النمط البري.
إذا كان الورم عبارة عن طفرة في جين نازعة هيدروجين الإيزوسيترات، فسيحدث تغير في جين IDH1 أو IDH2. وفقًا لنظام منظمة الصحة العالمية الحالي، إذا أظهرت الفحوصات المختبرية تغيرًا في IDH، فعندئذٍ يكون الورم نجميًا؛ أي ورمًا يحتوي على طفرة في جين نازعة هيدروجين الإيزوسيترات. وبحسب تسمية نوع الورم، تُصنَّف درجته، سواء أكانت من الدرجة الثانية أم الثالثة أم الرابعة، بناءً على مدى سرعة نموه. يساعد اختبار نازعة هيدروجين الإيزوسيترات فريق الرعاية الصحية في تصنيف الورم والتنبؤ بسلوكه.
متى تجب زيارة الطبيب
حدِّد موعدًا لزيارة اختصاصي الرعاية الصحية إذا شعرت بأعراض مستمرة مثيرة للقلق.
الأسباب
غالبًا لا يتضح السبب الدقيق للورم النجمي، الذي يُعرف بأنه نوع من الأورام التي تصيب الدماغ أو الحبل النخاعي. ينشأ هذا النوع من الورم عندما يبدأ نمو الخلايا النجمية، وهي خلايا موجودة في الدماغ أو الحبل النخاعي، وانقسامها بطريقة غير طبيعية لا يمكن السيطرة عليها. تدعم الخلايا النجمية عادة الخلايا الموجودة في الدماغ والحبل النخاعي وتحميها.
يحدث الورم النجمي عند حدوث تغيرات في الحمض النووي للخلايا النجمية. يحمل حمض الخلية النووي تعليمات توجِّه الخلية إلى أداء وظيفتها. في الخلايا السليمة، يعطي الحمض النووي تعليمات بالنمو والتكاثر بمعدل ثابت. وتدفع التعليمات الخلايا إلى الموت في وقت محدد.
في خلايا الأورام، تؤدي التغيرات في الحمض النووي إلى إعطاء تعليمات مختلفة للخلايا. تُسمى هذه التغيرات الجينية طفرات. يمكن أن تسبب هذه الطفرات الإصابة بالورم النجمي من خلال التأثير على مدى تحكم الخلايا في النمو وإصلاح التلف. يسبب حدوث تغيرات جينية انقسام الخلايا في غير أوانها وبقاءها حية لفترة أطول من الطبيعي. يؤدي ذلك بدوره إلى تجمُّع عدد كبير جدًا من الخلايا معًا مسببة الورم.
ومع نمو الورم، يمكن أن يضغط على الأجزاء القريبة منه في الدماغ أو الحبل النخاعي. وفي بعض الأحيان، تؤدي التغيرات في الحمض النووي إلى تحويل خلايا الورم إلى خلايا سرطانية. ويمكن أن تغزو الخلايا السرطانية أنسجة الجسم السليمة وتدمرها.
اكتشف العلماء أن حدوث تغيرات جينية معينة داخل الورم يحفز هذا النمو غير الصحي لخلايا الورم النجمي بحيث:
- تؤثر التغيرات في جينات IDH1 وIDH2 على كيفية إنتاج واستخدام خلايا الورم للطاقة. تشيع هذه التغيرات في العديد من الأورام النجمية منخفضة الدرجة.
- تؤثر التغيرات في جينات TP53 وATRX على كيفية إصلاح الخلايا للحمض النووي وكيفية إدارة نمو الخلايا.
- يؤثر إسكات جين MGMT على كيفية إصلاح خلايا الورم لتلف الحمض النووي، كما يمكن أن يؤثر على مدى فعالية العلاج.
- بالنسبة إلى الأطفال، غالبًا ما تظهر التغيرات في جين BRAF في الأورام النجمية شعرية الخلايا، وتُعرف بأنها أورام الدماغ بطيئة النمو. تحدث هذه التغيرات الجينية داخل الورم ولا تنتقل عادة بالوراثة بين الأجيال.
