Diagnosis
Strokes FAQ Neurologist Robert D. Brown, Jr. M.D., M.P.H., answers the most frequently asked questions about strokes.
Hi, I'm Dr. Robert Brown, a neurologist at Mayo Clinic. And I'm here to answer some of the important question you may have about strokes.
The fast acronym, F.A.S.T., is a good way of remembering stroke symptoms and what to do if you or a friend or loved one experiences those symptoms. F for facial weakness, A for arm weakness, S for speech slurring, and T for time. Time to call 911 should those symptoms occur. Sometimes stroke symptoms may be temporary, lasting only several minutes or hours, and this is called a transient ischemic attack. The symptoms should not be ignored even if they are temporary. The risk of stroke is markedly increased in the days and weeks after those symptoms occur, so seek emergency evaluation to clarify why the symptoms occurred and how best to prevent a future stroke.
An aneurysm is a small saccular-shaped or berry-shaped out-pouching off of an artery in the brain. About two to three percent of the population has a brain aneurysm, and most never cause any symptoms. But on occasion, that aneurysm can rupture, leading to bleeding into and surrounding the brain, a bleeding type of stroke called a subarachnoid hemorrhage. People with that type of hemorrhage typically present with a sudden onset of a very severe headache, unlike anything they've ever experienced before, and they should seek emergency medical care.
The brain cells are affected very quickly after a stroke occurs. In the most common type of stroke, called an ischemic stroke, or cerebral infarction, there's a lack of blood flow to an area of the brain leading the brain cells to begin to die off due to a lack of oxygen and other nutrients. Emergency treatments can sometimes be used to restore the blood flow. Stroke treatments are most effective if they can be used early after stroke symptoms occur.
Most strokes are preventable. And stroke prevention is far more effective than trying to treat a stroke after it has occurred. There are both non-modifiable risk factors, those things we cannot change, and modifiable risk factors, those things that can be changed. Non-modifiable risk factors include age, race, gender, and family history of stroke. Modifiable risk factors include high blood pressure, high cholesterol levels, cigarette smoking, diabetes, obstructive sleep apnea, lack of regular exercise, obesity, heavy alcohol use, recreational drug use, and some types of heart disease.
Every stroke is a little bit different because any area of the brain can be affected by a stroke. Some strokes lead to only mild symptoms, and others are more severe and have a major impact on speech, strength, swallowing, walking, and vision. The patient with a stroke will typically start therapies very early after a stroke, including physical therapy, occupational therapy, and speech therapy. A person can continue to recover from a stroke for many months after a stroke up to a year or even longer. This recovery is a very gradual process. But don't give up. Celebrate the gains from week to week and month to month.
If you have any stroke risk factors, partner with your medical team to control them. If stroke symptoms occur, seek emergency care. Work with your medical team to arrange for the appropriate evaluation to clarify why the stroke happened, and institute strategies to prevent another stroke from occurring in the future. Take your medications as advised. Your medical team will also institute therapies to help you with any deficit that you might have related to your stroke so that you can live your life to the fullest after a stroke occurs. Thank you for your time and we wish you well.
During a stroke, things move quickly once you get to the hospital. Your emergency team works to learn what type of stroke you're having. You'll likely have a CT scan or other imaging test soon after arrival. Healthcare professionals also need to rule out other possible causes of your symptoms, such as a brain tumor or a drug reaction.
 Stroke consultation
Stroke consultation
Stroke consultation at Mayo Clinic
Tests
CT scan of brain tissue damaged by stroke
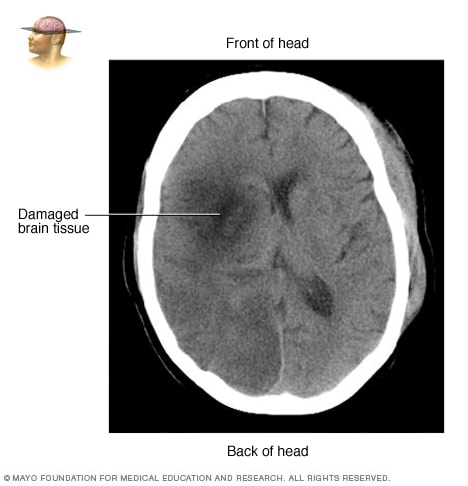
CT scan of brain tissue damaged by stroke
CT scan showing brain tissue damaged by stroke
Cerebral angiogram
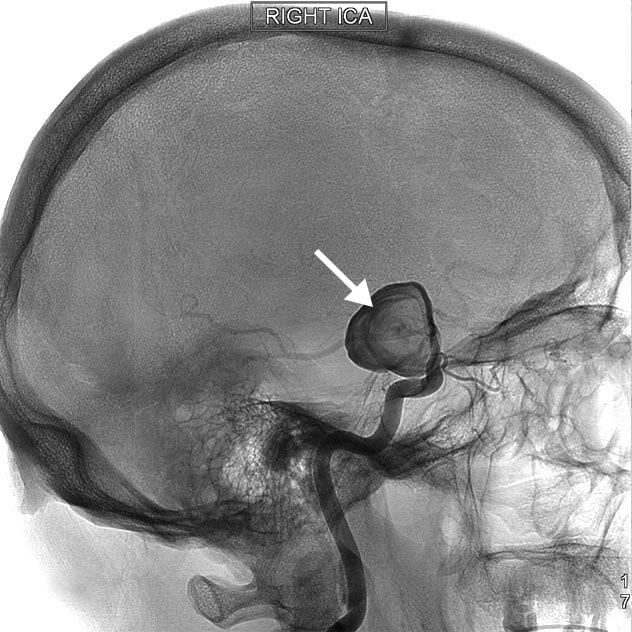
Cerebral angiogram
A cerebral angiogram showing a carotid aneurysm associated with stroke
Some of the tests you may have include:
- A physical exam. A healthcare professional does several tests, including listening to your heart and checking your blood pressure. A neurological exam looks at how a potential stroke is affecting your nervous system.
