Overview
The liver
The liver
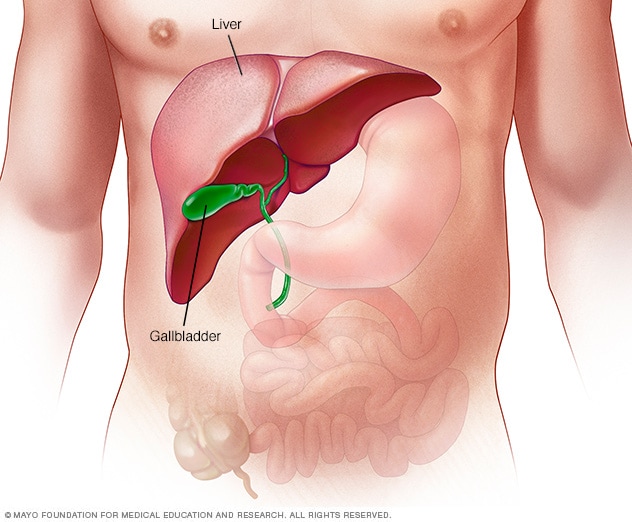
The liver is your largest internal organ. About the size of a football, it's located mainly in the upper right portion of your abdomen, beneath the diaphragm and above your stomach.
Start your donor evaluation
Begin the process of becoming a living kidney or liver donor by clicking here to complete a health history questionnaire.
A liver transplant is a surgery that removes a liver that no longer functions properly (liver failure) and replaces it with a healthy liver from a deceased donor or a portion of a healthy liver from a living donor.
Your liver is your largest internal organ and performs several critical functions, including:
- Processing nutrients, medications and hormones
- Producing bile, which helps the body absorb fats, cholesterol and fat-soluble vitamins
- Making proteins that help the blood clot
- Removing bacteria and toxins from the blood
- Preventing infection and regulating immune responses
Liver transplant is usually reserved as a treatment option for people who have significant complications due to end-stage chronic liver disease. Liver transplant may also be a treatment option in rare cases of sudden failure of a previously healthy liver.
The number of people waiting for a liver transplant greatly exceeds the number of available deceased-donor livers.
Receiving a portion of a liver from a living donor is an alternative to waiting for a deceased-donor liver to become available. Living-donor liver transplant is possible because the human liver regenerates and returns to its normal size shortly after surgical removal of part of the organ.
In 2018, about 8,200 liver transplants were performed in the U.S. among adults and children. Of those, about 390 involved livers from living donors. At the same time, about 12,800 people were registered on the waiting list for a liver transplant.
Products & Services
Types
Why it's done
Healthy liver vs. liver cirrhosis
Healthy liver vs. liver cirrhosis
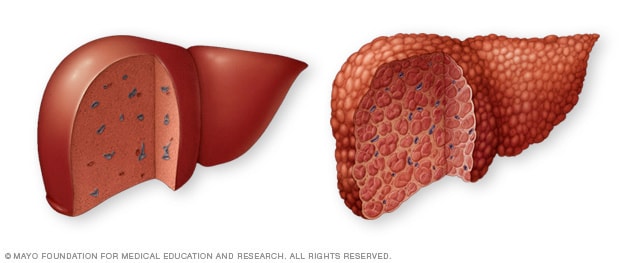
A typical liver, shown on the left, shows no signs of scarring. In cirrhosis, shown on the right, scar tissue replaces typical liver tissue.
Liver transplant is a treatment option for some people with liver cancer and for people with liver failure whose condition can't be controlled with other treatments.
Liver failure may happen quickly or over a long period of time. Liver failure that occurs quickly, in a matter of weeks, is called acute liver failure. Acute liver failure is an uncommon condition that is usually the result of complications from certain medications.
Although a liver transplant may treat acute liver failure, it is more often used to treat chronic liver failure. Chronic liver failure occurs slowly over months and years.
