Overview
Atrial fibrillation
Atrial fibrillation
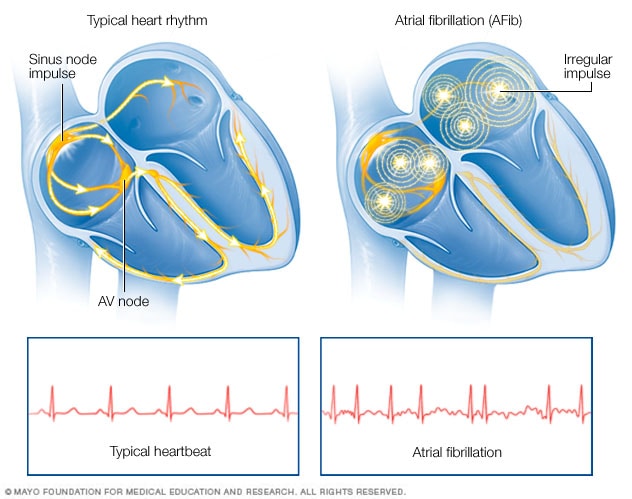
Atrial fibrillation (AFib) is a heart rhythm disorder. In a typical heart, a group of cells called the sinus node sends electrical signals that start each heartbeat. The signals go across the upper heart chambers to the AV node, where they usually slow down. Then the signals go to the lower heart chambers, causing them to squeeze and pump out blood. But in AFib, the signals in the upper chambers are chaotic. The AV node can't stop all of the chaotic signals from entering the lower chambers. This causes a fast and irregular heartbeat.
Atrial fibrillation (AFib) is an irregular and often very rapid heart rhythm. An irregular heart rhythm is called an arrhythmia. AFib can lead to blood clots in the heart. The condition also increases the risk of stroke, heart failure and other heart-related complications.
During atrial fibrillation, the heart's upper chambers, called the atria, beat chaotically and irregularly. They beat out of sync with the lower heart chambers, called the ventricles. AFib may cause a fast, pounding heartbeat, shortness of breath or light-headedness. Some people don't notice symptoms.
Episodes of atrial fibrillation may come and go, or they may be constant. AFib itself usually isn't life-threatening. But it's a serious condition that needs proper treatment to prevent stroke.
Treatment for AFib may include medicines, therapy to shock the heart back to a regular rhythm and procedures to block faulty heart signals.
A person with atrial fibrillation also may have a related heart rhythm disorder called atrial flutter. The treatments for AFib and atrial flutter are similar.
Products & Services
Symptoms
Symptoms of atrial fibrillation (AFib) may include:
- A fast, fluttering or pounding heartbeat, called palpitations.
- Chest pain.
- Dizziness.
- Fatigue.
- Lightheadedness.
- Reduced ability to exercise.
- Shortness of breath.
- Weakness.
Some people with AFib don't notice any symptoms.
Atrial fibrillation may be:
- Occasional, also called paroxysmal atrial fibrillation. AFib symptoms come and go. The symptoms usually last for a few minutes to hours. Some people have symptoms for as long as a week. The irregular heartbeat can happen again and again. Symptoms might go away on their own. Some people with this type of AFib need treatment.
- Persistent. The irregular heartbeat is constant. The heart rhythm does not correct itself. If symptoms occur, medical treatment is needed to reset the heart rhythm.
- Long-standing persistent. This type of AFib is constant and lasts longer than 12 months. Medicines or a procedure are needed to correct the irregular heartbeat.
- Permanent. The irregular heart rhythm can't be reset. Medicines are needed to control the heart rate and to prevent blood clots.
When to see a doctor
If you have symptoms of atrial fibrillation, make an appointment for a health checkup. You may be referred to a doctor trained in heart diseases, called a cardiologist.
If you have chest pain, get emergency medical help right away. Chest pain could mean that you're having a heart attack.
Causes
To understand the causes of atrial fibrillation (AFib), it may be helpful to know how the heart typically beats.
The heart has four chambers:
- The two upper chambers are called the atria.
- The two lower chambers are called the ventricles.
