Overview
Bile duct damage
Bile duct damage
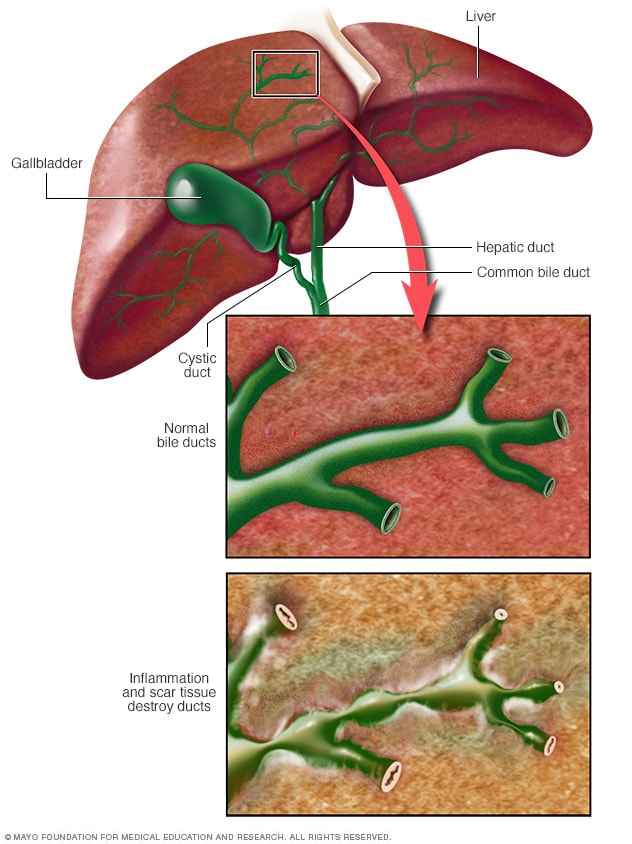
Bile ducts carry bile from the liver to the small intestine. Bile helps break down fats. When bile ducts become damaged, bile can back up into the liver, causing damage to liver cells. This damage can lead to liver failure.
Primary biliary cholangitis is an autoimmune disease in which the bile ducts are inflamed and slowly destroyed. It previously was called primary biliary cirrhosis.
Bile is a fluid made in the liver. It helps with digestion and absorbing certain vitamins. It also helps the body absorb fats and get rid of cholesterol, toxins and worn-out red blood cells. Ongoing inflammation in the liver can lead to bile duct inflammation and damage known as cholangitis. At times, this can lead to permanent scarring of liver tissue, called cirrhosis. It also can eventually lead to liver failure.
Although it affects both sexes, primary biliary cholangitis mostly affects women. It's considered an autoimmune disease, which means your body's immune system is mistakenly attacking healthy cells and tissue. Researchers think a combination of genetic and environmental factors triggers the disease. It usually develops slowly. At this time, there's no cure for primary biliary cholangitis, but medicines may slow liver damage, especially if treatment begins early.
Products & Services
Symptoms
More than half of people with primary biliary cholangitis do not have any noticeable symptoms when diagnosed. The disease may be diagnosed when blood tests are done for other reasons, such as routine testing. Symptoms eventually develop over the next 5 to 20 years. Those who do have symptoms at diagnosis typically have poorer outcomes.
Common early symptoms include:
Later signs and symptoms may include:
- Yellowing of the skin and eyes, called jaundice.
- Dry eyes and mouth.
- Pain in the upper right abdomen.
- Swelling of the spleen, called splenomegaly.
- Bone, muscle or joint pain.
- Swollen feet and ankles.
- Buildup of fluid in the abdomen due to liver failure, called ascites.
- Fatty deposits, called xanthomas, on the skin around the eyes, eyelids or in the creases of the palms, soles, elbows or knees.
- Darkening of the skin that's not related to sun exposure, called hyperpigmentation.
- Weak and brittle bones, called osteoporosis, which can lead to fractures.
- High cholesterol.