Chronic liver failure may be caused by a variety of conditions. The most common cause of chronic liver failure is scarring of the liver (cirrhosis). When cirrhosis occurs, scar tissue replaces typical liver tissue and the liver doesn't function properly. Cirrhosis is the most frequent reason for a liver transplant.
Major causes of cirrhosis leading to liver failure and liver transplant include:
- Hepatitis B and C.
- Alcoholic liver disease, which causes damage to the liver due to excessive alcohol consumption.
- Nonalcoholic fatty liver disease, a condition in which fat builds up in the liver, causing inflammation or liver cell damage.
- Genetic diseases affecting the liver. They include hemochromatosis, which causes excessive iron buildup in the liver, and Wilson's disease, which causes excessive copper buildup in the liver.
- Diseases that affect the tubes that carry bile away from the liver (bile ducts). They include primary biliary cirrhosis, primary sclerosing cholangitis and biliary atresia. Biliary atresia is the most common reason for liver transplant among children.
Liver transplant may also treat certain cancers that originate in the liver.
Risks
Complications of the procedure
Liver transplant surgery carries a risk of significant complications. There are risks associated with the procedure itself and with the drugs necessary to prevent rejection of the donor liver after the transplant.
Risks associated with the procedure include:
- Bile duct complications, including bile duct leaks or shrinking of the bile ducts
- Bleeding
- Blood clots
- Failure of the donated liver
- Infection
- Rejection of the donated liver
- Mental confusion or seizures
Long-term complications may also include the liver disease returning in the transplanted liver.
Anti-rejection medication side effects
After a liver transplant, you'll take medications for the rest of your life to help prevent your body from rejecting the donated liver. These anti-rejection medications can cause a variety of side effects, including:
- Bone thinning
- Diabetes
- Diarrhea
- Headaches
- High blood pressure
- High cholesterol
Because anti-rejection drugs work by suppressing the immune system, they also increase risk of infection. Your doctor may give you medications to help you fight infections.
How you prepare
Choosing a transplant center
If your doctor recommends a liver transplant, you may be referred to a transplant center. You're also free to select a transplant center on your own or choose a center from your insurance company's list of preferred providers.
When you're considering transplant centers, you may want to:
- Learn about the number and type of transplants the center performs each year.
- Ask about the transplant center's liver transplant survival rates.
- Compare transplant center statistics through the database maintained by the Scientific Registry of Transplant Recipients.
- Understand the costs that will be incurred before, during and after your transplant. Costs will include tests, organ procurement, surgery, hospital stays, and transportation to and from the center for the procedure and follow-up appointments.
- Consider additional services provided by the transplant center, such as coordinating support groups, assisting with travel arrangements, helping with local housing for your recovery period and offering referrals to other resources.
- Assess the center's commitment to keeping up with the latest transplant technology and techniques, which indicates that the program is growing.
After you've selected a transplant center, you'll need an evaluation to determine whether you meet the center's eligibility requirements. Each transplant center has its own eligibility criteria. If you aren't accepted at one transplant center, you may undergo evaluation at another center.
The goals of the evaluation process are to determine whether you:
- Are healthy enough to have surgery and can tolerate lifelong post-transplant medications
- Have any medical conditions that would interfere with transplant success
- Are willing and able to take medications as directed and follow the suggestions of the transplant team
Specific tests, procedures and consultations you may undergo include:
- Laboratory tests, such as blood and urine tests to assess the health of your organs, including your liver
- Imaging tests, such as an ultrasound of your liver
- Heart tests to determine the health of your cardiovascular system
- A general health exam, including routine cancer screening tests, to evaluate your overall health and to check for any other illnesses that may impact the success of your transplant
Your evaluation may also include:
- Nutrition counseling with dietitians who assess your diet and make recommendations on how to plan healthy meals before and after your transplant
- Psychological evaluation to assess and treat any underlying issues, such as depression or anxiety, and determine whether you fully understand the risks of a liver transplant
- Meetings with social workers who assess your support network to determine whether you have friends or family to help care for you after transplant
- Addiction counseling to help people who are having difficulty stopping their use of alcohol, drugs or tobacco
- Financial counseling to help you understand the cost of a transplant and post-transplant care and to determine what costs are covered by your insurance
Once these tests and consultations are completed, the transplant center's selection committee meets to discuss your situation. The committee determines whether a liver transplant is the best treatment for you and whether you're healthy enough to undergo a transplant.
