Descripción general
Astrocitoma
Astrocitoma
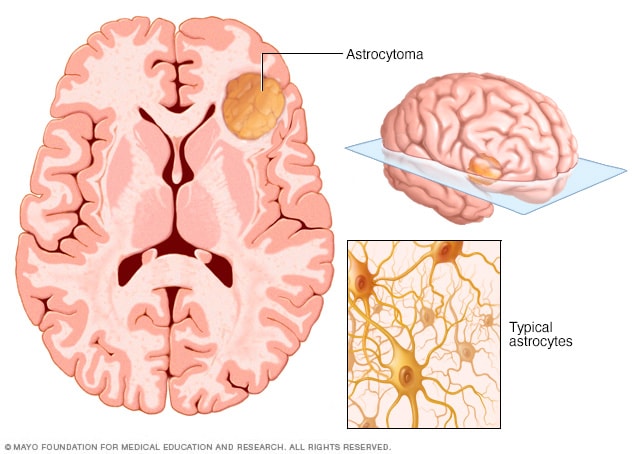
El astrocitoma es un tipo de cáncer que puede ocurrir en el cerebro o en la médula espinal. Comienza en las células llamadas astrocitos que brindan sostén a las células nerviosas. Algunos astrocitomas crecen muy lentamente y otros pueden ser cánceres agresivos que crecen rápidamente.
El astrocitoma es una proliferación de células que comienza en el cerebro o la médula espinal. La protuberancia, que se denomina tumor, se inicia en unas células llamadas astrocitos. Los astrocitos sostienen y conectan las células nerviosas del cerebro y la médula espinal.
Los síntomas del astrocitoma varían en función de dónde se encuentre el tumor. Un astrocitoma en el cerebro puede causar cambios de personalidad, convulsiones, dolores de cabeza y náuseas. Un astrocitoma en la médula espinal puede causar debilidad y discapacidad en la zona afectada por el tumor en desarrollo.
Algunos astrocitomas se multiplican lentamente. Estos no se consideran cancerosos. Los tumores no cancerosos a veces se llaman astrocitomas benignos. La mayoría de los astrocitomas se multiplican rápidamente y se consideran como cáncer cerebral. También se conocen como astrocitomas malignos. Que el tumor sea benigno o maligno es uno de los factores que el equipo de atención médica tiene en cuenta a la hora de elaborar un plan de tratamiento.
Productos y servicios
Síntomas
Los signos y síntomas del astrocitoma pueden variar según el lugar en el que surja el tumor. Este tumor puede aparecer en el cerebro o en la médula espinal.
Entre los síntomas de astrocitomas en el cerebro, se incluyen los siguientes:
- Convulsiones, que pueden causar pérdida del conocimiento o cambios en el comportamiento, como quedarse mirando a la nada.
- Dolores de cabeza.
- Náuseas y vómitos.
- Cambios en la personalidad.
- Problemas para hablar.
- Mucho cansancio o mucha debilidad.
Entre los síntomas de astrocitomas en la médula espinal, se incluyen los siguientes:
- Dolor en el área afectada.
- Dolor que empeora por la noche.
- Debilidad en los brazos o piernas que empeora con el tiempo.
- Problemas para caminar.
Early symptoms of astrocytoma
- New seizures, which are often the first sign in slow-growing tumors.
- Subtle changes in thinking, mood or memory.
- Mild headaches.
- Difficulty finding the right words to say.
- Changes in vision.
- Clumsiness on one side of the body.
- Pain in the neck or back that begins slowly.
- Tingling or numbness that travels into an arm or leg.
Later symptoms of astrocytoma as the tumor grows
- Headaches that get worse, especially in the morning or with coughing or straining.
- Nausea and vomiting, which can happen as a result of increased pressure.
- Increasing weakness.
- Speech or vision troubles.
- Changes in memory, thinking or concentration, called cognitive decline.
- Worsening balance.
- Bowel or bladder changes.
