Overview
Pituitary tumor
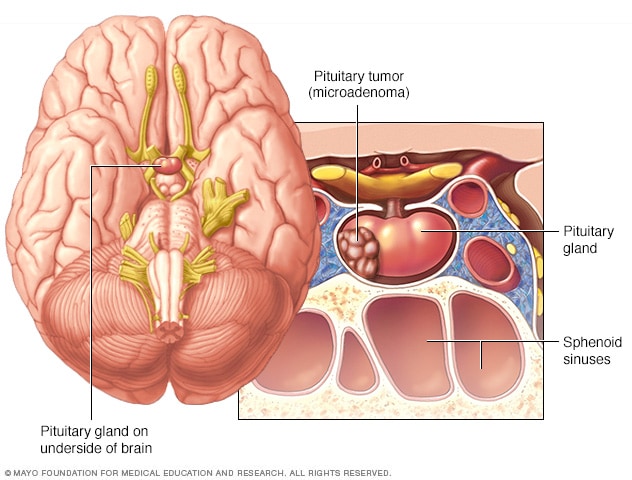
Pituitary tumor
Pituitary tumors are tumors that form in the pituitary gland near the brain. These tumors can cause changes in hormone levels. This illustration shows a smaller tumor, called a microadenoma.
Pituitary tumors are growths that form in the pituitary gland. This small, pea-sized gland is located behind the nose at the base of the brain. It makes hormones that help control many important body functions. Some pituitary tumors cause the pituitary gland to make too many hormones. Others cause it to make too few.
The pituitary is known as the master gland. That's because it sends chemical messages that tell other glands in the body when to start or stop making their hormones. In that way, it helps coordinate growth, metabolism, stress response and reproduction. But another part of the brain called the hypothalamus helps direct the pituitary. The hypothalamus monitors hormone levels and sends signals to keep them steady.
Most pituitary tumors are not cancer. These are called benign pituitary tumors. These noncancerous tumors also are called pituitary adenomas or pituitary neuroendocrine tumors. Most adenomas stay in the pituitary gland or the nearby tissue around it, and they grow slowly. They do not spread to other parts of the body.
A very small number of these tumors have changes in the cells that affect how they are built and how quickly they divide. Tumors with those cell changes can make the tumor grow faster, invade nearby areas or come back after treatment. These are called aggressive pituitary tumors. More rarely, a pituitary tumor may spread to other parts of the body. When this happens, it is called pituitary cancer. There are no clear risk factors that determine whether a pituitary tumor is likely to become aggressive or cancerous.
Pituitary tumors can be treated in several ways. The tumor may be removed with brain tumor surgery. Or its growth may be controlled with medicines or radiation therapy. Medicines also may help manage hormone levels. Your healthcare professional may suggest a combination of these treatments. And sometimes, the best plan is to carefully watch the tumor over time, using a watchful waiting approach.
Types
Types of pituitary adenomas include:
- Functioning. These tumors make hormones. They cause different symptoms based on which hormones they make. Functioning pituitary tumors are grouped into categories by the hormones they produce, including:
- Adrenocorticotropic hormone (ACTH). Tumors that produce ACTH are called corticotroph adenomas.
- Growth hormone. These tumors are called somatotroph adenomas.
- Luteinizing hormone and follicle-stimulating hormone. These hormones are known as gonadotropins. Pituitary tumors that make these hormones are called gonadotroph adenomas.
- Prolactin. These tumors are called prolactinomas or lactotroph adenomas.
- Thyroid-stimulating hormone. These tumors are called thyrotroph adenomas.
- Nonfunctioning. These tumors don't make hormones. Instead, the symptoms they cause come from their size. As they grow, they can press on the pituitary gland, the nearby nerves or the brain.
- Macroadenomas. These are larger adenomas. They are 1 centimeter or more in size. They can be functioning or nonfunctioning.
- Microadenomas. These adenomas are smaller. They are less than 1 centimeter in size. Like macroadenomas, they can be functioning or nonfunctioning.
Pituitary tumors are different from pituitary cysts. A cyst is a sac filled with fluid that may form on or near the pituitary gland. Occasionally, the amount of fluid can increase causing the cyst to enlarge over time. Pituitary cysts may or may not require treatment.
Products & Services
Symptoms
Not all pituitary tumors cause symptoms. Sometimes these tumors are found during an imaging test, such as a brain MRI or a brain CT, that was done for another reason. If they don't cause symptoms, pituitary tumors usually don't need treatment.
Pituitary tumor symptoms can happen when a tumor presses on the brain or nearby areas. Symptoms also can be caused by a hormone imbalance. Hormone levels can rise when a pituitary tumor makes too much of certain hormones. Or hormone levels can drop if a large tumor stops the pituitary gland from working the way it should.
