Overview
Person with acromegaly
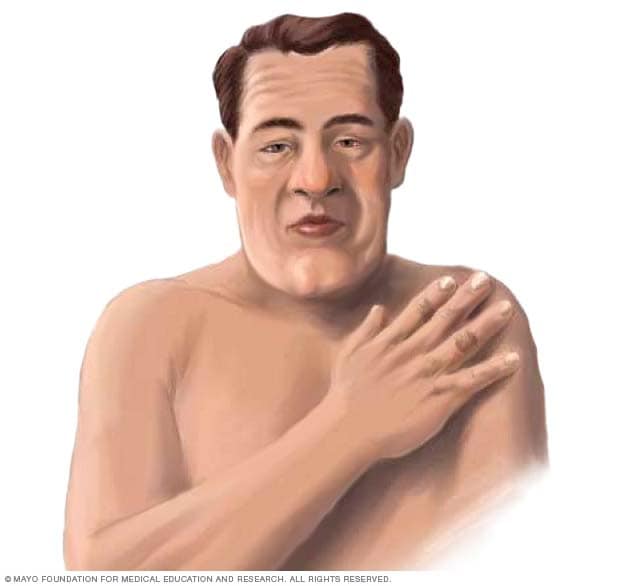
Person with acromegaly
Symptoms of acromegaly include an enlarged face and hands. Changes to the face may cause the brow bone and lower jaw to jut out. And the nose and lips may get larger.
Acromegaly is a rare hormonal condition in adults that causes some bones, organs and other tissues to grow bigger. A small gland in the brain called the pituitary gland drives these changes by making too much growth hormone (GH). High GH levels increase another hormone called insulin-like growth factor-1 (IGF-1). This usually happens due to a noncancerous, also called benign, pituitary tumor.
When the body has too much growth hormone, bones get bigger. In childhood, this leads to increased height as part of a condition called gigantism. In adults with acromegaly, a change in height doesn't happen. Instead, bones in the hands, feet and face become bigger. Other changes may include joint pain, thickened skin, and facial changes such as a bigger jaw or nose.
These changes happen slowly over many years. So people with acromegaly and their loved ones may not notice the symptoms right away. It may take a long time to see changes. And healthcare professionals may have a hard time finding and treating the condition early on.
Acromegaly is a rare hormonal condition. Fewer than 15 people per 100,000 are living with acromegaly. Each year, about 3 to 5 people out of every million people are diagnosed with acromegaly. Because the condition develops slowly and diagnosis is often delayed, the true number of cases may be a little higher.
Without treatment, acromegaly can lead to other serious and sometimes life-threatening complications. But treatments such as surgery, medicine and radiation can lower the risk of complications and improve many acromegaly symptoms. With treatment, many people with acromegaly can live a healthy life with a life expectancy close to that of people without acromegaly.
Products & Services
Symptoms
Acromegaly symptoms can change the way some body parts look. Common visible changes can include:
- Thick ears and lips.
- A broad nose.
- Enlarged hands and feet.
- A jutting brow or jaw.
- Gaps between teeth.
- An enlarged tongue.
- An expanded rib cage that may cause the chest to have a round shape.
Skin changes in acromegaly may include acne, skin tags, thickened or oily skin, and swelling under the skin.
Most often, people with acromegaly don't have every possible body change. And because the changes come on slowly, they may take years to notice.
How does acromegaly affect the body?
Beyond visible changes, too much GH and IGF-1 affect many organs and systems. Specific effects include:
- Dental health. Acromegaly can cause an unusually large jaw and spacing between the teeth. People may notice gaps forming between teeth, bite changes or teeth that don't line up correctly. The tongue also may enlarge, leading to speech and breathing problems. Regular dental care is important for managing these oral changes.
- Reproductive and sexual health. Excess growth hormone can affect reproductive health. In men, acromegaly may lead to erectile dysfunction, reduced libido and low testosterone. Enlargement of soft tissues also may occur, but sexual issues are usually due to hormonal imbalance rather than physical enlargement.
- Voice changes. Thickening of tissues in the vocal cords and throat can make the voice deeper or hoarser over time. Some people also notice snoring or changes in speech.