Astrocytoma symptoms by tumor location
An astrocytoma may start in the brain or the spinal cord. The signs and symptoms often look different depending on the location of the tumor.
Back and lower part of brain
- Trouble with balance and coordination such as stumbling or shaky movements.
- Headache, nausea and vomiting from pressure in the brain.
Brainstem
- Double vision or other eye movement issues.
- Facial weakness or lack of feeling in the face.
- Difficulty speaking or swallowing.
- Difficulty with walking and balance.
- Weakness.
Spinal cord
- Back or neck pain that slowly gets worse.
- Pain that spreads into an arm or leg.
- Numbness and tingling.
- Weakness.
- Poor balance, falls and unsteadiness when walking.
- Bowel or bladder changes that may occur later.
These symptoms aren't necessarily specific to astrocytoma but can happen with many types of brain tumors. New symptoms or symptoms that get worse should be checked by your healthcare professional. These symptoms include a first-time seizure, vision changes, speech trouble, one-sided weakness or headaches that are worse in the morning.
Can swelling, called edema, around the tumor worsen symptoms?
Yes. Swelling of brain tissue around the tumor is called peritumoral edema. It can make symptoms worse or cause new symptoms to appear. These symptoms may include headaches, weakness, speech trouble or vision changes. The swelling increases pressure inside the skull and can stretch or irritate nearby brain pathways. This may worsen common symptoms. Short courses of steroid medicines may be used to reduce swelling and relieve symptoms.
Edema is more common in high-grade astrocytomas and contributes to symptoms even when the tumor itself is not very large.
How do children's symptoms of pilocytic astrocytoma differ from adult symptoms?
Pilocytic astrocytomas are a type of astrocytoma that are more common in children and teens. Adults can have these tumors, but it is rare. Because pilocytic astrocytomas grow slowly, symptoms often develop gradually over weeks or months.
Children may have:
- Headaches, especially in the morning.
- Balance problems or clumsiness if the tumor is in the cerebellum.
- Nausea, vomiting or irritability from pressure in the brain.
- Vision problems if the tumor affects the optic pathway.
In very young children, parents may notice changes in coordination, school performance or behavior.
In adults, astrocytomas are more likely to develop in a different part of the brain. They may cause new seizures, speech issues, or changes in thinking or personality as early symptoms.
Astrocytoma grading system
Astrocytomas are sorted into grades depending on how their cells appear and act under a microscope. The World Health Organization (WHO) created this grading system to help predict how quickly the tumor might grow or spread and to guide treatment decisions.
| Grade |
Name |
How it behaves |
Notes |
| 1 |
Pilocytic astrocytoma |
Least aggressive. Grows slowly and usually has clear edges. |
Often treated successfully with surgery alone. It's considered nonmalignant (benign). Most people are cured with surgery and live a typical lifespan. |
| 2 |
Diffuse astrocytoma |
Slow growing but often grows into nearby brain tissue, which can make complete removal difficult. |
Cells look only slightly different from typical under the microscope. Treatment usually involves surgery to remove as much of the tumor as safely possible followed by radiation or chemotherapy or both. Median survival is between 7 and 8 years. |
| 3 |
Anaplastic astrocytoma |
High-grade. Grows faster than grade 2 and is more serious. |
Requires more aggressive treatment. Treatment usually involves surgery to remove as much tumor as safely possible, followed by radiation therapy and chemotherapy. Overall median survival is about 5 years or longer depending on the tumor type. |
| 4 |
Glioblastoma |
Most aggressive. Can arise from a lower grade tumor or appear suddenly as high-grade disease. |
Most common in adults. Treatment is usually surgery followed by radiation and chemotherapy. Median survival is around 15 months. |
Circumscribed versus diffuse tumors
Some astrocytomas are called circumscribed, and others are called diffuse. Circumscribed means the tumor is well defined and localized. Diffuse astrocytomas spread into nearby brain tissue. Circumscribed defines the growth pattern and the category of the tumor, but not the grade. Pilocytic and pleomorphic xanthoastrocytoma (PXA) are circumscribed tumors. These are grouped separately from diffuse astrocytomas.