If the answer to both questions is yes, then you're placed on the liver transplant waiting list.
What you can expect
Before the procedure
Being placed on the waiting list
Doctors will use the results of your liver function tests and other factors to assess the severity of your illness, how urgently you need a transplant and your place on the liver transplant waiting list.
Transplant waiting list priority is determined by a scoring system. Doctors use the Model for End-Stage Liver Disease (MELD) score for adults and Pediatric End-Stage Liver Disease (PELD) score for children younger than age 12.
Your doctor will use a specific formula to determine your MELD score, which can range from 6 to 40. The score estimates the risk of death within 90 days without a transplant. A high MELD score indicates the urgent need of a transplant.
As deceased-donor organs become available, they are classified by blood type and allocated according to MELD scores. People with higher MELD scores are generally offered donated livers first. Time spent on the liver transplant waiting list is used to break ties among people with the same MELD scores and blood types.
Some liver conditions, such as liver cancer, may not result in a person getting a high MELD score. The transplant center can request additional MELD points for people with specific diseases if they meet defined exception criteria.
In addition, adults with acute liver failure are exempted from the MELD-based donor organ prioritization system and may be placed higher on the transplant waiting list according to the severity of their disease.
Waiting for a new liver
The wait for a donor liver can vary greatly. Some people wait days, while others wait months or may never receive a deceased-donor liver.
As you wait for a new liver, your doctor will treat the complications of your liver failure to make you as comfortable as possible.
Complications of end-stage liver failure are serious, and you may be frequently hospitalized. If your liver deteriorates, your MELD score is updated.
Living liver donors
A small percentage of liver transplants each year are from living donors. In these cases, surgeons transplant a small portion of a liver from a healthy, living person. Living-donor liver transplants were initially used for children needing liver transplants because suitable deceased-donor organs are scarce. Now, it is also an option for adults who have end-stage liver disease.
Living-donor liver transplants offer an alternative to waiting for a deceased-donor liver and allow the organ recipient to avoid possible health complications of waiting for a transplant. The first step is to identify a living donor who is healthy and able to safely undergo a major surgical procedure. The donor's age, blood type and organ size also are critical considerations in determining whether you and the donor are a match for living-donor liver transplant.
Most living liver donors are close family members or friends of the liver transplant candidate. If you have a family member or friend who is willing to donate part of his or her liver to you, talk to your transplant team about this option.
Living-donor transplants have good results, just as transplants using livers from deceased donors. But finding a living donor may be difficult. Living liver donors go through extensive evaluation to ensure they are a match with the organ recipient and to assess their physical and mental health. The surgery also carries significant risks for the donor.
Your transplant team can discuss the benefits and risks with you and the potential donor.
Domino liver transplant
Another, less common, type of living-donor liver transplant is called a domino liver transplant. In a domino liver transplant, you receive a liver from a living donor who has a disease called familial amyloidosis. Familial amyloidosis is a very rare disorder in which an abnormal protein accumulates and eventually damages the body's internal organs.
In this procedure, the donor with familial amyloidosis receives a liver transplant to treat his or her condition. Then, the donor gives his or her liver to you in a domino liver transplant because the liver still functions well. You may eventually develop symptoms of amyloidosis, but these symptoms usually take decades to develop.
Doctors usually select recipients who are 55 years old or older and who aren't expected to develop symptoms before the end of their natural life expectancy. After the transplant, doctors monitor for signs of the condition.
Doctors will evaluate you to determine if you may be a candidate for a domino liver transplant or if another treatment option would be more appropriate for your condition.