Early symptoms of acromegaly may be subtle, such as changes in ring or shoe size. As the condition progresses, other common symptoms can include:
- Vision troubles, including loss of side vision.
- More sweating and body odor than is typical.
- Fatigue and low energy.
- Headaches.
- Joint pain.
- Sleep problems, including sleep apnea.
What is the difference between acromegaly and other conditions?
Acromegaly is a rare hormonal condition in adults that happens when there is too much growth hormone (GH) and insulin-like growth factor-1 (IGF-1). Acromegaly is usually caused by a noncancerous, also called benign, pituitary tumor. It leads to enlarged hands, feet and facial features, joint pain, and serious complications if it's not treated. Several other conditions may look similar to acromegaly, but the causes and symptoms are different.
Acromegaly vs. gigantism
- Gigantism happens when too much growth hormone is produced before puberty while the bones are still growing.
- Children with gigantism grow unusually tall, with very long arms and legs.
- Acromegaly develops after puberty, when the growth plates are closed. It causes changes in hands, feet and facial bones, but not extreme height.
Acromegaly vs. Cushing disease
- Cushing disease is caused by too much cortisol. Cortisol is another pituitary hormone. The extra cortisol changes where fat is stored.
- Symptoms include weight gain in the face and trunk, a hump on the back from the redistributed fat storage, easy bruising and diabetes.
- Acromegaly is caused by too much of the GH and IGF-1 hormones and leads to bone and tissue overgrowth, not fat redistribution.
Acromegaly vs. Marfan syndrome
- Marfan syndrome is a genetic condition that affects connective tissue.
- People with Marfan syndrome are tall and thin with long arms, legs and fingers, and heart or eye conditions.
- Acromegaly develops later in life and does not cause the long, slender build of Marfan syndrome.
Acromegaly vs. Paget's disease of bone
- Paget's disease is a condition where bones break down and regrow in an unusual way, becoming weak and misshapen.
- It can cause skull enlargement, bent legs or bone pain.
- Unlike Paget's disease of bone, acromegaly also causes soft tissue swelling, enlarged hands and feet, and metabolic complications such as diabetes, high blood pressure, high cholesterol and sleep apnea.
Acromegaly vs. achondroplasia
- Achondroplasia is the most common form of dwarfism. It is caused by a gene change that affects bone growth.
- People with achondroplasia have short stature, short arms and legs, and an average-sized trunk.
- Acromegaly does not cause short stature. Instead, it causes enlargement of features after typical growth is complete.
Acromegaly vs. Weaver syndrome
- Weaver syndrome is a very rare condition present from birth that causes rapid growth, advanced bone age and developmental delays. Weaver syndrome is caused by a change in a gene and is passed down from a parent to a child.
- Babies and children with Weaver syndrome are tall and large for their age.
- Acromegaly develops in adulthood and is not caused by a gene change.
When to see a doctor
Get a healthcare checkup if you think you have symptoms of acromegaly. The condition usually develops slowly. Even family members may take a long time to notice the physical changes that happen. But it's important for a healthcare professional to find the condition as early as possible. Treatment can help prevent serious health conditions that can happen along with acromegaly.
Causes
Pituitary gland and hypothalamus
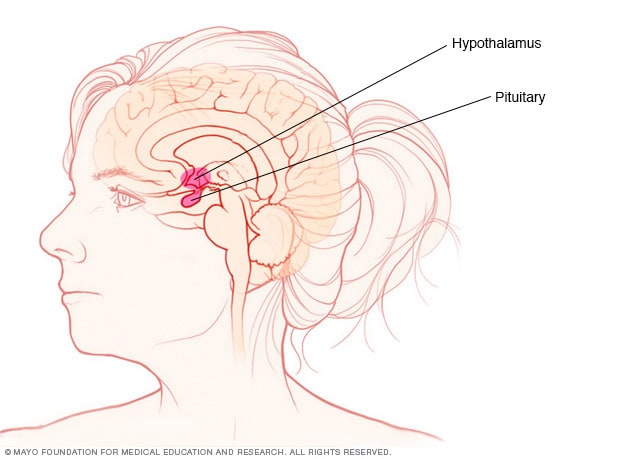
Pituitary gland and hypothalamus
The pituitary gland and the hypothalamus are in the brain. They make hormones that control many important functions in the body.
