Diagnosis and testing
Endoscopic retrograde cholangiopancreatography
Endoscopic retrograde cholangiopancreatography
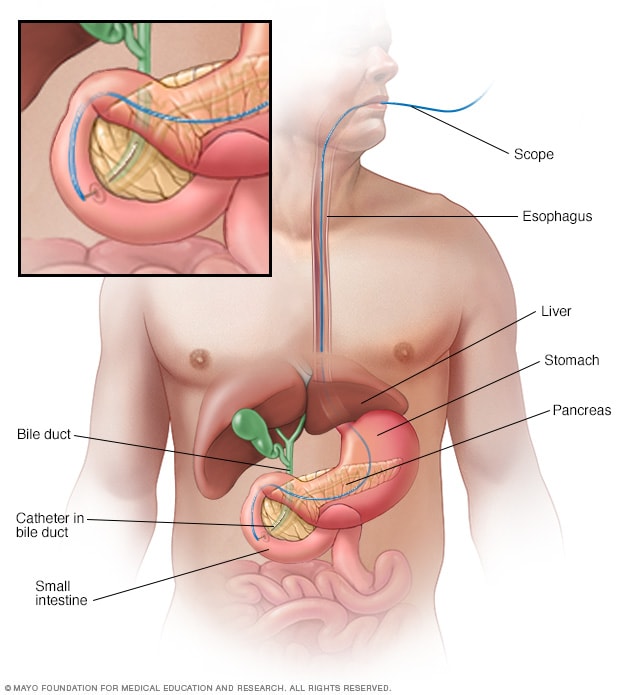
Endoscopic retrograde cholangiopancreatography (ERCP) uses a dye to highlight the bile ducts on X-ray images. A thin, flexible tube with a camera on the end, called an endoscope, goes through the throat and into the small intestine. The dye enters the ducts through a small hollow tube, called a catheter, passed through the endoscope. Tiny tools passed through the catheter also can be used to remove gallstones.
Liver biopsy

Liver biopsy
A liver biopsy is a procedure to remove a small sample of liver tissue for laboratory testing. A liver biopsy is commonly performed by inserting a thin needle through your skin and into your liver.
Tests and procedures used to diagnose PSC include:
- Liver function blood tests. These tests check protein and enzyme levels, such as alkaline phosphatase, to see how well your liver is working.
- MRI of your bile ducts. The primary diagnostic tool is magnetic resonance imaging (MRI), of the liver, bile ducts, gallbladder and pancreas. The test is called magnetic resonance cholangiopancreatography (koh-lan-jee-o-pan-cree-uh-TOG-ruh-fee).
-
X-rays of your bile ducts. Another option for imaging is a specialized X-ray exam called a cholangiogram. This procedure uses a dye to highlight the bile ducts on an X-ray image. These tests usually are done if MRI is not an option.
The dye may be delivered by a tube that is fed through the digestive tract and passes from the small intestine into the main bile duct. This method is called endoscopic retrograde cholangiopancreatography (ERCP). The dye also may be injected through the skin and into the liver.
- Liver biopsy. With a liver biopsy, a needle is used to remove a piece of liver that can be studied in a lab. An exam of the tissue under a microscope can show the condition of the bile ducts and liver tissues. Liver biopsy is sometimes called a PSC specimen test. Lab technicians examine the tissue specimen for inflammation, scarring and bile duct changes. Biopsy is most useful if PSC is suspected but not clear on imaging. It also may be useful if there is concern about overlap with autoimmune hepatitis.
Examining the colon
A colonoscopy is a procedure to see inside the large intestine, also called the colon. A long, flexible tube with a camera, called an endoscope, is inserted into the rectum and passed into the colon. The exam allows your healthcare professional to see the condition and perform biopsies of the lining of the colon.
If you don't already have a diagnosis of inflammatory bowel disease, you'll likely have a colonoscopy to test for ulcerative colitis, Crohn's disease or colitis. A colonoscopy also can reveal cancerous tumors or other irregular tissues in the colon. This exam also is part of regular monitoring after a diagnosis of PSC.
More Information
Treatment
There are no approved medical therapies that alter the natural history of PSC. Treatments for PSC focus on managing symptoms and complications and monitoring liver damage.
Ursodiol
Ursodiol, also called ursodeoxycholic acid, is a naturally occurring bile acid. For some people, low doses of ursodiol (Actigall, others) may result in signs of improved or more-stable liver function for a time. Ursodiol doesn't prevent disease complications or delay disease progression. Ursodiol may reduce itching.
Treatment for itching
- Antihistamines. Allergy medicines called antihistamines may help reduce mild itching. Because antihistamines can cause drowsiness, they may be good for people kept awake by itchiness.
- Bile acid sequestrants. Some medicines that bind to bile acids — the substances thought to cause itching in liver disease — are used to treat moderate to severe itching. These include cholestyramine (Locholest, Prevalite) and colestipol (Colestid). These medicines often cause constipation, cannot be used with several other medicines and may cause a vitamin K deficiency.
- Rifampin. Rifampin (Rifadin, Rimactane) is an antibiotic that may reduce moderate to severe itching. It may be used when bile acid sequestrants can't be used. Rifampin can cause liver inflammation, so blood tests are done regularly to test for side effects.
- Opioid antagonists. Naltrexone is an opioid agonist that may reduce moderate to severe itching. This medicine is typically used for treating alcohol use and opioid use disorders. Naltrexone can't be used if there is advanced liver disease.
