Breast cancer types: What your type means
Not all breast cancers are the same. Find out how healthcare professionals decide the breast cancer type and what it means.
By Mayo Clinic Staff
One thing your healthcare team considers when making your breast cancer treatment plan is the type of breast cancer that you have. The type tells your healthcare team about the cells that make up your breast cancer. Your team uses this information to choose the treatments that are most likely to help you.
Much of the information about your type of breast cancer can be found in a pathology report. A pathology report is made by the doctors who test samples of your breast cancer cells in a lab. These doctors are called pathologists. Ask a member of your healthcare team to help you understand what your pathology report means.
Here's a look at what's considered when deciding what type of breast cancer you have.
What kinds of cells are involved in the breast cancer?
Breast anatomy
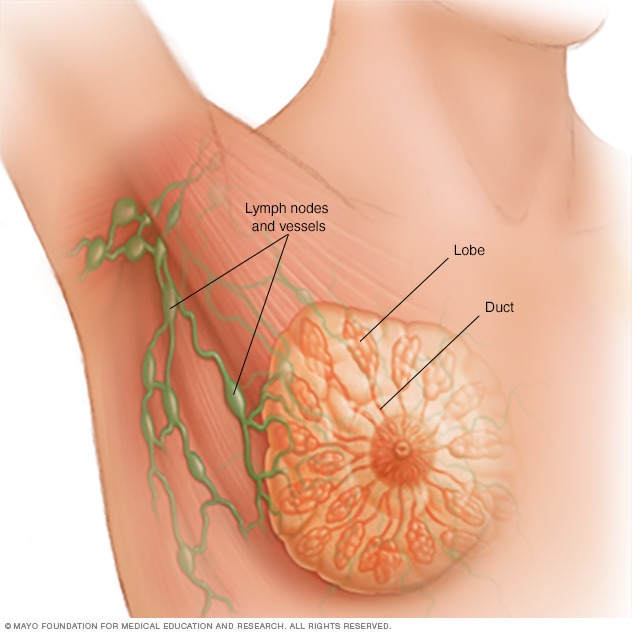
Breast anatomy
Each breast contains 15 to 20 lobes of glandular tissue, arranged like the petals of a daisy. The lobes are further divided into smaller lobules that produce milk for breastfeeding. Small tubes, called ducts, conduct the milk to a reservoir that lies just beneath the nipple.
Pathologists in the lab look at the kind of cells that make up the breast cancer. Kinds of cells include:
- Ductal cells. Ductal breast cancer, also called ductal carcinoma, is the most common type of breast cancer. This type of cancer starts in cells in the lining of a milk duct within the breast. The ducts can carry breast milk to the nipple.
- Lobular cells. Lobular breast cancer, also called lobular carcinoma, starts in the lobules of the breast. The lobules can make breast milk. The lobules are connected to the ducts, which can carry breast milk to the nipple.
- Connective tissue cells. Rarely, cancer in the breast is made up of connective tissue cells. Connective tissue includes the muscles, fat and blood vessels. Cancer that begins in the connective tissue is called soft tissue sarcoma. Examples of rare breast sarcomas include angiosarcoma and leiomyosarcoma.
- Lymphatic system cells. Lymphoma is a cancer that starts in the cells of the lymphatic system. Very rarely, lymphoma can start in lymphatic system cells in the breast. Most breast lymphomas are a kind of non-Hodgkin lymphoma.
How do the cancer cells look under a microscope?
When looking at the breast cancer cells with a microscope, the pathologist looks for:
- Cancer cells with unique appearances. Some subtypes of breast cancer are named for the way they look under the microscope. Subtypes include tubular, mucinous, medullary and micropapillary. Your subtype gives your healthcare team some clues about your prognosis and how your cells may respond to treatment.
- Differences between the cancer cells and healthy cells. How different the cancer cells look from healthy cells is called the cancer's grade. Breast cancer grades go from 1 to 3. A grade 1 breast cancer has cells that look a little different from healthy cells. It generally means the cancer is likely to grow more slowly. A grade 3 breast cancer has cells that look very different from healthy cells. It generally means that the cancer is more likely to grow quickly.
Are the cancer cells fueled by hormones?
Some breast cancers are sensitive to the hormones estrogen and progesterone. Pathologists look for hormone receptors on the outside of the breast cancer cells. Cancer cells use these receptors to catch hormones that are circulating in the body. The cells use the hormones for fuel to grow the cancer.
