Diagnosis
A diagnosis of Lynch syndrome often starts by reviewing a family's history of cancer. Depending on that family history, various tests and procedures may be used to diagnose Lynch syndrome.
Family history
Your healthcare professional may advise genetic testing for Lynch syndrome if one or more of the following are true for you:
- More than one blood relative had any cancer that could be linked to Lynch syndrome, including colon cancer or endometrial cancer. Other cancers caused by Lynch syndrome include those that affect the stomach, ovaries, pancreas, brain, small intestine, ureters, gallbladder, bile duct, bladder and skin, as well as cancer that affects the area at the center of the kidney, called the renal pelvis.
- One or more blood relatives had a type of cancer related to Lynch syndrome before age 50.
- One or more blood relatives have had more than one type of cancer related to Lynch syndrome.
- More than one generation of your family has had the same kind of cancer.
Testing cancer cells
If you or someone in your family has had cancer, a sample of the cancer cells may be tested for Lynch syndrome.
Tests on cancer cells include:
- Immunohistochemistry (IHC) testing. IHC testing uses dye to stain the cancer cells. The staining shows whether the cells have certain proteins. Missing proteins may help the care team see whether genes related to Lynch syndrome caused the cancer.
- Microsatellite instability (MSI) testing. Microsatellites are pieces of DNA. In people with Lynch syndrome, there may be errors or issues in microsatellites.
Positive IHC or MSI test results can show that the cancer cells have genetic changes that are connected to Lynch syndrome. But the results don't tell for sure whether you have Lynch syndrome. Some people have these genetic changes only in their cancer cells. This means the genetic changes weren't passed down within a family.
People with Lynch syndrome have a specific change in the gene that causes Lynch syndrome in all the cells in their bodies. Genetic testing is needed to see whether all the cells have this change.
Genetic testing
Genetic testing looks for changes in the genes that can cause Lynch syndrome. The testing is often done with a sample of blood. But sometimes, genetic testing may be done with a sample of saliva or by using a swab to collect tissue from inside the cheek, called a buccal swab.
If a family member has Lynch syndrome, genetic testing may look only for the gene that runs in the family. If you're the first person in your family to be tested for Lynch syndrome, the test may look at many genes associated with Lynch syndrome. A genetics professional can help decide which test is best for you.
Genetic testing may show:
-
A positive result. A positive genetic test result means a genetic change that causes Lynch syndrome was found in the cells. It doesn't mean you'll get cancer. But it does mean that your risk of some cancers is higher than it is in people who don't have Lynch syndrome.
Your risk of cancer also may depend on which Lynch-related gene runs in your family. A genetics professional can explain your risk based on the genetic test results.
- A negative result. A negative genetic test result means gene changes that cause Lynch syndrome weren't found in the cells. It means you probably don't have Lynch syndrome. But you could still have a higher risk of getting cancer. That's because people with a strong family history of cancer may have a higher risk of the disease.
- An unclear result. Genetic tests don't always give a yes or no answer. Sometimes, genetic testing finds a gene change that healthcare professionals aren't sure about. This is called a variant of unknown significance. A genetics professional can help you understand what this type of test result could mean for your health.
At-home genetic testing
There are no reliable at-home testing kits for Lynch syndrome. At-home DNA tests can provide information about ancestry or general health traits, but they can't reliably detect Lynch syndrome. These mail-in kits usually check only a few common genetic markers and don't include the detailed testing needed to find changes in the MLH1, MSH2, MSH6, PMS2 or EPCAM genes that cause Lynch syndrome.
For accurate results, genetic testing should be done through a healthcare professional or genetic counselor, who can order a medical-grade test from a certified laboratory and interpret the results correctly.
Treatment
Colonoscopy exam
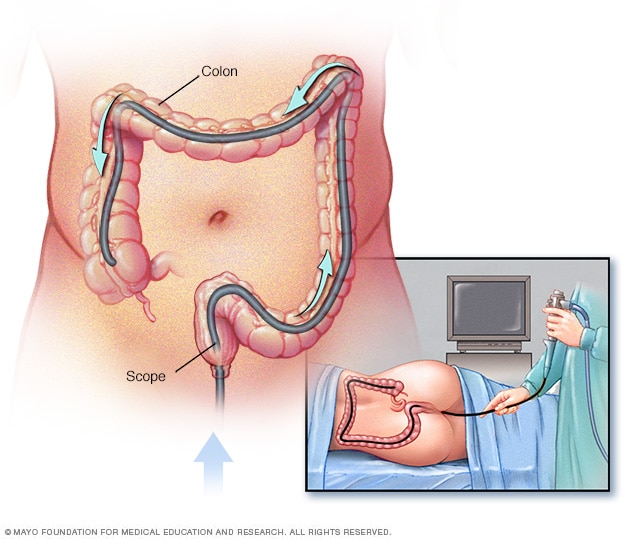
Colonoscopy exam
During a colonoscopy, a healthcare professional puts a colonoscope into the rectum to check the entire colon.
