Overview
The large intestine, including the colon, rectum and anus
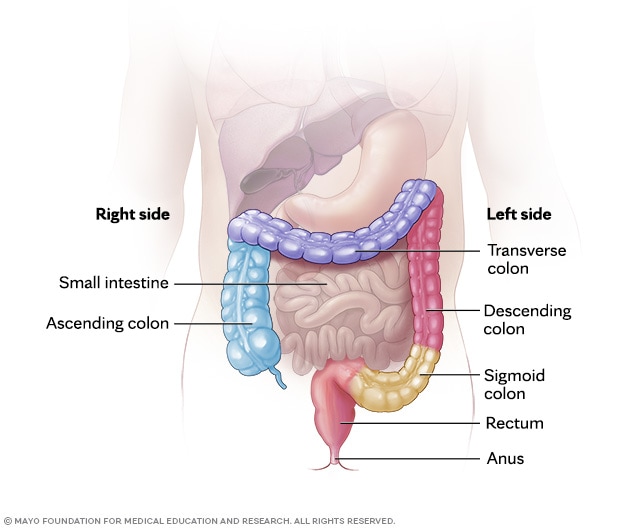
The large intestine, including the colon, rectum and anus
The entire large intestine includes the ascending colon, transverse colon, descending colon, sigmoid colon, rectum and anus.
Colectomy is a surgical procedure to remove all or part of your colon. Your colon, part of your large intestine, is a long tubelike organ at the end of your digestive tract. Colectomy may be necessary to treat or prevent diseases and conditions that affect your colon, including cancer, Crohn's disease, ulcerative colitis or diverticulitis. Colectomy also is known as colon resection.
Colectomy surgery usually requires an ostomy procedure, such as colostomy or ileostomy. An ostomy procedure involves reattaching the remaining portions of your digestive system to allow waste to leave your body.
Types
There are several types of colectomy procedures. The name depends on which part of the colon is removed. Surgeons choose the type based on the location of the disease. The most common types include:
- Right hemicolectomy. This surgery removes the ascending colon, and it sometimes includes the end of the small intestine and the beginning of the transverse colon. It is the most common type of colectomy.
- Left hemicolectomy. This surgery removes the left side of the colon. This usually includes the part of the colon from the middle of the transverse colon down through the descending colon, often ending at the upper rectum.
- Sigmoid colectomy, also known as sigmoidectomy. This surgery removes the sigmoid colon. This is the curved part that connects the colon to the rectum.
- Segmental resection. This surgery removes only a short, diseased segment of the colon. The two healthy ends are then sewn or stapled back together to restore bowel continuity.
- Low anterior resection. This surgery removes the upper part of the rectum and is often done for rectal cancer, with the goal of preserving the anus and bowel function.
- Abdominoperineal resection (APR). This surgery removes the sigmoid colon, rectum and anus. Because the anus is removed, a permanent colostomy is created to allow stool to leave the body.
- Total colectomy. This surgery removes the entire colon. The small intestine is then connected to the rectum to allow continued bowel movements through the anus.
- Proctocolectomy. This surgery removes both the colon and the rectum. In many cases, the end of the small intestine is brought out through the abdominal wall as an ileostomy to allow waste to pass into a bag. Sometimes, instead of a permanent ileostomy, the surgeon may create a pouch from the small intestine and connect it to the anus, allowing stool to pass through the anus as it typically would. This procedure is known as ileoanal anastomosis (J-pouch) surgery.
Products & Services
Why it's done
Colectomy is used to treat and prevent diseases and conditions that affect the colon, such as:
- Bleeding that can't be controlled. Severe bleeding from the colon may require surgery to remove the affected portion of the colon.
- Bowel obstruction. A blocked colon is an emergency that may require total or partial colectomy, depending on the situation.
- Colon cancer. If you have colon cancer, surgery to remove the cancer and nearby tissue may give you the best chance to cure the disease or keep it under control. Surgery also can help prevent problems such as bleeding, blockage or a hole in the colon that might happen if the cancer grows larger. Early-stage cancers may require only a small section of the colon to be removed during colectomy. Cancers at a later stage may require more of the colon to be removed.
- Crohn's disease. If medicines aren't helping you, removing the affected part of your colon may offer temporary relief from symptoms. Colectomy also may be an option if precancerous changes are found during a test to examine the colon, called colonoscopy.
- Ulcerative colitis. A total colectomy or proctocolectomy may be recommended if medicines aren't helping to control your symptoms. Proctocolectomy also may be recommended if precancerous changes are found during a colonoscopy.
- Diverticulitis. Surgery to remove the affected portion of the colon may be recommended if your diverticulitis recurs or if you experience complications of diverticulitis. Complications may include infection, blockage, a hole in the colon, or a tunnel that can form between the colon and nearby organs, called a fistula.
- Preventive surgery. If you have a very high risk of colon cancer due to the formation of multiple precancerous colon polyps, you may choose to undergo total colectomy to prevent cancer in the future. Colectomy may be an option for people with inherited genetic conditions that increase colon cancer risk, such as familial adenomatous polyposis or Lynch syndrome.