Hormone status of breast cancers includes:
- Estrogen receptor positive. A breast cancer that's estrogen receptor positive, also called ER positive, has receptors for the hormone estrogen. Treatment with hormone therapy can block the growth of the cancer cells. Another term for breast cancer hormone therapy is endocrine therapy.
- Progesterone receptor positive. A breast cancer that's progesterone receptor positive, also called PR positive, has receptors for the hormone progesterone. Treatment with endocrine therapy can block the growth of the cancer cells.
- Hormone receptor negative. A breast cancer that doesn't have hormone receptors is hormone receptor negative, also called HR negative. Endocrine therapy that blocks hormones in the body doesn't work for this type of breast cancer.
Most breast cancers have hormone receptors.
Do the cancer cells make extra HER2?
Some breast cancer cells make too much of a protein called human epithelial growth factor-receptor 2, also called HER2. Healthy breast cells make some HER2, but the cancer cells can make a lot more. Tests in the lab can show whether your breast cancer cells make extra HER2.
Tests for HER2 can show whether your breast cancer is:
- HER2 positive. Breast cancer cells that make a lot of extra HER2 protein are called HER2 positive. Targeted therapy treatments with medicine that hurts cells making too much HER2 can help control this kind of breast cancer.
- HER2 low. Breast cancer is called HER2 low if some of the cancer cells show signs of making extra HER2. This result can happen if only some of the cells are making extra HER2. It also might mean the cells making HER2 are making low levels of the protein. Targeted therapy against HER2 may be a treatment option for HER2 low breast cancers in certain situations.
- HER2 negative. If the breast cancer cells don't make extra HER2, then the cancer is HER2 negative. Targeted therapy against the HER2 protein won't work for these breast cancers.
About half of breast cancers are believed to be HER2 low. Treatment for HER2-low breast cancer is an active area of cancer research.
What are some types of breast cancer?
Some types of breast cancer include:
- Ductal carcinoma in situ. Ductal carcinoma in situ, also called DCIS, is a type of breast cancer that's not invasive. It happens when cancer cells form in a breast duct. The cancer cells stay in the duct and don't spread into the breast tissue. It's sometimes called noninvasive cancer or stage 0 breast cancer.
- HER2-positive breast cancer. A HER2-positive breast cancer is any invasive breast cancer that makes a lot of extra HER2 protein. HER2-positive breast cancers tend to grow more quickly. But treatment with targeted therapy medicines that hurt cells making extra HER2 is very effective against these cancers.
- Invasive ductal carcinoma. Invasive ductal carcinoma is a type of breast cancer that starts in a breast duct. It's the most common type of breast cancer.
- Invasive lobular carcinoma. Invasive lobular carcinoma is a type of breast cancer that starts in a milk gland in the breast, also called a lobule.
- Triple-negative breast cancer. A triple-negative breast cancer means the cancer cells don't have receptors for HER2 or for the hormones estrogen and progesterone. Treatments with medicine that targets HER2 won't work against this kind of breast cancer. Endocrine therapy to block hormones in the body also won't work.
To plan the best treatment for you, your healthcare team considers your breast cancer type and many other factors. These other factors include the cancer's stage and the likelihood that the cancer will come back after treatment. Your team also considers your preferences and your overall health.
Oct. 31, 2024
- Breast invasive, resection. American College of Pathologists. https://www.cap.org/protocols-and-guidelines/cancer-reporting-tools/cancer-protocol-templates. Accessed March 4, 2024.
- Chugh R, et al. Breast sarcoma: Epidemiology, risk factors, clinical presentation, diagnosis and staging. https://www.uptodate.com/contents/search. Accessed Feb. 29, 2024.
- Breast cancer treatment – Patient version. National Cancer Institute. https://www.cancer.gov/types/breast/patient/breast-treatment-pdq. Accessed Feb. 29, 2024.
- Klimberg VS, et al., eds. Bland and Copeland's The Breast: Comprehensive Management of Benign and Malignant Diseases. 6th ed. Elsevier; 2024. https://www.clinicalkey.com. Accessed Feb. 29, 2024.
- Bleiweiss IJ. Pathology of breast cancer. https://www.uptodate.com/contents/search. Accessed Feb. 16, 2024.
- Roy AM, et al. A review of treatment options in HER2-low breast cancer and proposed treatment sequencing algorithm. Cancer. 2023; doi:10.1002/cncr.34904.
- Breast cancer. Cancer.Net. https://www.cancer.net/cancer-types/breast-cancer/view-all. Accessed March 4, 2024.