Diagnosis
Myelofibrosis diagnosis often starts with a physical exam. Other tests that can help diagnose this bone marrow cancer include blood tests and imaging tests. A healthcare professional may take a sample of your bone marrow for testing.
Physical exam
Your healthcare professional may ask about your symptoms and examine your body. The health professional might feel your belly to check for signs of swelling in the spleen and liver.
Blood tests
A healthcare professional might take a sample of blood for testing. One blood test used for myelofibrosis is a complete blood count. This test counts the number of cells in a sample of blood. In people with myelofibrosis, this test often finds low numbers of red blood cells. White blood cell and platelet counts may be higher or lower than expected.
Imaging tests
Imaging tests make pictures of the inside of the body. For myelofibrosis, a healthcare professional might use the pictures to see whether the spleen and liver are larger than usual. They also may look for signs that scar tissue has replaced healthy tissue in the bone marrow. Imaging tests might include computerized tomography scans, also called CT scans, and magnetic resonance imaging scans, also called MRI scans.
Bone marrow aspiration and biopsy
Bone marrow exam
Bone marrow exam
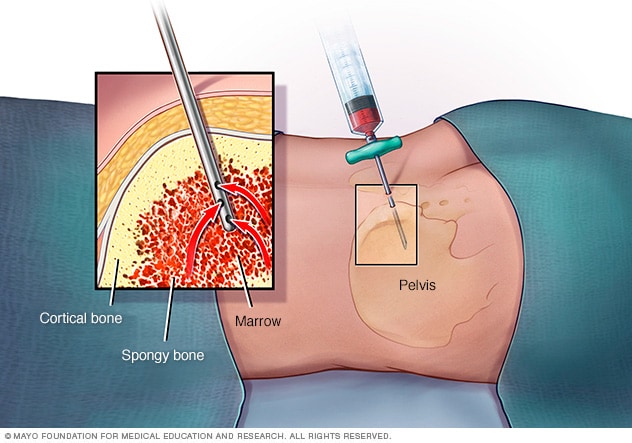
In a bone marrow aspiration, a healthcare professional uses a thin needle to remove a small amount of liquid bone marrow. It is usually taken from a spot in the back of the hip bone, also called the pelvis. A bone marrow biopsy is often done at the same time. This second procedure removes a small piece of bone tissue and the enclosed marrow.
Bone marrow aspiration and biopsy are procedures that involve collecting cells from the bone marrow. The cells are sent for testing.
Bone marrow has a solid part and a liquid part. In a bone marrow aspiration, a needle is used to draw a sample of the fluid. In a bone marrow biopsy, a needle is used to collect a small amount of the solid tissue and the enclosed fluid. The samples are typically taken from the hip bone.
In people with myelofibrosis, this test might find signs of scarring in the bone marrow.
Testing cancer cells for DNA changes
If concerning cells are found in the blood or bone marrow, these cells might be tested for changes in the DNA inside the cells. The genetic changes found in the DNA of your cancer cells can help your healthcare team make a diagnosis. The changes also might help your healthcare team make a treatment plan.
The genetic changes that are most common in myelofibrosis cells are called JAK2, CALR and MPL.
More Information
Treatment
Treatments for myelofibrosis include blood transfusions and medicines, such as chemotherapy and targeted therapy. Other treatments include surgery to remove the spleen, radiation therapy and bone marrow transplant, also called stem cell transplant.
The goal of treatment for most people with myelofibrosis is to provide relief from symptoms of the disease. For some, a bone marrow transplant, also called a stem cell transplant, may provide a chance for a cure. This treatment can be very hard on the body, and it might not be an option for many people.
To find out which myelofibrosis treatments are most likely to benefit you, your healthcare professional may use one or more formulas to assess your condition. These formulas take into account many aspects of your cancer and your overall health. A healthcare professional may assign a risk category that indicates how serious your condition is.
A lower risk myelofibrosis might grow slowly. Treatment might not be needed right away, or treatment might focus on controlling any symptoms. A higher risk myelofibrosis might be getting worse quickly. People with higher risk myelofibrosis might consider stronger treatments, such as a bone marrow transplant.
Treatment may not be needed right away
Myelofibrosis treatment might not be needed right away if you don't have any symptoms. Rather than giving you treatment, your healthcare professional may monitor your health closely through regular checkups and exams. Some people remain symptom-free for years.