IDH tumors
IDH is a gene found in cells. There are two: IDH1 and IDH2. When a tumor is IDH wild type, it means the IDH gene looks healthy and there's no change to the IDH gene in the tumor cells. Glioblastoma is an IDH wild-type tumor.
When a tumor is IDH mutant, there is a change in the IDH1 or IDH2 gene. In the current WHO system, if lab tests show an IDH change, the tumor is named astrocytoma, IDH mutant. After naming the type, a grade is assigned — 2, 3 or 4 — based on how fast it's likely to grow. IDH testing helps the healthcare team classify the tumor and predict how it may behave.
Cuándo debes consultar a un médico
Programa una cita con un médico u otro profesional de atención médica si tienes síntomas continuos que te preocupan.
Causas
La causa del astrocitoma a menudo es desconocida. El tumor comienza con la proliferación de células en el cerebro o en la médula espinal. Se forma en células llamadas astrocitos. Los astrocitos sostienen y conectan las células nerviosas del cerebro y la médula espinal.
Un astrocitoma ocurre cuando los astrocitos presentan cambios en el ADN. El ADN de una célula contiene las instrucciones que le indican lo que debe hacer. En las células sanas, el ADN da las instrucciones para que crezcan y se multipliquen a un determinado ritmo. Las instrucciones les indican a las células que deben morir en un momento determinado. En el caso de las células tumorales, los cambios en el ADN hacen que las instrucciones sean diferentes; Los cambios indican a las células tumorales que proliferen y se multipliquen rápidamente. De este modo, las células tumorales siguen viviendo mientras que las sanas mueren. Esto causa un exceso de células.
Las células tumorales forman una proliferación que genera presión en partes cercanas del cerebro o la médula espinal a medida que crece. A veces, los cambios en el ADN generan que las células tumorales se conviertan en células cancerosas. Las células cancerosas pueden invadir y destruir los tejidos sanos del cuerpo.
Factores de riesgo
Entre los factores de riesgo del astrocitoma, se incluyen los siguientes:
- Antecedentes de radioterapia: Si recibiste tratamientos de radiación por otro tipo de cáncer, en especial cerca de la cabeza o cuello, puede que tengas más riesgo.
- Edad mediana: El astrocitoma puede ocurrir a cualquier edad, pero es más común en los adultos entre 30 y 55 años.
- Síndromes hereditarios: Las personas que tienen algunos trastornos en sus antecedentes familiares tienen más posibilidades de padecer astrocitoma. Algunos ejemplos son la neurofibromatosis de tipo 1, el síndrome de Lynch y el síndrome de Li-Fraumeni.
No hay manera de prevenir el astrocitoma.
Could lifestyle or the environment cause astrocytoma?
There's no proven link between lifestyle factors, such as diet, exercise or smoking, and astrocytoma. Other suspected environmental risks, such as chemical exposures or cellphone use, have not been shown to cause astrocytoma. Most cases appear by chance, without a clear outside trigger.
There is no known way to prevent astrocytoma.
Complicaciones
Astrocytomas can cause complications as the tumor grows or as a result of treatment. Possible astrocytoma complications include:
- Neurological issues. The tumor may press on parts of the brain or spinal cord. This can lead to headaches, seizures, trouble speaking, weakness or difficulty walking.
- Tumor recurrence. Even after treatment, astrocytomas may come back, especially if they are high grade or could not be fully removed.
- Treatment risks and side effects. Surgery, radiation and chemotherapy sometimes can cause side effects such as trouble with memory or thinking, seizures, headaches, nausea, or fatigue. In some cases, treatment may damage healthy brain tissue.
Your care team works with you to help manage these issues and support your quality of life.
Nov. 07, 2025