Diagnosis
A prompt evaluation of your symptoms is vital to diagnose the cause of a transient ischemic attack. It also helps your healthcare professional determine the best treatment. To pinpoint the cause of the TIA and to assess your risk of a stroke, your healthcare professional may rely on the following:
-
Physical exam and tests. Your healthcare professional performs a physical exam and a neurological exam. Tests of your vision, eye movements, speech and language, strength, reflexes, and sensory system are included.
Your healthcare professional may use a stethoscope to listen to the carotid artery in your neck. During this exam, a whooshing sound called a bruit may mean that you have atherosclerosis. Or your healthcare professional may use an ophthalmoscope. This instrument looks for cholesterol fragments or platelet fragments called emboli in the tiny blood vessels of the retina at the back of the eye.
You also may be checked for risk factors of a stroke. These include high blood pressure, high cholesterol levels, diabetes and sometimes high levels of the amino acid homocysteine.
- Carotid ultrasonography. If your healthcare professional suspects that a narrowed carotid artery in the neck may be the cause of your TIA, you may need a carotid ultrasound. A wandlike device called a transducer sends high-frequency sound waves into the neck. The sound waves pass through the tissue and create images on a screen. The images can show narrowing or clotting in the carotid arteries.
- Computerized tomography (CT) or computerized tomography angiography (CTA) scans. CT scans of the head use X-ray beams to create a 3D image. This allows your healthcare professional to look at the brain or the arteries in the neck and brain. A CTA scan may involve an injection of a contrast material into a blood vessel. Unlike a carotid ultrasound, a CTA scan can look at blood vessels in the neck and head.
- Magnetic resonance imaging (MRI) or magnetic resonance angiography (MRA). These tests use a strong magnetic field to create a 3D view of the brain. MRA uses technology similar to MRI to look at the arteries in the neck and brain. But an MRA may include an injection of a contrast material into a blood vessel.
-
Echocardiography. This test may be done to find out if a heart issue caused fragments in the blood that led to a blockage. A traditional echocardiography is called a transthoracic echocardiogram (TTE). A TTE involves moving an instrument called a transducer across the chest to look at the heart. The transducer emits sound waves that bounce off different parts of the heart, creating an ultrasound image.
Or you may need another type of echocardiography called a transesophageal echocardiogram (TEE). A flexible probe with a transducer is placed into the tube that connects the mouth to the stomach, known as the esophagus. Because the esophagus is directly behind the heart, a TEE can create clearer, detailed ultrasound images. This allows a better view of some things, such as blood clots, that might not be seen clearly in a traditional echocardiography exam.
-
Arteriography. This procedure is used in some people to get a view of arteries in the brain not usually seen in an X-ray. A radiologist inserts a thin, flexible tube called a catheter through a small incision, usually in the groin.
The catheter is guided through the major arteries and into the carotid or vertebral artery in the neck. Then a dye is injected through the catheter. The dye allows the arteries to be seen on X-ray images.
More Information
Treatment
Once your healthcare professional learns the cause of the transient ischemic attack, the goal of treatment is to correct the issue and prevent a stroke. You may need medicines to prevent blood clots. Or you might need surgery.
Medicines
Several medicines may lower the risk of stroke after a TIA. Your healthcare professional recommends a medicine based on what caused the TIA, where it was located, its type and how bad the blockage was. Your healthcare professional may prescribe:
-
Anti-platelet drugs. These medicines make a circulating blood cell called platelets less likely to stick together. Sticky platelets begin to form clots when blood vessels are injured. Clotting proteins in blood plasma also are involved in the process.
Aspirin is the most commonly used anti-platelet medicine. Aspirin is also the least expensive treatment with the fewest potential side effects. An alternative to aspirin is the anti-platelet drug clopidogrel (Plavix).
Aspirin and clopidogrel may be prescribed together for about a month after the TIA. Research shows that taking these two medicines together in certain situations reduces the risk of a future stroke more than taking aspirin alone.
Sometimes both medicines are taken together for a longer period. This may be recommended when the cause of the TIA is a narrowing of a blood vessel in the head.
When there's a serious block of a major artery, the medicine cilostazol may be prescribed with aspirin or clopidogrel.
Alternatively, your healthcare professional may prescribe ticagrelor (Brilinta) and aspirin for 30 days to decrease your risk of recurrent stroke.
Your healthcare professional also may consider prescribing a combination of low-dose aspirin and the anti-platelet drug dipyridamole to reduce blood clotting. The way dipyridamole works is slightly different from aspirin.
- Anticoagulants. These medicines include heparin and warfarin (Jantoven). They lower the risk of blood clots by affecting clotting-system proteins instead of platelet function. Heparin is used for a short time and is rarely used in the management of TIAs.
These medicines require careful monitoring. If you have atrial fibrillation, your healthcare professional may prescribe a direct oral anticoagulant such as apixaban (Eliquis), rivaroxaban (Xarelto), edoxaban (Savaysa) or dabigatran (Pradaxa), which may be safer than warfarin due to lower bleeding risk.
Surgery
Carotid endarterectomy
Carotid endarterectomy
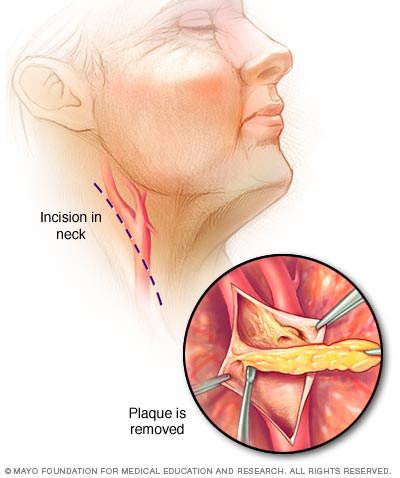
In carotid endarterectomy, a surgeon opens the carotid artery to remove the plaques that block it.
If the carotid artery in the neck is very narrowed, your healthcare professional may suggest a surgery called carotid endarterectomy (end-ahr-tur-EK-tuh-me). This preventive surgery clears carotid arteries of fatty deposits before another TIA or stroke can occur. An incision is made to open the artery, the plaques are removed, and the artery is closed.
Angioplasty
Some people need a procedure called carotid angioplasty and stent placement. This procedure involves using a balloon-like device to open a clogged artery. Then a small wire tube called a stent is placed into the artery to keep it open.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Preparing for your appointment
A transient ischemic attack often is diagnosed in an emergency situation. But if you're concerned about your risk of having a stroke, you can plan to talk about it with your healthcare professional at your next appointment.
What you can do
If you want to discuss your risk of a stroke with your healthcare professional, write down and be ready to discuss:
- Your risk factors for a stroke, such as family history of strokes.
- Your medical history, including a list of all medicines, as well as any vitamins or supplements, you're taking.
- Key personal information, such as lifestyle habits and major stressors.
- Whether you think you've had a TIA and what symptoms you experienced.
- Questions you might have.
What to expect from your doctor
Your healthcare professional may recommend that you have several tests to check your risk factors. You're given instructions on how to prepare for the tests, such as fasting before having your blood drawn to check your cholesterol and blood sugar levels.
Feb. 09, 2024