- Blood tests. You may need tests to check how fast your blood clots and whether your blood sugar is too high or low. You also may be tested to see if you have an infection.
- Computerized tomography (CT) scan. A CT scan uses a series of X-rays to create a detailed image of your brain. A CT scan can show bleeding in the brain, an ischemic stroke, a tumor or other conditions. You might have a dye injected into your bloodstream to view the blood vessels in the neck and brain in greater detail. This type of test is called a computerized tomography angiography.
- Magnetic resonance imaging (MRI). An MRI uses powerful radio waves and a magnetic field to create a detailed view of the brain. The test can detect brain tissue damaged by an ischemic stroke and brain hemorrhages. Sometimes a dye is injected into a blood vessel to view the arteries and veins and highlight blood flow. This test is called magnetic resonance angiography or magnetic resonance venography.
- Carotid ultrasound. In this test, sound waves create detailed images of the inside of the carotid arteries in the neck. A carotid ultrasound can show buildup of fatty deposits called plaques and blood flow in the carotid arteries.
- Cerebral angiogram. This test is less common, but it provides a detailed view of arteries in the brain and neck. A thin, flexible tube called a catheter is inserted through a small incision, usually in the groin. The tube is guided through the major arteries and into the carotid or vertebral artery in the neck. Then a dye is injected into the blood vessels to make the arteries visible under X-ray imaging.
- Echocardiogram. An echocardiogram uses sound waves to create detailed images of the heart. An echocardiogram can find a source of clots in the heart that may have traveled to the brain and caused a stroke.
More Information
Treatment
Emergency treatment depends on whether you're having an ischemic or hemorrhagic stroke. During an ischemic stroke, blood vessels in the brain are blocked or narrowed. During a hemorrhagic stroke, there's bleeding into the brain.
Ischemic stroke
To treat an ischemic stroke, blood flow must quickly be restored to the brain. This may be done with:
-
Emergency IV medicine. An IV medicine that can break up a clot has to be given within 4.5 hours from when symptoms began. The sooner the medicine is given, the better. Quick treatment improves your chances of survival and may reduce complications.
An IV injection of recombinant tissue plasminogen activator (TPA) is the gold standard treatment for ischemic stroke. The two types of TPA are alteplase (Activase) and tenecteplase (TNKase). An injection of TPA is usually given through a vein in the arm within the first three hours. Sometimes, TPA can be given up to 4.5 hours after stroke symptoms started.
This medicine restores blood flow by dissolving the blood clot causing the stroke. By quickly removing the cause of the stroke, it may help people recover more fully from a stroke. Your healthcare professional considers certain risks, such as potential bleeding in the brain, to determine whether TPA is appropriate for you.
- Emergency endovascular procedures. Healthcare professionals sometimes treat ischemic strokes directly inside the blocked blood vessel. Endovascular therapy has been shown to improve outcomes and reduce long-term disability after ischemic stroke. These procedures must be performed as soon as possible:
- Medicines delivered directly to the brain. During this procedure, a long, thin tube called a catheter is inserted through an artery in the groin. The catheter is moved through the arteries to the brain to deliver TPA directly where the stroke is happening. The time window for this treatment is somewhat longer than for injected TPA but is still limited.
- Removing the clot with a stent retriever. A device attached to a catheter can directly remove the clot from the blocked blood vessel in the brain. This procedure is especially helpful for people with large clots that can't be completely dissolved with TPA. This procedure often is performed in combination with injected TPA.