Symptoms from tumor pressure
Large pituitary tumors, called macroadenomas, can press on the pituitary gland, nerves, the brain or other parts of the body nearby. This can cause symptoms such as:
- Headache.
- Vision issues, especially loss of side vision and double vision.
- Facial numbness or pain.
- Drooping eyelid.
- Seizures.
Dizziness isn't a typical symptom of a pituitary tumor, but it can happen. Low cortisol from pituitary hormone deficiency can cause low blood pressure, which can make you feel lightheaded. Some medicines used to treat pituitary tumors can cause dizziness when standing.
Symptoms from hormone changes
Cushing syndrome
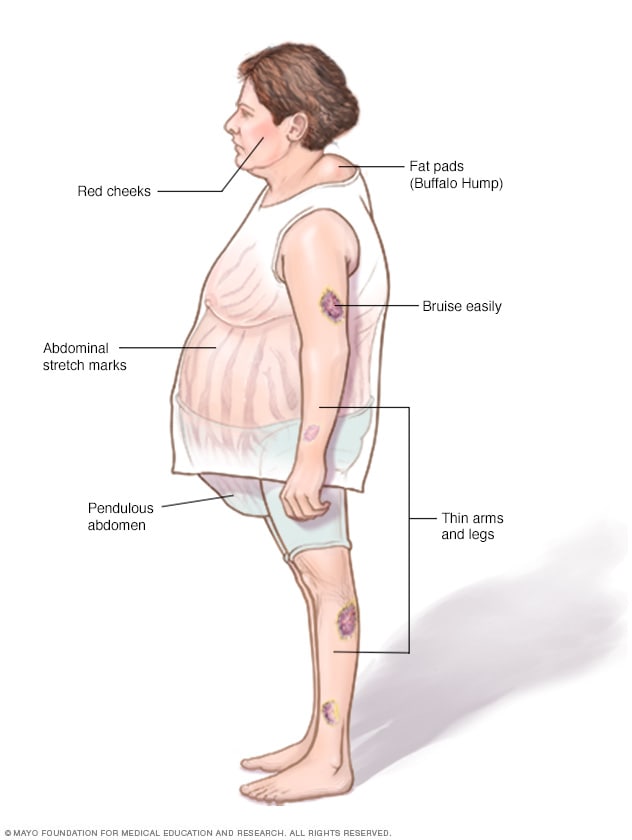
Cushing syndrome
Left untreated, Cushing syndrome can result in a rounded face, weight gain around the belly and upper back, thinner arms and legs, easy bruising, and stretch marks.
Person with acromegaly
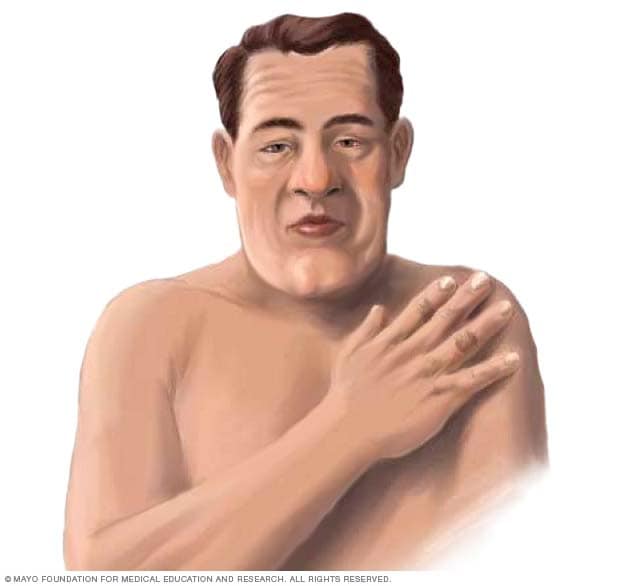
Person with acromegaly
Symptoms of acromegaly include an enlarged face and hands. Facial changes may include a more prominent brow and lower jaw, along with a larger nose and lips.
- Low amounts of hormones. Large pituitary tumors can make it harder for the pituitary gland to make hormones. When that happens, symptoms may include:
- Tiredness or weakness.
- Low energy.
- Loss of body hair.
- Sexual issues, such as difficulty with erections or less interest in sex.
- Changes in menstrual cycles.
- Feeling cold.
- Losing or gaining weight without trying.
- High amounts of hormones. Most pituitary tumors that make hormones produce too much of just one hormone. This can raise the level of that hormone in the body and cause symptoms. In rare cases, a pituitary tumor may make more than one hormone. The following types of functioning pituitary adenomas cause different symptoms depending on the hormones they make.