There's no cure for Lynch syndrome. People with Lynch syndrome often have tests to look for early signs of cancer. This is called cancer screening. If cancer is found early, when it's small, treatment is more likely to be successful. Sometimes the risk of cancer can be significantly lowered with surgery or other treatment.
Cancer screening
For people with Lynch syndrome, cancer screening tests are especially important because cancers can develop at a younger age and get worse more quickly than in the general population. The cancer screening tests you need depend on the Lynch syndrome gene you carry and what cancers run in your family.
| Cancer type |
Screening recommendations |
| Colon cancer |
People with Lynch syndrome should begin having colonoscopies at ages 20 to 25, or 2 to 5 years earlier than the youngest age at diagnosis of colorectal cancer in their family. Colonoscopies should be repeated every 1 to 2 years. A colonoscopy cannot diagnose Lynch syndrome, but it can find and remove growths before they become cancer. |
| Endometrial cancer |
Endometrial cancer is cancer that starts in the inside lining of the uterus. That lining is called the endometrium. Screening for endometrial cancer may begin at ages 30 to 35. An endometrial biopsy, which removes a small sample of the uterine lining, can be done every 1 to 2 years. Some experts also use ultrasound imaging to look for changes in the uterus. |
| Ovarian cancer |
Routine ovarian cancer screening has not been shown to save lives because it often misses early cancers and sometimes leads to false alarms or unnecessary surgery. |
| Stomach and small bowel cancer |
Screening with an upper endoscopy may begin between ages 30 to 40 and should be repeated every 2 to 4 years. Earlier testing may be considered if you have a family history of upper digestive cancers or high-risk factors, such as stomach polyps or Barrett's esophagus. |
| Urinary tract cancer |
An annual urine test to check for blood or other changes can begin at ages 30 to 35. This is particularly recommended for people with MSH2 variants or a family history of urinary tract cancers. |
| Pancreatic cancer |
People with several blood relatives who have had pancreatic cancer may consider screening with MRI or endoscopic ultrasound at a center that sees patients at high risk. Testing usually begins at age 50, or 10 years earlier than the youngest age at diagnosis in the family. |
| Skin cancer |
A skin exam should be done every 1 to 2 years by a healthcare professional familiar with sebaceous (oil gland) tumors. When to begin screening is decided based on each person's individual situation. |
| Brain cancer |
There is no set screening schedule for brain cancer in people with Lynch syndrome. Instead, you should watch for neurological symptoms such as persistent headache, vision changes, hearing loss, dizziness, trouble with balance, or weakness in the arms or legs. If these occur, you should see a healthcare professional right away. |
| Prostate cancer |
Men with Lynch syndrome have a risk of prostate cancer that is five times higher than that for men without Lynch syndrome. The use of annual prostate-specific antigen (PSA) testing is recommended beginning at age 40 for men with Lynch syndrome, particularly those with MSH2 or MSH6 mutations. |
| Breast cancer |
Current research hasn't shown a clear link between Lynch syndrome and an increased risk of breast cancer. However, some data suggest that women with MSH6 or PMS2 mutations may have a slightly higher risk. For now, experts agree that breast cancer screening should follow standard population guidelines based on a person's individual and family history, rather than on the presence of Lynch syndrome itself. |
Treatment to prevent cancer
In some situations, surgery or other treatment to reduce risk of cancer may be a good choice for people who have Lynch syndrome. Talk about the benefits and risks with your healthcare professional.
Treatment to reduce risk of cancer may be available for:
- Endometrial cancer. Surgery to remove the uterus is called a hysterectomy. It prevents endometrial cancer. Another option may be a procedure to place a birth control device in the uterus. The device, called an intrauterine device (IUD), releases a hormone that lowers the risk of endometrial cancer. An IUD also prevents pregnancy.
- Ovarian cancer. Surgery to remove the ovaries is called an oophorectomy. It greatly lowers the risk of ovarian cancer. Another option is taking oral contraceptives, also called birth control pills. Research suggests that taking birth control pills for at least five years lowers the risk of ovarian cancer.
- Colon cancer. Surgery to remove most or all of the colon is called a colectomy. It lowers the risk of colon cancer.
