Overview
An atrial septal defect (ASD) is a heart condition that you're born with. That means it's a congenital heart defect. People with an ASD have a hole between the upper heart chambers. The hole increases the amount of blood going through the lungs.
Small atrial septal defects might be found by chance and never cause a concern. Others might close during infancy or early childhood.
A large, long-term atrial septal defect can damage the heart and lungs. Surgery may be needed to repair an atrial septal defect and to prevent complications.
Types
Types of atrial septal defects (ASDs) include:
- Secundum. This is the most common type of ASD. It occurs in the middle of the wall between the upper heart chambers. This wall is called the atrial septum.
- Primum. This type of ASD affects the lower part of the wall between the upper heart chambers. It might occur with other heart problems present at birth.
- Sinus venosus. This is a rare type of ASD. It most often happens in the upper part of the wall between the heart chambers. It often occurs with other heart structure changes present at birth.
- Coronary sinus. The coronary sinus is part of the vein system of the heart. In this rare type of ASD, part of the wall between the coronary sinus and the left upper heart chamber is missing.
Products & Services
Symptoms
A baby born with an atrial septal defect (ASD) may not have symptoms. Symptoms may begin in adulthood.
Atrial septal defect symptoms may include:
- Shortness of breath, especially when exercising.
- Tiredness, especially with activity.
- Swelling of the legs, feet or belly area.
- Irregular heartbeats, also called arrhythmias.
- Skipped heartbeats or feelings of a quick, pounding or fluttering heartbeat, called palpitations.
When to see a doctor
Serious congenital heart defects are often diagnosed before or soon after a child is born.
Get immediate emergency help if a child has trouble breathing.
Call a healthcare professional if these symptoms occur:
- Shortness of breath, especially during exercise or activity.
- Easy tiring, especially after activity.
- Swelling of the legs, feet or belly area.
- Skipped heartbeats or feelings of a quick, pounding heartbeat.
Causes
The cause of atrial septal defect is not clear. The problem affects the structure of the heart. It happens as the baby's heart is forming during pregnancy.
The following may play a role in the cause of congenital heart defects such as atrial septal defect:
- Changes in genes.
- Some medical conditions.
- Certain medicines.
- Smoking.
- Alcohol misuse.
How the heart works
Chambers and valves of the heart
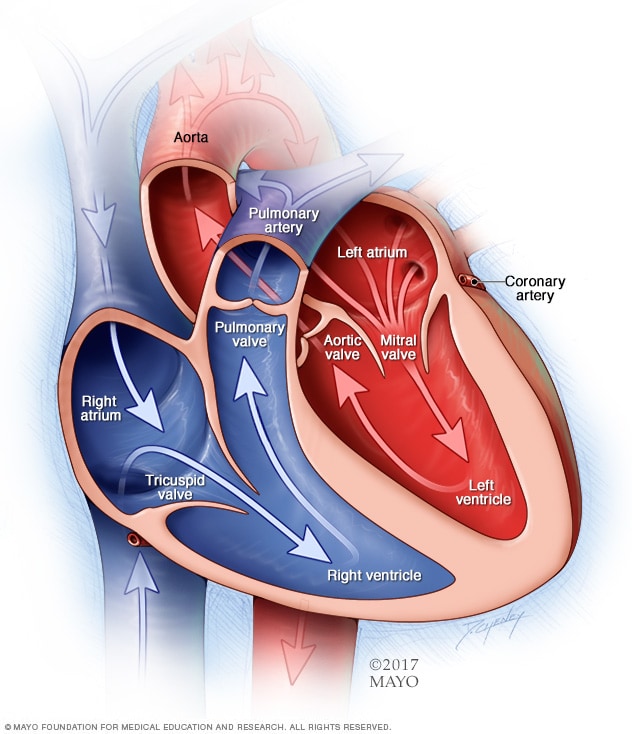
Chambers and valves of the heart
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves are gates at the chamber openings. They keep blood flowing in the right direction.
Atrial septal defect
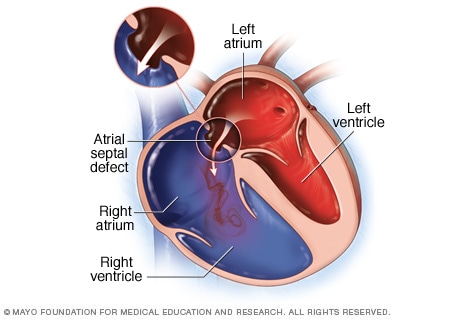
Atrial septal defect
An atrial septal defect (ASD) is a hole between the heart's upper chambers. The heart problem is present at birth. It is a type of congenital heart defect.
To understand the cause of atrial septal defect, it may be helpful to know how the heart typically works.
The typical heart is made of four chambers. The two upper chambers are called the atria. The two lower chambers are called the ventricles.
The right side of the heart moves blood to the lungs. In the lungs, blood picks up oxygen and then returns it to the heart's left side. The left side of the heart then pumps the blood through the body's main artery, called the aorta. The blood then goes out to the rest of the body.
A large atrial septal defect can send extra blood to the lungs and cause the right side of the heart to work too hard. Without treatment, the right side of the heart grows larger over time and becomes weak. The blood pressure in the arteries in the lungs also can increase, causing pulmonary hypertension.
Risk factors
Atrial septal defect (ASD) occurs as the baby's heart is forming during pregnancy. It is a congenital heart defect. Things that may increase a baby's risk of atrial septal defect or other heart problems present at birth include:
- German measles, also called rubella, during the first few months of pregnancy.
- Diabetes.
- Lupus.
- Alcohol or tobacco use during pregnancy.
- Cocaine use during pregnancy.
- Use of some medicines during pregnancy, including those to treat seizures and mood conditions.
Some types of congenital heart defects occur in families. This means they are inherited. Tell your care team if you or someone in your family had a heart problem present at birth. Screening by a genetic counselor can help show the risk of certain heart defects in future children.
Complications
A small atrial septal defect might never cause any concern. Small atrial septal defects often close during infancy.
Larger atrial septal defects can cause serious complications, including:
- Right-sided heart failure.
- Irregular heartbeats, called arrhythmias.
- Stroke.
- Early death.
- High blood pressure in the lung arteries, called pulmonary hypertension.
Pulmonary hypertension can cause permanent lung damage. This complication, called Eisenmenger syndrome, most often occurs over many years. It sometimes happens in people with large atrial septal defects.
Treatment can prevent or help manage many of these complications.
Atrial septal defect and pregnancy
If you have an atrial septal defect and are pregnant or thinking about becoming pregnant, talk to a care professional first. It's important to get proper prenatal care. A healthcare professional may suggest repairing the hole in the heart before getting pregnant. A large atrial septal defect or its complications can lead to a high-risk pregnancy.
Prevention
Because the cause of atrial septal defect (ASD) is not clear, prevention may not be possible. But getting good prenatal care is important. If you were born with an ASD, make an appointment for a health checkup before becoming pregnant.
During this visit:
- Talk about current health conditions and medicines. It's important to closely control diabetes, lupus and other health conditions during pregnancy. Your healthcare professional may suggest changing doses of some medicines or stopping them before pregnancy.
- Review your family medical history. If you have a family history of congenital heart defects or other genetic conditions, you might talk with a genetic counselor to find your risks.
- Ask about getting tested to see if you've had German measles, also called rubella. Rubella in a pregnant person has been linked to some types of congenital heart defects in the baby. If you haven't already had German measles or the vaccine, get the recommended vaccinations.
Jan. 23, 2024