-
Pituitary tumors that make adrenocorticotropic hormone. Pituitary tumors that make adrenocorticotropic hormone (ACTH) are called corticotroph adenomas. ACTH causes the adrenal glands to make a hormone called cortisol. When a tumor makes too much ACTH, the adrenal glands make too much cortisol. This causes a condition called Cushing disease. Cushing disease is one cause of a broader condition called Cushing syndrome.
Cushing disease symptoms include:
- Weight gain and fatty tissue deposits around the belly, chest and upper back.
- A rounded face.
- Stretch marks.
- Depression or anxiety.
- Thin skin that bruises easily.
- Thinning of the arms and legs with muscle weakness.
- Thicker or more visible body hair.
- Slow healing of cuts, insect bites and infections.
- Areas of darkened skin.
- Acne.
- Changes in menstrual cycles.
- Sexual issues, such as difficulty with erections and less interest in sex.
-
Pituitary tumors that make growth hormone. Some pituitary tumors make too much growth hormone. These are called growth hormone-secreting tumors or somatotroph adenomas. In adults, too much growth hormone causes a condition called acromegaly. Symptoms include:
- Changes in facial features, including larger lips, nose and tongue, prominent brow, a longer lower jaw, or wider spaces between teeth.
- Larger hands and feet.
- Snoring or sleep apnea.
- Thicker skin.
- More sweating and body odor.
- Joint pain.
- High blood pressure.
- High blood sugar.
- A deeper voice.
In children and teens, too much growth hormone can cause faster growth and unusual height. This is called gigantism.
- Pituitary tumors that make luteinizing hormone and follicle-stimulating hormone. Some pituitary tumors produce luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones also are known as gonadotropins. Pituitary tumors that make these hormones are called gonadotroph adenomas.
It's rare for these adenomas to make enough hormones to cause symptoms. Most of the time, symptoms are caused by the pressure from the tumor. When hormone-related symptoms do happen, they affect women and men differently.
Symptoms in women may include:
- Change in menstrual cycles.
- Fertility problems.
- Enlarged and painful ovaries, caused by a condition called ovarian hyperstimulation syndrome.
Symptoms in men may include:
- Enlarged testicles.
- Higher levels of testosterone.
Pituitary tumors that make prolactin
Pituitary adenomas that produce prolactin are called prolactinomas or lactotroph adenomas. Too much of the hormone prolactin lowers the body's levels of gonadotropins, which in turn lowers the sex hormones estrogen and testosterone. High prolactin affects men and women differently.
In women, too much prolactin may cause:
- Irregular or missed periods.
- Milky breast discharge not associated with pregnancy.
- Breast tenderness.
- Problems with fertility.
- Less interest in sex.
In men, too much prolactin can cause a condition called male hypogonadism. Symptoms may include:
- Trouble with erections.
- Less interest in sex.
- Growth of breast tissue.
- Problems with fertility.
Pituitary tumors that make thyroid-stimulating hormone
Some pituitary tumors make thyroid-stimulating hormone. These tumors are called thyrotroph adenomas or thyroid-stimulating hormone-secreting tumors. They cause the thyroid gland to release too much of the hormone thyroxine. That can lead to a condition called hyperthyroidism, also known as overactive thyroid disease. Hyperthyroidism speeds up the body's metabolism and can cause many symptoms. Some of the most common include:
- Unplanned weight loss.
- A fast or irregular heartbeat.
- Nervousness, anxiety or irritability.
- Frequent bowel movements.
- Sweating.
- Shaking or tremors.
- Sleep troubles.
When to see a doctor
If you notice symptoms that could be related to a pituitary tumor, see your healthcare professional. Treatment often can bring hormones back to a healthy level and ease symptoms.
Pituitary tumors are usually not inherited, but in rare cases they can run in families. In particular, the hereditary condition multiple endocrine neoplasia, type 1, (MEN 1) can increase the risk of pituitary tumors. If MEN 1 is in your family, talk to your healthcare professional about tests that may help find a pituitary tumor early.