Nutrition support
PSC makes it hard for your body to absorb certain vitamins. Even though you may eat a healthy diet, you may find that you can't get all the nutrients you need.
Your healthcare professional may recommend vitamin supplements that you take as tablets or that you receive as an infusion through a vein in your arm. If the disease weakens your bones, you may take calcium and vitamin D supplements as well.
Treatment for bile duct blockages
Blockages that occur in your bile ducts may be due to disease progression or may be a sign of bile duct cancer. Procedures with ERCP can open blocked ducts. The procedures include:
- Balloon dilation. This procedure can open blockages in the larger bile ducts outside the liver. In balloon dilation, your healthcare professional runs a slender tube with an inflatable balloon at its tip, called a balloon catheter, through an endoscope and into a blocked bile duct. Once the balloon catheter is in place, the balloon is inflated.
- Stent placement. In this procedure, your health professional uses an endoscope and attached instruments to place a small plastic tube called a stent in a blocked bile duct to hold the duct open. These stents often need to be replaced.
Treatment for infections
Bile that backs up in narrowed or blocked ducts often causes frequent bacterial infections. To prevent and treat these infections, people with PSC may need ERCP procedures. Also, they may take repeated courses of antibiotics or take antibiotics for long periods.
Liver transplant
Liver transplantation is the only treatment known to cure PSC. During a liver transplant, surgeons remove a diseased liver and replace it with a healthy liver from a donor.
However, not everyone with PSC needs a liver transplant. Many people live with PSC for years by managing symptoms and monitoring their liver health. A transplant is only considered when the condition becomes advanced, causing liver failure, repeated infections, bile duct blockages, severe itching or cancer that cannot be removed surgically.
Even then, healthcare professionals carefully weigh the risks and benefits. Some people with PSC never require a transplant, while others eventually do. For those who need it, outcomes are excellent. The survival rate after liver transplant is over 90% at one year and about 80% at five years. It's important to know that PSC can sometimes return even after a successful transplant.
Prognosis
Life expectancy with PSC can vary a lot from person to person. On average, people live about 10 to 20 years after diagnosis without a liver transplant, though some progress faster and others more slowly.
PSC often progresses unpredictably. Some people remain stable for years, while others develop complications such as liver failure, repeated infections or bile duct cancer more quickly. However, the survival rate after liver transplant is excellent.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Many people with PSC are able to live full and meaningful lives, especially in the early years after diagnosis. PSC often progresses slowly. With regular monitoring, symptom management and healthy lifestyle choices, people can continue work, family and daily activities.
Taking steps to care for your liver and manage your symptoms can make a difference:
- Don't drink alcohol.
- Get the hepatitis A and hepatitis B vaccinations.
- Use care with chemicals at home and at work.
- Eat a balanced diet with plenty of fruits, vegetables, whole grains and lean protein. Limit foods high in fat, sugar and salt. Exercise regularly. Maintain a healthy weight.
- Follow directions on all prescription and nonprescription medicines. Make sure your pharmacist and your healthcare professionals know that you have liver disease.
- Talk with your healthcare professional about any herbs or supplements you're currently taking since some can be harmful to your liver.
- Ask your healthcare team if you should add certain supplements to your diet. Because PSC can make it hard for the body to absorb nutrients, especially fat-soluble vitamins such as vitamins A, D, E and K, your care team may recommend vitamin supplements. If PSC weakens the bones, calcium also may be prescribed.
- To manage extreme tiredness, keep a regular sleep schedule. Do not drink caffeine in the afternoon and evening.
Alternative medicine
Alternative therapies may lessen pain and help cope with extreme tiredness linked to liver disease. These include acupuncture, yoga, meditation and massage.
Preparing for your appointment
A first appointment may be because of symptoms or because of the results of routine blood tests that show signs of poor liver function. Your primary healthcare professional may refer you to a digestive disease specialist, called a gastroenterologist, or a liver specialist, called a hepatologist.
Because appointments can be brief and because there's often a lot to talk about, it's a good idea to be prepared. Here's some information to help you get ready and what to expect from your healthcare professional.
What you can do
- Be aware of any pre-appointment restrictions. When you make your appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you take, the dose of each, and the reasons for taking them.
- Consider taking a family member or friend along. Sometimes it can be hard to remember all the information provided during an appointment. Someone who goes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare professional.
Your time with your health professional is limited. You may feel less rushed if you make a list of questions you want to ask at your appointment. Here are some possible questions for initial appointments or after a diagnosis:
- Can you explain my test results to me?
- Will I need more tests?
- How far has my PSC progressed?
- How serious is the damage to my liver?
- How will we know if I need a liver transplant?
- What treatments can relieve my signs and symptoms?
- What are the potential side effects of each treatment?
- Should I be tested for inflammatory bowel disease?
- What signs and symptoms signal that my condition is worsening?
- When should I make another appointment?
- Are there any restrictions that I need to follow?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
In addition to the questions that you've prepared, don't hesitate to ask questions that come up during your appointment.
What to expect from your doctor
Your healthcare professional is likely to ask you several questions. Being ready to answer them may allow more time later to cover points you want to talk about. Your health professional may ask:
- When did you begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- Do you have frequent bouts of diarrhea?
- Have you noticed blood in your stool?
- How much alcohol do you drink?
- What is your typical diet?
- What kind of exercise do you get?
Oct. 14, 2025