Discuss your treatment options with your healthcare team. In some situations, you may have a choice between various types of colectomy operations. Your care team can discuss the benefits and risks of each.
Risks
Colectomy carries a risk of serious complications. Your risk of complications is based on your general health, the type of colectomy you undergo and the approach your surgeon uses to perform the operation.
In general, complications of colectomy can include:
- Bleeding.
- Blood clots in the legs, called deep vein thrombosis, and the lungs, called pulmonary embolism.
- Infection.
- Injury to organs near your colon, such as the bladder and small intestines.
- Tears in the sutures that reconnect the remaining parts of your digestive system.
You'll spend time in the hospital after your colectomy to allow your digestive system to heal. Your healthcare team will monitor you for signs of complications from your surgery.
How you prepare
During the days leading up to your colon surgery, your healthcare team may ask that you:
- Stop taking certain medicines. Certain medicines can increase your risk of complications during surgery, so your healthcare team may ask that you stop taking those medicines before your surgery.
- Fast before your surgery. Your care team will give you specific instructions. You may be asked to stop eating and drinking several hours to a day before your procedure.
- Drink a solution that clears your bowels. You may be prescribed a laxative solution that you mix with water at home. You drink the solution over several hours, following the directions. The solution causes diarrhea to help empty your colon. Your care team also may recommend enemas.
- Take antibiotics. In some cases, you may be prescribed antibiotics to kill the bacteria found naturally in your colon and to help prevent infection.
Preparing for colectomy isn't always possible. For instance, if you need an emergency colectomy due to bowel obstruction or bowel perforation, there may not be time to prepare.
Plan for your hospital stay
You'll spend at least a few days in the hospital after your colectomy, depending on your situation. Make arrangements for someone to take care of your responsibilities at home and at work.
Think ahead to what you might like to have with you while you're recovering in the hospital. Things you might pack include:
- A robe and slippers.
- Toiletries, such as your toothbrush and toothpaste and, if needed, your shaving supplies.
- Comfortable clothes to wear home.
- Activities to pass the time, such as a book, magazine or games.
- Any medical devices you use at home, such as your CPAP machine for sleep apnea.
What you can expect
During your colectomy
Right hemicolectomy
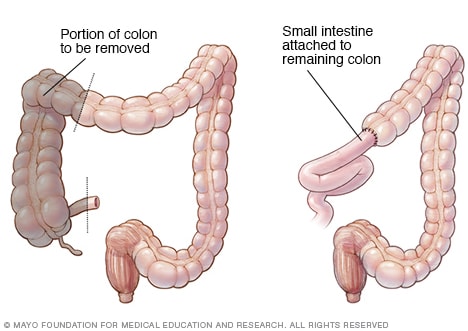
Right hemicolectomy
A colectomy procedure to remove one side of the colon is called hemicolectomy. A right hemicolectomy, as shown here, involves removing the right side of the colon and attaching the small intestine to the remaining portion of the colon.
Left hemicolectomy
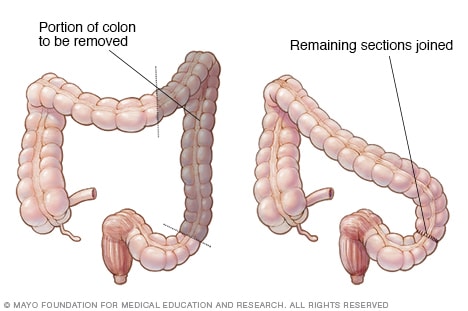
Left hemicolectomy
A colectomy procedure to remove one side of the colon is called hemicolectomy. A left hemicolectomy, as shown here, involves removing the left side of the colon and attaching the remaining parts of the colon.
Colostomy
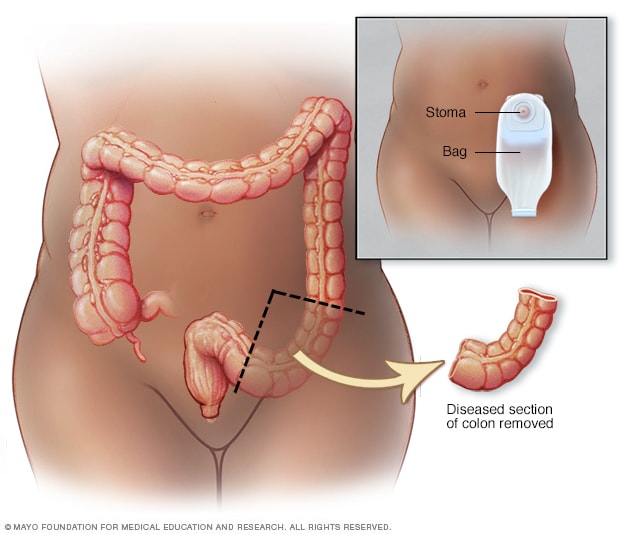
Colostomy
During colostomy surgery, an opening is made in the belly called a stoma. Part of the colon is brought through the stoma and attached to a pouch outside the body. Stools then pass through the stoma and go into the pouch.