The most common cause of acromegaly is a noncancerous tumor in the pituitary gland, called an adenoma. An adenoma makes too much growth hormone over a long amount of time.
Too much growth hormone causes many symptoms of acromegaly. Some of the symptoms, such as headaches and impaired vision, are due to the tumor pressing on nearby brain tissues.
Rarely, tumors in other parts of the body cause acromegaly. These include tumors of the lung or pancreas. Sometimes these tumors release growth hormone. Or they make a hormone called growth hormone-releasing hormone. This signals the pituitary gland to make more growth hormone.
The pituitary gland is located at the base of the brain, behind the bridge of the nose. It makes growth hormone and other hormones. Growth hormone plays an important role in controlling physical growth.
The pituitary gland releases growth hormone into the bloodstream. This triggers the liver to make a hormone called insulin-like growth factor-1 (IGF-1). IGF-1 is what causes bones and other tissues to grow. Too much growth hormone leads to too much IGF-1. And that can cause acromegaly symptoms and complications.
What is the relationship between pituitary tumors and acromegaly?
Acromegaly is almost always caused by a pituitary adenoma, which is a noncancerous tumor that develops in the pituitary gland. Pituitary adenomas are the most common type of pituitary tumor. Pituitary adenomas and other tumors are types of skull base tumors.
The pituitary gland contains different types of hormone-producing cells, including somatotroph cells. Somatotroph cells make growth hormone (GH). When a tumor grows from the somatotroph cells, it can release too much GH. Extra GH causes the liver to make more insulin-like growth factor 1 (IGF-1). This leads to the body changes seen in acromegaly such as enlarged hands, feet and facial features. Only somatotroph adenomas, sometimes called GH-secreting adenomas, cause acromegaly.
Other types of pituitary adenomas come from different hormone-producing cells, but these do not cause acromegaly:
- Lactotroph adenomas make prolactin and can cause issues such as irregular periods and difficulty getting pregnant.
- Corticotroph adenomas make adrenocorticotropic hormone (ACTH). Too much ACTH causes the adrenal glands to release extra cortisol, which can lead to Cushing disease.
- Thyrotroph adenomas make thyroid-stimulating hormone (TSH) and can lead to hyperthyroidism.
- Gonadotroph adenomas usually do not make excess hormone. But as they grow, gonadotroph adenomas can press on nearby tissues and cause symptoms such as headaches, vision problems, low energy, or changes in sexual and reproductive health.
Risk factors
The main known risk factor for acromegaly is a rare inherited condition called multiple endocrine neoplasia, type 1 (MEN1). In MEN1, tumors can form in the parathyroid glands, pancreas and pituitary gland. These tumors release extra hormones. Too much parathyroid hormone can weaken bones and cause kidney stones. A pancreas tumor may release insulin and cause low blood sugar. If a pituitary tumor makes excess growth hormone, acromegaly can result.
Very rarely, acromegaly also can run in families. This may occur in conditions such as familial isolated pituitary adenoma (FIPA), which increases the chance of pituitary tumors.
Outside of these rare inherited syndromes, most people with acromegaly have no known risk factors.
Complications
Without treatment, acromegaly can lead to complications, including:
Heart and blood vessel complications
Cancer and conditions that can lead to cancer
- Higher risk of some cancers, including prostate, breast, colon, thyroid and stomach cancer.
- Growths called polyps on the lining of the colon. Without treatment, these growths can lead to colon cancer.
Sexual health, reproductive health and pregnancy concerns
Metabolic problems
Bone, joint and nerve conditions
Other complications
- Sleep apnea, which is a condition where breathing repeatedly stops and starts during sleep.
- Changes in the thyroid gland, called a goiter.
- Vision changes or vision loss if the tumor presses on the optic nerves.
- Depression (major depressive disorder), fatigue and reduced quality of life.
Early treatment of acromegaly can prevent these complications or keep them from becoming worse. Without treatment, acromegaly and its complications can shorten life expectancy.
Oct. 22, 2025