- Diarrhea that may include greasy stools, called steatorrhea.
- Underactive thyroid, called hypothyroidism.
- Weight loss.
Causes
It's not clear what causes primary biliary cholangitis. Many experts consider it an autoimmune disease in which the body turns against its own cells. Researchers believe this autoimmune response may be triggered by environmental and genetic factors.
The liver inflammation seen in primary biliary cholangitis starts when certain types of white blood cells called T cells, also known as T lymphocytes, start to collect in the liver. Usually, these immune cells detect and help defend against germs, such as bacteria and viruses. But in primary biliary cholangitis, they mistakenly destroy the healthy cells that line the small bile ducts in the liver.
Inflammation in the smallest ducts spreads and eventually damages other cells in the liver. As the cells die, they're replaced by scar tissue, also known as fibrosis, that can lead to cirrhosis. Cirrhosis is scarring of liver tissue that makes it difficult for your liver to work properly.
Risk factors
The following factors may increase your risk of primary biliary cholangitis:
- Sex. Most people with primary biliary cholangitis are women.
- Age. It's most likely to occur in people 30 to 60 years old.
- Genetics. You're more likely to get the condition if you have a family member who has or had it.
- Geography. It's most common in people of northern European descent, but primary biliary cholangitis can affect all ethnicities and races.
Researchers think that genetic factors combined with certain environmental factors trigger primary biliary cholangitis. These environmental factors may include:
- Infections, such as a urinary tract infection.
- Smoking cigarettes, especially over long periods of time.
- Exposure to toxic chemicals, such as in certain work environments.
Complications
As liver damage worsens, primary biliary cholangitis can cause serious health problems, including:
- Liver scarring, called cirrhosis. Cirrhosis makes it difficult for your liver to work and may lead to liver failure. It means the later stage of primary biliary cholangitis. People with primary biliary cholangitis and cirrhosis have a poor medical outlook. They also have a higher risk of other complications.
- Increased pressure in the portal vein, called portal hypertension. Blood from your intestine, spleen and pancreas enters your liver through a large blood vessel called the portal vein. When scar tissue from cirrhosis blocks normal blood flow through your liver, blood backs up. This causes increased pressure inside the vein. Also, because blood doesn't flow correctly through your liver, drugs and other toxins aren't filtered properly from your bloodstream.
- Enlarged veins, called varices. When blood flow through the portal vein is slowed or blocked, blood may back up into other veins. It usually backs up into those in your stomach and esophagus. Increased pressure may cause delicate veins to break open and bleed. Bleeding in the upper stomach or esophagus is a life-threatening emergency. It requires immediate medical care.
- Enlarged spleen, called splenomegaly. Your spleen may become swollen with white blood cells and platelets. This is because your body no longer filters toxins out of the bloodstream as it should.
- Gallstones and bile duct stones. If bile cannot flow through the bile ducts, it may harden into stones in the ducts. These stones can cause pain and infection.
- Liver cancer. Liver scarring increases your risk of liver cancer. If you have liver scarring, you'll need regular cancer screening.
- Weak bones, called osteoporosis. People with primary biliary cholangitis have an increased risk of weak, brittle bones that may break more easily.
- Vitamin deficiencies. Not having enough bile affects your digestive system's ability to absorb fats and the fat-soluble vitamins, A, D, E and K. Because of this, some people with advanced primary biliary cholangitis may have low levels of these vitamins. Low levels can result in a variety of health problems, including night blindness and bleeding disorders.
- High cholesterol. Up to 80% of people with primary biliary cholangitis have high cholesterol.
- Decreased mental function, called hepatic encephalopathy. Some people with advanced primary biliary cholangitis and cirrhosis have personality changes. They also may have problems with memory and concentration.
- Increased risk of other disease. Primary biliary cholangitis is associated with other disorders, including those that affect the thyroid, skin and joints. It also can be associated with dry eyes and mouth, a disorder called Sjogren's syndrome.
Sept. 16, 2025