The time window when these procedures can be considered has been expanding due to newer imaging technology. Perfusion imaging tests done with CT or MRI help determine if that someone may benefit from endovascular therapy.
Other procedures
Your healthcare professional may recommend a procedure to open up an artery that is narrowed by plaque. This type of procedure is done to lower your risk of having another stroke or transient ischemic attack. Options vary, but include:
- Carotid endarterectomy. Carotid arteries are the blood vessels that run along each side of the neck, supplying the brain with blood. This surgery removes the plaque blocking a carotid artery and may reduce the risk of ischemic stroke. A carotid endarterectomy also involves risks, especially for people with heart disease or other medical conditions.
- Angioplasty and stents. In an angioplasty, a surgeon threads a catheter to the carotid arteries through an artery in the groin. A balloon is then inflated to expand the narrowed artery. Then a stent can be inserted to support the opened artery.
Hemorrhagic stroke
Emergency treatment of hemorrhagic stroke focuses on controlling the bleeding and reducing pressure in the brain caused by excess fluid.
Emergency measures
If you take blood-thinning medicines to prevent blood clots, you may be given treatment to counteract the blood thinners' effects. These treatments include medicines or a transfusion of blood products. Medicines also can lower the pressure in your brain, lower blood pressure, prevent spasms of the blood vessels and prevent seizures.
Surgery
If the area of bleeding is large, you may need surgery to remove the blood and relieve pressure on your brain. Surgery also may be used to repair blood vessel damage associated with hemorrhagic strokes.
Your healthcare professional may recommend one of these procedures if an aneurysm, arteriovenous malformation (AVM) or other blood vessel condition caused the stroke.
- Surgical clipping. A surgeon places a tiny clamp at the base of an aneurysm to stop blood flow to it. An aneurysm is a bulge at a weak spot in a blood vessel. The clamp can keep the aneurysm from bursting. Or the clamp can keep an aneurysm that has recently burst from bleeding again.
- Coiling, also known as endovascular embolization. A catheter is inserted into an artery in the groin and guided to the brain. Using the catheter, a surgeon places tiny coils into the aneurysm to fill it. This blocks blood flow into the aneurysm and causes blood to clot.
- Surgical removal of a tangle of thin-walled blood vessels, known as an AVM. Surgeons may remove a smaller AVM if it's in an area of the brain that's easy to access. This removes the risk of rupture and lowers the risk of hemorrhagic stroke. However, it's not always possible to remove an AVM if it's deep within the brain or if it's large. It also may not be possible to remove if the procedure would impact brain function.
- Stereotactic radiosurgery. This procedure uses multiple beams of highly focused radiation to repair blood vessel malformations. Stereotactic radiosurgery is an advanced treatment that's not as invasive as other procedures.
Stroke recovery and rehabilitation
Brain hemisphere connections
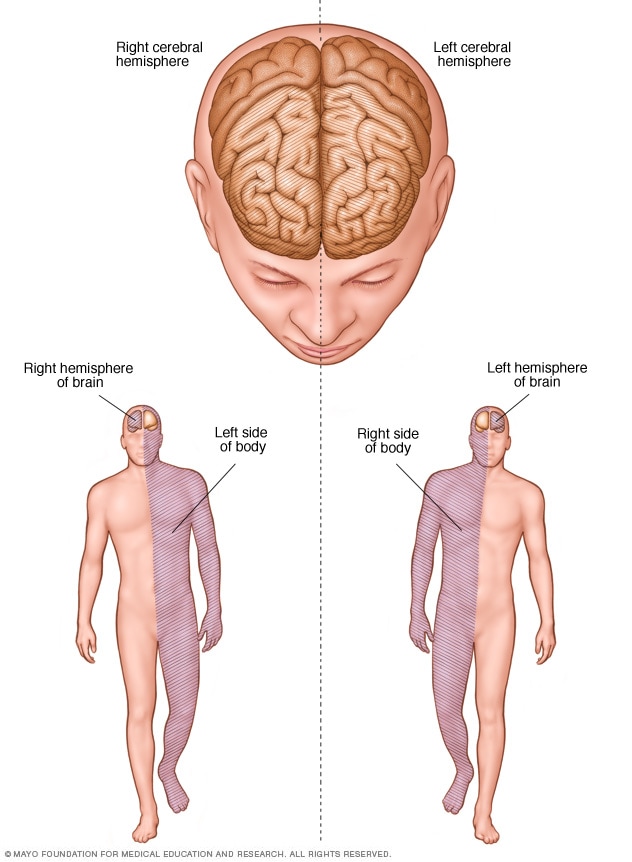
Brain hemisphere connections
After emergency treatment, you're closely monitored for at least a day. After that, stroke care focuses on helping you recover as much function as possible and to return to independent living. The impact of the stroke depends on the area of the brain involved and the amount of tissue damaged.