Staying healthy
Whether you're waiting for a donated liver or your transplant surgery is already scheduled, work to stay healthy. Being healthy and as active as you're able can make it more likely you'll be ready for the transplant surgery when the time comes. It may also help speed your recovery from surgery. Work to:
- Take your medications as prescribed
- Follow your diet and exercise guidelines
- Keep all appointments with your health care team
- Stay involved in healthy activities, including relaxing and spending time with family and friends
Stay in touch with your transplant team and let them know of any significant changes in your health. If you're waiting for a donated liver, make sure the transplant team knows how to reach you at all times. Keep your packed hospital bag ready and make arrangements for transportation to the transplant center in advance.
During the procedure
Living-donor liver transplant
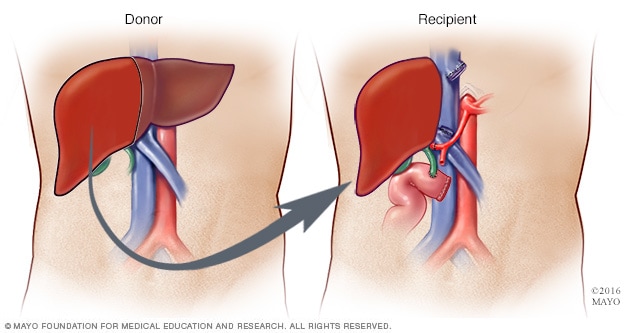
Living-donor liver transplant
During a living-donor liver transplant, surgeons remove about 40% to 70% of the donor liver and place it into the recipient.
Living-donor liver regeneration
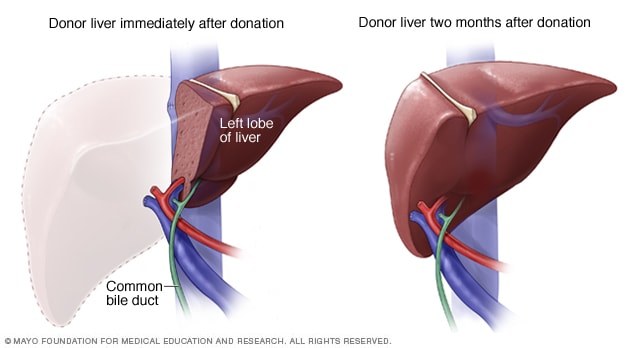
Living-donor liver regeneration
Within a couple of months after living-donor liver surgery, the donor's liver typically grows back to its previous size, volume and capacity.
Deceased-donor liver transplant
If you're notified that a liver from a deceased donor is available, you'll be asked to come to the hospital immediately. Your health care team will admit you to the hospital, and you'll undergo an exam to make sure you're healthy enough for the surgery.
Liver transplant surgery is done using general anesthesia, so you'll be in a sleep-like state during the procedure.
The transplant surgeon makes a long incision across your stomach to access your liver. The location and size of your incision varies according to your surgeon's approach and your own anatomy.
The surgeon removes your liver and places the donor liver in your body. Then the surgeon connects your blood vessels and bile ducts to the donor liver. Surgery can take up to 12 hours, depending on your situation.
Once your new liver is in place, the surgeon uses stitches and staples to close the surgical incision. You're then taken to the intensive care unit to begin recovery.
Living-donor liver transplant
If you're receiving a liver transplant from a living donor, your surgery will be scheduled in advance.
Surgeons first operate on the donor, removing the portion of the liver for transplant. Then surgeons remove your liver and place the donated liver portion in your body. They then connect your blood vessels and bile ducts to the new liver.
The transplanted liver portion in your body and the portion left behind in the donor's body regenerate rapidly, reaching normal volume within several weeks.
After the procedure
After a liver transplant
After your liver transplant, you can expect to:
- Possibly stay in the intensive care unit for a few days. Doctors and nurses will monitor your condition to watch for signs of complications. They'll also test your liver function frequently for signs that your new liver is working.