Inside the upper right heart chamber is a group of cells called the sinus node. The sinus node makes the signals that start each heartbeat.
The signals move across the upper heart chambers. Next, the signals arrive at a group of cells called the AV node, where they usually slow down. The signals then go to the lower heart chambers.
In a healthy heart, this signaling process usually goes smoothly. The resting heart rate is typically 60 to 100 beats a minute.
But in atrial fibrillation, the signals in the upper chambers of the heart are chaotic. As a result, the upper chambers tremble or shake. The AV node is flooded with signals trying to get through to the lower heart chambers. This causes a fast and irregular heart rhythm.
In people with AFib, the heart rate may range from 100 to 175 beats a minute.
Causes of atrial fibrillation
Changes with the heart's structure are the most common cause of atrial fibrillation (AFib).
Heart diseases and health conditions that can cause AFib include:
- A heart condition you're born with, called a congenital heart defect.
- A heart rhythm disorder that affects the heart's natural pacemaker, called sick sinus syndrome.
- A sleep disorder called obstructive sleep apnea.
- Heart attack.
- Heart valve disease.
- High blood pressure.
- Lung diseases, including pneumonia.
- Narrowed or blocked arteries, called coronary artery disease.
- Thyroid disease such as an overactive thyroid.
- Infections from viruses.
Heart surgery or stress due to surgery or sickness also may cause AFib. Some people who have atrial fibrillation have no known heart disease or heart damage.
Lifestyle habits that can send the heart into AFib may include:
- Drinking too much alcohol or caffeine.
- Illegal drug use.
- Smoking or using tobacco.
- Taking medicines that have stimulants, including cold and allergy medicines bought without a prescription.
Risk factors
Things that can increase the risk of atrial fibrillation (AFib) include:
- Age. The risk of AFib increases as you grow older.
- Caffeine, nicotine or illegal drug use. Caffeine, nicotine and some illegal drugs — such as amphetamines and cocaine — can cause your heart to beat faster. Use of these substances may lead to the development of more-serious irregular heartbeats.
- Drinking too much alcohol. Drinking too much alcohol can affect the electrical signals in the heart and cause an irregular heartbeat.
- Changes in the level of body minerals. Minerals in the blood called electrolytes help the heart beat. They include potassium, sodium, calcium and magnesium. If these substances are too low or too high, irregular heartbeats may occur.
- Family history. An increased risk of atrial fibrillation occurs in some families.
- Heart conditions or heart surgery. Coronary artery disease, heart valve disease and heart conditions present at birth increase the risk of AFib. A history of heart attack or heart surgery also makes a person more likely to get the condition.
- High blood pressure. Over time, high blood pressure may cause part of the heart to become stiff and thick. This can change how heartbeat signals travel through the heart.
- Obesity. People who have obesity are at higher risk of developing atrial fibrillation.
- Other long-term health conditions. You may be more likely to get AFib if you have diabetes, chronic kidney disease, lung disease or sleep apnea.
- Some medicines and supplements. Some prescription medicines and certain cough and cold remedies bought without a prescription can cause irregular heartbeats.
- Thyroid disease. Having an overactive thyroid gland can raise the risk of irregular heartbeats.
Complications
A possible complication of atrial fibrillation (AFib) is blood clots. Blood clots can lead to stroke.
The risk of stroke from AFib increases as you grow older. Other health conditions also may increase the risk of a stroke due to AFib. These conditions include:
- High blood pressure.
- Diabetes.
- Heart failure.
- Some types of heart valve disease.
Blood thinners are commonly used to prevent blood clots and strokes in people with atrial fibrillation.
Prevention
Healthy lifestyle choices can reduce the risk of heart disease and may prevent atrial fibrillation (AFib). Here are some basic heart-healthy tips:
- Control high blood pressure, high cholesterol and diabetes.
- Don't smoke or use tobacco.
- Eat nutritious foods that are low in salt and saturated fat.
- Exercise at least 30 minutes a day on most days of the week unless your healthcare team says not to.
- Keep a healthy weight.
- Get good sleep. Adults should aim for 7 to 9 hours daily.
- Reduce and manage stress.
Oct. 03, 2025