Aspirin for cancer prevention
Some research suggests that taking an aspirin every day may lower the risk of cancer in people with Lynch syndrome. Research shows that taking a baby aspirin daily is enough to help prevent colorectal cancer. Talk with your healthcare professional to decide whether taking aspirin could be a good choice for you.
Potential future treatments
There are no treatments that cure or reverse Lynch syndrome itself. This is because it is an inherited genetic condition. But researchers are studying new ways to prevent or treat cancers linked to Lynch syndrome:
-
Cancer vaccines. Scientists are developing vaccines that teach the immune system to recognize and attack cells that are not typical before they turn into cancer.
Early studies in people with Lynch syndrome show that these vaccines can safely trigger immune responses, but they are still being tested in clinical trials.
- Personalized or "precision" prevention. Researchers are learning that cancer risks vary depending on which Lynch-related gene is changed. Future care may use this genetic information to design prevention plans — such as when to start screening or how often to test — tailored to each person's exact gene mutation and family history.
Prognosis
People with Lynch syndrome have a higher chance of developing certain cancers at younger ages than most people, often before age 50. In the past, many were diagnosed only after symptoms appeared, leading to worse outcomes. Today, thanks to regular colonoscopies, endometrial screening and preventive surgeries, cancers are more often found early or prevented altogether. Most people who follow recommended care plans can expect a near-typical lifespan.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
Learning you have Lynch syndrome can be stressful and may cause worry about your future. Over time, most people find ways to cope. Here are some practical steps that may help.
Learn about Lynch syndrome
Gather information so you can make informed decisions about your care. Write down your questions and bring them to your appointments. Ask your healthcare team for reliable resources. The more you know, the more confident you may feel about managing your health.
Take care of yourself
Focus on healthy habits you can control:
- Eat a balanced diet.
- Exercise regularly.
- Don't smoke.
- Limit alcohol.
- Maintain a healthy weight.
- Keep up with all medical appointments, including cancer screenings.
Find support
Talk with someone you trust about your feelings. This could be a friend, family member, counselor, social worker or clergy member. Ask a member of your healthcare team about support groups in your area. And find support online through Mayo Clinic Connect, which is an online community where you can connect with others for support, practical information and answers to everyday questions about your condition.
Addressing common concerns
Having Lynch syndrome may raise questions about other parts of your life, including:
- Privacy. You may worry about how your diagnosis could affect your insurance or job. A genetics professional can explain your legal protections.
- Children. If you have children or plan to, a genetics professional can help you understand inheritance, discuss genetic testing, and guide you on how and when to talk with your children about Lynch syndrome.
- Family. Lynch syndrome affects families. A genetics professional can help you plan conversations with blood relatives about risks and testing options.
Preparing for your appointment
Make an appointment with a healthcare professional if you have any symptoms that worry you. If your healthcare professional thinks you could have Lynch syndrome, you may be referred to a genetics professional, such as a genetic counselor.
A genetics professional can help you decide whether genetic testing would be useful for you. If you choose to have genetic testing, a genetics professional also can help you understand your results.
What you can do
To get ready for a meeting with a genetics professional:
- Gather your medical records. If you've had cancer, bring your medical records to your appointment.
- Ask for information from family members who've had cancer. If family members have had cancer, ask for information about their diagnoses. Write down the types of cancer they had, types of treatment and ages at diagnosis.
- Take a family member or friend along, if possible. Sometimes it can be hard to remember all the information provided during an appointment. Someone who comes with you may remember something that you missed or forgot.
- Write down questions to ask your care team.
Questions to ask
Examples of questions to ask a genetics professional include:
- What causes Lynch syndrome?
- How is Lynch syndrome passed through families?
- If I have a family member with Lynch syndrome, what is the chance that I have the syndrome too?
- What types of tests are involved in genetic testing?
- What will the results of genetic testing tell me?
- How long can I expect to wait for my results?
- If my genetic test result is positive, what is the chance that I will get cancer?
- What tests can find cancers at an early stage?
- If my genetic test result is negative, does that mean I won't get cancer?
- Are genetic testing results ever wrong or not clear?
- What do my genetic test results mean for my family?
- How much does genetic testing cost?
- Will my insurance company pay for genetic testing?
- What laws protect me from discrimination if my genetic test result is positive?
- Is it OK to decide against genetic testing?
- If I choose not to have genetic testing, what does that mean for my future health?
- Are there brochures or other printed material that I can take with me? What websites do you suggest?
Be sure to ask any other questions that you may have.
What to expect
The genetics professional will likely ask questions about your health history and the health history of your family. Questions may include:
- Have you ever had cancer?
- Have members of your family had cancer?
- At what age was each family member with cancer diagnosed?
- Have any family members ever had genetic testing?
Dec. 02, 2025