Treatments for anemia
If myelofibrosis is causing severe anemia, your healthcare professional may recommend treatments such as:
- Blood transfusions.
- Medicines that increase blood cell production.
Treatments for an enlarged spleen
If an enlarged spleen is causing complications, your healthcare professional may recommend treatment. Your options may include:
- Targeted therapy. Targeted therapy for cancer is a treatment that uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die. For myelofibrosis, targeted therapy medicines attack cells with changes in the JAK2 gene.
- Chemotherapy. Chemotherapy treats cancer with strong medicines.
- Surgery to remove the spleen. Surgery to remove the spleen is called splenectomy. It might be used if other treatments don't help.
- Radiation therapy. Radiation therapy treats cancer with powerful energy beams. Radiation therapy can help reduce the size of the spleen. It might be used if surgery isn't an option.
Bone marrow transplant
A bone marrow transplant, also called a bone marrow stem cell transplant, involves putting healthy bone marrow stem cells into the body. These cells replace cells hurt by chemotherapy and other treatments.
For myelofibrosis, the healthy bone marrow stem cells come from a donor. A transplant using donor cells is called an allogenic stem cell transplant.
Before the transplant, you receive chemotherapy or radiation therapy treatments to destroy your bone marrow. The healthy stem cells from a donor are put in your body.
This treatment has the potential to cure myelofibrosis. It also has a high risk of life-threatening side effects. This treatment isn't an option for everyone with myelofibrosis.
Palliative care
Palliative care is a special type of healthcare that helps people with serious illnesses feel better. If you have cancer, palliative care can help relieve pain and other symptoms. A team of healthcare professionals gives palliative care. This can include doctors, nurses and other specially trained health professionals. Their goal is to improve quality of life for you and your family.
Palliative care specialists work with you, your family and your care team to help you feel better. They provide an extra layer of support while you have cancer treatment. You can have palliative care at the same time as strong cancer treatments, such as surgery, chemotherapy or radiation therapy.
When palliative care is used along with all of the other treatments, people with cancer may feel better and live longer.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
A myelofibrosis diagnosis can cause strong feelings. Some people say they felt shocked, scared or sad when they got their diagnosis. With time, each person finds a way to cope with these feelings. Until you find what works for you, here are some ideas to help you cope.
Learn enough about your condition to feel comfortable making decisions
Learn as much as you need to about myelofibrosis. Ask your healthcare team to recommend some good sources of information to get you started. As you learn more about your condition, you might feel more confident about making decisions about your care.
Find a good listener
Finding someone who is willing to listen to you talk about your hopes and fears can be helpful as you manage a cancer diagnosis. This could be a friend or family member. A counselor, medical social worker or clergy member also may offer helpful guidance and care.
Consider joining a support group, either in your community or on the internet. A support group of people with cancer can be a source of useful information, practical tips and encouragement.
Take time for yourself
If you have myelofibrosis, you may have a lot of medical appointments. Some days, you may feel sick even if you don't look sick. And some days, you may just be sick of having cancer.
Try to set aside time each day for something you enjoy. Find ways to relax. Some people have hobbies that help them take their minds off of cancer for a little while.
Preparing for your appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you. If your healthcare professional thinks that you have myelofibrosis, that person may refer you to a specialist. Often, this is a doctor who specializes in blood diseases, called a hematologist.
Appointments can be short and being prepared can help. Here's some information that may help you get ready.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test. Make a list of:
- Your symptoms, including any that don't seem related to the reason for your appointment.
- Key personal information, including major stresses, recent life changes and family medical history.
- All medications, vitamins or other supplements you take, including the doses.
- Questions to ask your doctor.
Take a family member or friend along, if possible, to help you remember the information you're given.
For myelofibrosis, some basic questions to ask your doctor include:
- Do I have cancer?
- Do I need more tests?
- What are my treatment options?
- What are the potential risks of these treatment options?
- Do any of the treatments cure my cancer?
- Can I have a copy of my pathology report?
- How much time can I take to consider my treatment options?
- Are there brochures or other printed materials that I can take with me? What websites do you recommend?
- What would happen if I chose not to have treatment?
Don't hesitate to ask other questions.
What to expect from your doctor
Your healthcare professional is likely to ask you several questions, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How bad are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, seems to worsen your symptoms?