Overview
Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy
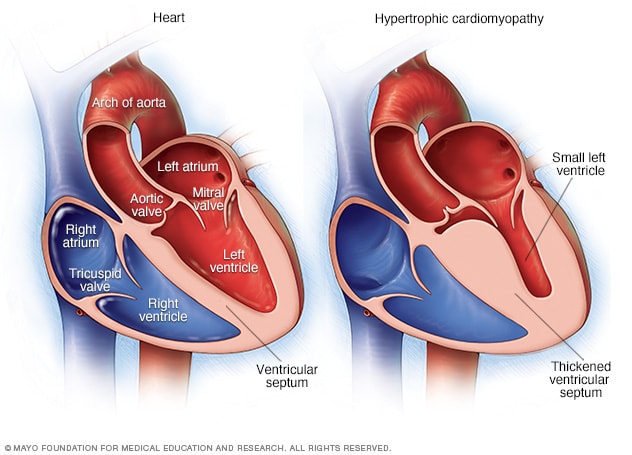
In hypertrophic cardiomyopathy, the muscular heart wall called the septum often becomes thicker than usual. But the thickening can happen anywhere in the left lower heart chamber, also called the left ventricle.
Hypertrophic cardiomyopathy (HCM) is a disease in which the heart muscle becomes thickened, also called hypertrophied. The thickened heart muscle can make it harder for the heart to pump blood.
Many people with hypertrophic cardiomyopathy don't realize they have it. That's because they have few, if any, symptoms. But in a small number of people with HCM, the thickened heart muscle can cause serious symptoms. These include shortness of breath and chest pain. Some people with HCM have changes in the heart's electrical system. These changes can result in life-threatening irregular heartbeats or sudden death.
Symptoms
Symptoms of hypertrophic cardiomyopathy can include one or more of the following:
- Chest pain, especially during exercise.
- Fainting, especially during or just after exercise or other physical activity.
- Sensation of fast, fluttering or pounding heartbeats called palpitations.
- Shortness of breath, especially during exercise.
When to see a doctor
Many conditions can cause shortness of breath and fast, pounding heartbeats. It's important to get a prompt checkup to find the cause and receive the right care. See your healthcare professional if you have a family history of HCM or any symptoms related to hypertrophic cardiomyopathy.
Call 911 or your local emergency number if you have any of the following symptoms for more than a few minutes:
- Rapid or irregular heartbeat.
- Trouble breathing.
- Chest pain.
Causes
Hypertrophic cardiomyopathy usually is caused by changes in genes that cause the heart muscle to thicken.
Hypertrophic cardiomyopathy typically affects the wall between the two bottom chambers of the heart. This wall is called the septum. The chambers are called the ventricles. The thickened wall might block blood flow out of the heart. This is called obstructive hypertrophic cardiomyopathy.
If there's no significant blocking of blood flow, the condition is called nonobstructive hypertrophic cardiomyopathy. But the heart's main pumping chamber, called the left ventricle, might stiffen. This makes it hard for the heart to relax. The stiffness also lessens the amount of blood the ventricle can hold and send to the body with each heartbeat.
Heart muscle cells also become arranged differently in people with hypertrophic cardiomyopathy. This is called myofiber disarray. It can trigger irregular heartbeats in some people.
Risk factors
Hypertrophic cardiomyopathy usually is passed down through families. That means it's inherited. People with one parent with hypertrophic cardiomyopathy have a 50% chance of having the gene change that causes the disease.
Parents, children, or brothers or sisters of a person with hypertrophic cardiomyopathy should ask their healthcare team about screening tests for the disease.
Complications
Complications of hypertrophic cardiomyopathy can include:
- Atrial fibrillation (AFib). A thickened heart muscle and changes in the structure of heart cells can trigger an irregular and often very rapid heartbeat called AFib. AFib also raises the risk of blood clots, which can travel to the brain and cause a stroke.
- Blocked blood flow. In many people, the thickened heart muscle blocks the blood flow leaving the heart. This can cause shortness of breath with activity, chest pain, dizziness and fainting spells.
- Mitral valve disease. If the thickened heart muscle blocks the blood flow leaving the heart, the valve between the left heart chambers might not close properly. That valve is called the mitral valve. If it doesn't close properly, blood can leak backward into the left upper chamber. This is a condition called mitral valve regurgitation. It might make hypertrophic cardiomyopathy symptoms worse.
- Dilated cardiomyopathy. In a small number of people with HCM, the thickened heart muscle becomes weak and doesn't work well. The condition tends to start in the left lower heart chamber. The chamber becomes larger. The heart pumps with less force.
- Heart failure. Over time, the thickened heart muscle can become too stiff to fill the heart with blood. As a result, the heart can't pump enough blood to meet the body's needs.
- Fainting, also called syncope. An irregular heartbeat or blockage of blood flow can sometimes cause fainting. Unexplained fainting can be related to sudden cardiac death, especially if it's happened recently and in a young person.
- Sudden cardiac death. Rarely, hypertrophic cardiomyopathy can cause heart-related sudden death in people of all ages. Many people with hypertrophic cardiomyopathy don't realize they have it. As a result, sudden cardiac death might be the first sign of the condition. It can happen in young people who seem healthy, including high school athletes and other young, active adults.
Prevention
There is no known way to prevent hypertrophic cardiomyopathy (HCM). It's important to find the condition with tests as early as possible to guide treatment and prevent complications.
Hypertrophic cardiomyopathy usually is passed down in families. If you have a parent, brother, sister or child with hypertrophic cardiomyopathy, ask your healthcare team if genetic screening is right for you. But not everyone with HCM has a gene change that tests can detect. Also, some insurance companies may not cover genetic testing.
If genetic testing isn't done, or if the results aren't helpful, screening may be done with repeated echocardiograms. Echocardiograms use sound waves to make pictures of the heart.
For people who have a family member with hypertrophic cardiomyopathy:
- Echocardiogram screenings are recommended starting at about age 12.
- Screening with echocardiograms should continue every 1 to 3 years through ages 18 to 21.
- After that, the screenings can be done every five years through adulthood.
You may need to have an echocardiogram more often based on your overall health and healthcare team's preference.
Feb. 23, 2024