- Spend 5 to 10 days in the hospital. Once you're stable, you're taken to a transplant recovery area to continue recuperating.
- Have frequent checkups as you continue recovering at home. Your transplant team designs a checkup schedule for you. You may undergo blood tests a few times each week at first and then less often over time.
- Take medications for the rest of your life. You'll take a number of medications after your liver transplant. You'll need to continue taking many of them for the rest of your life. Drugs called immunosuppressants help keep your immune system from attacking your new liver. Other drugs help reduce the risk of other complications after your transplant.
Expect six months or more of recovery time before you'll feel fully healed after your liver transplant surgery. You may be able to resume normal activities or go back to work a few months after surgery. How long it takes you to recover may depend on how ill you were before your liver transplant.
Results
Liver transplant survival rates
Your chances of a successful liver transplant and long-term survival depend on your particular situation.
In general, about 75% of people who undergo liver transplant live for at least five years. That means that for every 100 people who receive a liver transplant for any reason, about 75 will live for five years and 25 will die within five years.
People who receive a liver from a living donor often have better short-term survival rates than those who receive a deceased-donor liver. But comparing long-term results is difficult because people who have a living donor usually have a shorter wait for a transplant and aren't as sick as those who receive a deceased-donor liver.
Survival rates among liver transplant recipients also vary among U.S. transplant centers and can be found online at the Scientific Registry of Transplant Recipients.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Coping and Support
It's normal to feel anxious or overwhelmed while waiting for a transplant or to have fears about rejection, returning to work or other issues after a transplant. Seeking the support of friends and family members can help you cope during this stressful time.
Your transplant team also can assist you with other useful resources and coping strategies throughout the transplant process, such as:
- Joining a support group for transplant recipients. Talking with others who have shared your experience can ease fears and anxiety.
- Sharing your experiences on social media. Social media is another way to engage with others who have had a similar experience, which may help you adjust to your changing situation.
- Finding rehabilitation services. If you're returning to work, your social worker may be able to connect you with rehabilitation services provided by your home state's department of vocational rehabilitation.
- Setting realistic goals and expectations. Recognize that life after transplant may not be exactly the same as life before transplant. Having realistic expectations about results and recovery time can help reduce stress.
- Educating yourself. Learn as much as you can about your procedure and ask questions about things you don't understand. Knowledge is empowering.
Diet and nutrition
After your liver transplant, it is especially important to eat a well-balanced diet to help you recover and keep your liver healthy.
Your transplant team includes a nutrition specialist (dietitian) who can discuss your nutrition and diet needs and answer any questions you have after your transplant.
In general, your diet after liver transplant should be low in salt, cholesterol, fat and sugar.
To prevent damaging your new liver, it's important to avoid alcohol. Do not drink alcoholic beverages or use alcohol in cooking.
Your dietitian will also provide you with several healthy food options and ideas to use in your nutrition plan. Your dietitian's recommendations may include:
- Eating at least five servings of fruits and vegetables each day
- Avoiding grapefruit and grapefruit juice because of their effect on a group of immunosuppression medications
- Having enough fiber in your daily diet
- Choosing whole-grain foods over processed ones
- Drinking low-fat or fat-free dairy products, which is important to maintain optimal calcium and phosphorus levels
Your dietitian may also recommend:
- Eating lean meats, poultry and fish
- Following food safety guidelines
- Staying hydrated by drinking adequate water and other fluids each day
Exercise
Exercise and physical activity should be a regular part of your life after a liver transplant to continue improving your overall physical and mental health.
Soon after your transplant, you should walk as much as you can. Then, depending on your progress, you can start incorporating more physical activity into your daily life.
Walking, bicycling, swimming, low-impact strength training and other physical activities you enjoy can all be a part of a healthy, active lifestyle after transplant. But be sure to check in with your transplant team before starting or changing your post-transplant exercise routine.
Jan. 19, 2024