Ileoanal anastomosis

Ileoanal anastomosis
After proctocolectomy to remove your colon and your rectum, your surgeon may connect your small intestine to your anus (ileoanal anastomosis). This allows you to expel waste normally, though you'll likely have several watery bowel movements daily.
On the day of your surgery, your healthcare team will take you to a preparation room. Your blood pressure and breathing will be monitored. You may receive antibiotic medicine through a vein in your arm.
You will then be taken to an operating room and positioned on a table. You'll be given a general anesthesia medicine to put you in a sleeplike state so that you won't be aware during your operation.
The surgical team will then proceed with your colectomy. Colon surgery may be performed in two ways:
- Open colectomy. Open surgery involves making a longer incision in your abdomen to access your colon. Your surgeon uses surgical tools to free your colon from the surrounding tissue and cuts out either a portion of the colon or the entire colon. An open colectomy usually takes several hours. The exact time depends on how much of the colon is removed and whether there are complications, such as scar tissue or bleeding.
-
Laparoscopic colectomy. Laparoscopic colectomy, also called minimally invasive colectomy, involves several small incisions in your abdomen. Your surgeon passes a tiny video camera through one incision and special surgical tools through the other incisions.
The surgeon watches a video screen in the operating room as the tools are used to free the colon from the surrounding tissue. The colon is then brought out through a small incision in your abdomen. This allows the surgeon to operate on the colon outside of your body. Once repairs are made to the colon, the surgeon reinserts the colon through the incision.
The type of operation you undergo depends on your situation and your surgeon's expertise. Laparoscopic colectomy may reduce the pain and recovery time after surgery. But not everyone is a candidate for this procedure. Also, in some situations your operation may begin as a laparoscopic colectomy, but circumstances may force your surgical team to convert to an open colectomy.
Once the colon has been repaired or removed, your surgeon will reconnect your digestive system to allow your body to expel waste. Options may include:
- Rejoining the remaining portions of your colon. The surgeon may sew the healthy ends of your colon together, or connect your small intestine to the rectum. This is called an anastomosis, and it allows stool to leave your body in the usual way.
- Connecting your intestine to an opening created in your abdomen. If it is not safe to reconnect the colon or rectum, the surgeon may create a small opening in the abdominal wall called a stoma. Waste leaves the body through the stoma into a bag worn on the outside. This is called an ostomy. Colostomy and ileostomy are common ostomy procedures performed along with colectomy. Colostomy and ileostomy may be temporary or permanent, depending on your condition.
- Connecting your small intestine to your anus. After removing both the colon and the rectum in a proctocolectomy, the surgeon may use part of your small intestine to create a pouch that is attached to your anus. This is called ileoanal anastomosis (J-pouch) surgery. J-pouch surgery allows you to pass waste through your anus as you typically would, though you may have several watery bowel movements each day. This typically improves over time.
Your surgeon will discuss your options with you before your operation.
After your colectomy
After surgery you'll be taken to a recovery room to be monitored as the anesthesia wears off. Then your healthcare team will take you to your hospital room to continue your recovery.
You'll stay in the hospital until your bowel function returns, which usually takes a few days. During this time your team will monitor pain, bowel function and any signs of complications before you are discharged to continue healing at home.
Here is what most people can expect while recovering over the next few days and weeks:
- Pain management. Pain at the incision sites is typical. Medicines are given to keep pain under control.
- Activity. You'll likely be encouraged to start moving and walking as soon as possible, since activity helps prevent blood clots and pneumonia. Most people slowly return to usual activities in 1 to 2 weeks. These activities include working, driving, showering and walking up stairs.
- Bowel function. It usually takes 3 to 4 days before the bowel starts working again, allowing you to pass gas or stool and begin eating as you typically would. At first, bowel movements may be more frequent or looser, but this often improves as the colon adjusts.
- Diet. Clear liquids are typically started soon after surgery, and solid foods are added gradually. You may need to avoid very fatty or high-fiber foods at first, especially if you experience diarrhea or cramping.
- Fatigue. Feeling weak or tired is common for several weeks. The body needs time to regain strength after major surgery.
- Incision and wound care. The surgical sites need to be kept clean and watched for redness, drainage, swelling or fever, which can signal infection.
- Ostomy care. If your surgery involved a colostomy or ileostomy to attach your intestine to the outside of your abdomen, you'll meet with an ostomy nurse who will show you how to care for your stoma. The nurse will explain how to change the ostomy bag that will collect waste.
Results
After colectomy surgery, expect a couple of weeks of recovery at home. You may feel weak at first, but eventually your strength will return. Ask your healthcare team when you can expect to know the results of the procedure.
Your outcomes after colectomy depend mostly on the underlying disease being treated and its severity. For many people, colectomy surgery prevents dangerous complications or removes cancer, which can protect or even extend life.
If surgery was for colon cancer, you will need regular follow-up colonoscopies and imaging tests. This helps catch any recurrence or new cancers early.
Oct. 07, 2025