تحدث الأورام النجمية شعرية الخلايا بسبب تعطل إشارة النمو في الخلايا في حالة "التنشيط المستمر". يسبب ذلك نمو الخلايا ببطء في منطقة واحدة. تحدث الأورام النجمية عالية الدرجة بعد تراكم الكثير من التغيرات الضارة في الحمض النووي. ويسبب ذلك نمو الخلايا بصورة أسرع وانتشارها إلى أنسجة الدماغ القريبة.
عوامل الخطورة
تتضمن عوامل خطر الإصابة بالورم النجمي ما يلي:
- وجود سيرة مرضية للخضوع لجرعة عالية من العلاج بالإشعاع المؤيِّن على الرأس أو الرقبة. إذا خضعتَ لجرعة عالية من الإشعاع في علاج نوع آخر من السرطان، فقد يزداد خطر الإصابة. وينطبق ذلك إذا كان الإشعاع قريبًا من الرأس أو الرقبة وخاصة في مرحلة الطفولة.
- العمر. يمكن أن تصيب الأورام النجمية كلاً من الأطفال والبالغين. غالبًا ما تصيب الأورام منخفضة الدرجة الأطفال؛ حيث تميل إلى النمو ببطء. بينما تصيب الأورام عالية الدرجة البالغين في الغالب؛ حيث تنمو بصورة أسرع ويكون سلوكها أكثر عدوانية. تُشخَّص أغلب الأورام النجمية عالية الدرجة في الفئة العمرية التي تزيد على 40 عامًا.
- الحالات الوراثية. قد تؤدي الإصابة بحالات نادرة معينة تسري في العائلات، مثل الورام الليفي العصبي من النوع الأول (NF1)، ومتلازمة لينش، ومتلازمة تركو والتصلب الحدبي، إلى زيادة خطر الإصابة.
هل يمكن أن يؤدي نمط الحياة أو البيئة إلى الإصابة بالورم النجمي؟
لا توجد علاقة مثبتة بين عوامل نمط الحياة، مثل الحمية الغذائية أو ممارسة التمارين الرياضية أو التدخين، والإصابة بالورم النجمي. لم يتضح أن المخاطر البيئية الأخرى المشتبه فيها، مثل التعرض للمواد الكيميائية أو استخدام الهاتف الخلوي، تسبب الإصابة بالورم النجمي. تظهر معظم الحالات بالصدفة، من دون أي محفز خارجي.
لا توجد طريقة معروفة للوقاية من الإصابة بالورم النجمي.
المضاعفات
يمكن أن تسبب الأورام النجمية مضاعفات أثناء نمو الورم أو كنتيجة للعلاج. تتضمن مضاعفات الورم النجمي المحتملة ما يلي:
- مشكلات عصبية. قد يضغط الورم على أجزاء في الدماغ أو الحبل النخاعي. يمكن أن يؤدي ذلك إلى حدوث نوبات صداع أو نوبات صرع أو صعوبة في الكلام أو ضعف أو صعوبة في المشي.
- انتكاس الورم. يمكن أن تعاود الأورام النجمية الظهور حتى بعد العلاج، خصوصًا إذا كانت متقدمة أو لم يكن بالإمكان استئصالها بالكامل.
- مخاطر العلاج وآثاره الجانبية. في بعض الأحيان، يمكن أن تسبب الجراحة والعلاج الإشعاعي والكيميائي آثارًا جانبية مثل مشكلة في الذاكرة أو التفكير أو نوبات صرع أو نوبات صداع أو غثيان أو إرهاق. في بعض الحالات، قد يسبب العلاج تضرر أنسجة الدماغ السليمة.
يتعاون فريق الرعاية معك للمساعدة في إدارة هذه المشكلات ودعم جودة الحياة.