Causes
Pituitary gland and hypothalamus
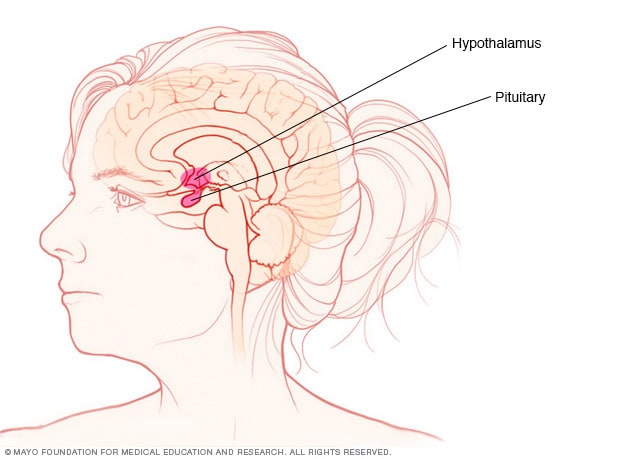
Pituitary gland and hypothalamus
The pituitary gland and the hypothalamus are located within the brain and control hormone production.
The pituitary gland is a small organ, about the size of a pea. It's located behind the nose at the base of the brain. Even though it's small, the pituitary gland affects nearly every part of the body. The hormones that the pituitary gland makes control important body functions, such as growth, blood pressure and reproduction.
The exact cause of pituitary tumors is not known. In rare cases, pituitary tumors can be caused by genes you've inherited. But most have no clear hereditary cause. Still, scientists think that changes in certain genes may play an important role in how pituitary tumors form.
Risk factors
Most people who develop pituitary tumors don't have any known risk factors. The environment and lifestyle choices don't seem to affect a person's risk of developing pituitary tumors.
While genes may play a role, most people with pituitary tumors don't have a family history of them.
The only known risk factors are rare hereditary conditions that raise the risk of many health conditions, including pituitary tumors. These conditions include:
How common are pituitary tumors?
Pituitary tumors are uncommon but not rare. About 100 in 100,000 people are living with a pituitary tumor that needs medical care. Each year about 4 to 7 people out of 100,000 are newly diagnosed with a pituitary tumor.
Many people also have very small pituitary growths that are found by chance and never cause symptoms. Studies of autopsies and brain-imaging tests suggest this happens in about 1 in 10 people.
Complications
Pituitary tumors usually don't spread to other parts of the body. They can affect a person's health, though. Pituitary tumors may cause:
- Vision changes, including vision loss.
- High blood pressure.
- High blood sugar.
- Bone loss.
- Heart issues.
- Trouble with thinking and memory.
Seizures
If a pituitary tumor presses on part of the brain called the medial temporal lobe, it sometimes can cause a seizure. This kind of seizure is called a focal seizure with impaired awareness. During this seizure, you may look awake but stare into space and not respond in a usual way. You also may lose awareness of what's happening and not remember the seizure afterward.
Permanent low hormone levels
Having a pituitary tumor or having one removed with surgery may permanently change your body's hormone supply. As a result, you may need hormone replacement therapy for the rest of your life.
Pituitary apoplexy
A rare but serious complication of a pituitary tumor is pituitary apoplexy. This happens when there is sudden bleeding into the tumor. Symptoms can include:
- A severe headache, likely the worst one you've ever had.
- Vision trouble, including double vision or loss of sight in one or both eyes.
- Upset stomach and vomiting.
- Confusion or trouble thinking clearly.
Pituitary apoplexy needs immediate care. Treatment often starts with corticosteroid medicine to reduce swelling around the tumor. In some cases, you may need surgery to remove the tumor.
What are the potential side effects of a pituitary tumor?
Pituitary tumors themselves don't cause side effects. But the changes in hormones or pressure in the brain from the tumor can cause side effects such as:
- Hormone changes can cause menstrual changes, milk leakage, low testosterone, weight or blood sugar changes, bone loss, and blood pressure changes.
- Pressure from a larger tumor can cause headaches, vision changes, or low levels of pituitary hormones that may need replacement.
What are side effects after pituitary tumor surgery?
Most people do well after endoscopic transnasal transsphenoidal surgery. Short-term effects such as nasal congestion, sore throat and headache are common and usually improve within days to weeks. Your healthcare team also watches for:
- Water balance changes in the first days after surgery. You may pass a lot of urine and feel very thirsty. A few days later, your sodium levels may drop. These are some of the common reasons for readmission to the hospital. These complications usually are temporary and treatable.
- Low pituitary hormones levels that may need replacement, such as thyroid hormone or cortisol.
- Less common surgical risks include cerebrospinal fluid (CSF) leak, bleeding and infection such as meningitis.
Prevention
There is no known way to prevent pituitary adenomas, as these tumors haven't been linked to any lifestyle choices. But living a healthy lifestyle supports your overall well-being and may help you manage any health conditions you have.
If you have a genetic condition that raises your risk of pituitary adenomas, regular screening may help find a tumor early. Finding pituitary adenomas early may increase the chances of successful treatment and improve long-term outcomes.
Dec. 23, 2025