If the stroke affected the right side of the brain, movement and feeling on the left side of your body may be affected. If the stroke damaged the left side of the brain, movement and feeling on the right side of your body may be affected. Brain damage to the left side of the brain also may cause speech and language disorders.
Most people who have had a stroke go to a rehabilitation program. Your healthcare professional can recommend the therapy program that is right for you. A program is recommended based on your age, overall health and degree of disability from the stroke. Your lifestyle, interests, priorities and whether you have help from family members or caregivers are considered.
Rehabilitation may begin before you leave the hospital. After discharge, you might continue the program in a rehabilitation unit of the same hospital. Or you may go to another rehabilitation unit or to a skilled nursing facility as an outpatient. You also might have rehabilitation at home.
Every person's stroke recovery is different. Depending on your condition, your treatment team may include:
- Doctor trained in brain conditions, known as a neurologist.
- Rehabilitation doctor, known as a physiatrist.
- Rehabilitation nurse.
- Dietitian.
- Physical therapist.
- Occupational therapist.
- Recreational therapist.
- Speech pathologist.
- Social worker or case manager.
- Psychologist or psychiatrist.
- Chaplain.

Speech therapy is often a part of stroke rehabilitation.
More Information
Treatment outcomes
One way to evaluate the care of patients diagnosed with stroke is to look at the percentage of patients receiving the timely and effective care measures that are appropriate.
The graphs below display the percentage of eligible Mayo Clinic patients diagnosed with stroke receiving all of the appropriate care measures.
Stroke Core Measure
See related graph.
Carotid Endarterectomy Mortality
See related graph.
Carotid Stenting Mortality
See related graph.
Comprehensive Stroke Measure
See related graph.
Comprehensive Stroke – Arrival Time to Skin Puncture
See related graph.
Comprehensive Stroke – Post Thrombolysis Revascularization Rate
See related graph.
Comprehensive Stroke – Timeliness of IV t-PA Therapy
See related graph.
For additional information and data visit Medicare Hospital Compare.
For additional information about quality at Mayo Clinic visit Quality Measures.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
A stroke is a life-changing event that can affect your emotional well-being as much as your physical function. Some people may feel frustrated or depressed. A stroke may cause mood changes and a lower sex drive.
Maintaining your self-esteem, connections to others and interest in the world are essential parts of your recovery. Several strategies may help you and your caregivers, including:
- Don't be hard on yourself. Physical and emotional recovery involves tough work and takes time. Celebrate your progress. Allow time for rest.
- Join a support group. Meeting with others recovering from a stroke lets you get out and share experiences. You also can exchange information and build new friendships.
- Let friends and family know what you need. People may want to help, but they may not know what to do. Let them know how they can help. You might ask that they bring over a meal and stay to eat with you and talk. Or you might ask that they attend social events or religious activities with you.
Communication challenges
Speech and language can be hard after a stroke. Here are some tips to help you and your caregivers cope with communication challenges:
- Practice. Try to have a conversation at least once a day. It can help you learn what works best for you. It also can help you feel connected and rebuild your confidence.
- Relax and take your time. Talking may be easiest and most enjoyable in a relaxing situation when you're not rushed. Some people who have had a stroke find that after dinner is a good time for conversation.
- Say it your way. When you're recovering from a stroke, you may need to use fewer words. Rely on gestures or use your tone of voice to communicate.
- Use props and communication aids. You may find it helpful to use cue cards to communicate. Cue cards might include words used often. Or they might include pictures of close friends and family members, a favorite television show, the bathroom, or other wants and needs.
Preparing for your appointment
A stroke in progress is usually diagnosed in a hospital. If you're having a stroke, your immediate care focuses on reducing brain damage. If you haven't had a stroke but you're worried about your risk, talk to your healthcare professional at your next appointment.
What to expect from your doctor
In the emergency room, you may see an emergency medicine specialist or a doctor trained in brain conditions, known as a neurologist. Nurses and medical technicians also are likely to be involved in your care.
Your emergency team's first priority is to stabilize your symptoms and overall medical condition. Then the team determines if you're having a stroke. Healthcare professionals try to find the cause of the stroke to determine the proper treatment.
If you're seeking medical advice during a scheduled appointment, your healthcare professional considers your risk factors for stroke and heart disease. Your healthcare professional can offer advice on how to lower your risk. This may include lifestyle strategies, stopping smoking or not using illicit drugs. Your healthcare professional also may consider if you need medicines to control high blood pressure, cholesterol and other stroke risk factors.