- Symptoms & causes
Colon cancer symptoms & causes
This is Mayo Clinic’s guide to colon cancer — a cancer that starts in the large intestine. Find out about symptoms, causes and more.
Medical review by Mayo Clinic Staff
Updated: April 14, 2025
Overview
Colon cancer is a growth of cells that begins in a part of the large intestine called the colon. The colon is the first and longest part of the large intestine. The large intestine is the last part of the digestive system. The digestive system breaks down food for the body to use.
Colon cancer typically affects older adults, though it can happen at any age. It usually begins as small clumps of cells called polyps that form inside the colon.
Colon polyps can take a long time to grow before they become cancerous, often 10 to 15 years. Polyps often don’t cause symptoms. Though not all polyps turn into cancer, certain types have a higher risk. For this reason, healthcare professionals recommend regular screening tests to look for polyps in the colon. Finding and removing polyps helps prevent colon cancer.
If colon cancer develops, many treatments can help control it or even cure it. Treatments include surgery, radiation therapy and medicines, such as chemotherapy, targeted therapy and immunotherapy.
Colon cancer sometimes is called colorectal cancer. This term combines colon cancer and rectal cancer, which is cancer that starts in the rectum.
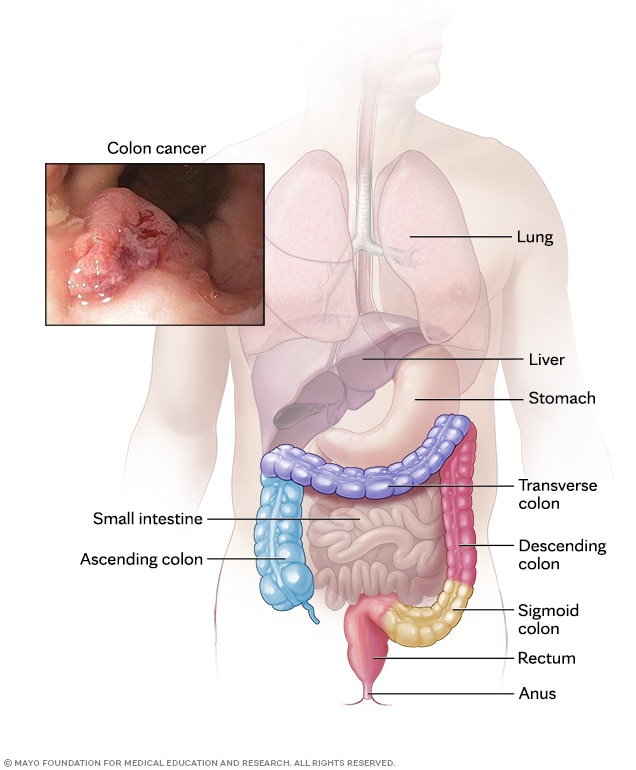
Colon cancer usually begins as small clumps of cells called polyps that form inside the colon. An exam of the whole colon using a long, flexible tube with a camera is one way to find polyps. This exam is called a colonoscopy.
Symptoms
Symptoms in early-stage colon cancer
Early-stage colon cancers are generally small cancers that are only in the colon. Many people with these cancers have no symptoms. That is why routine screening tests are so important. These tests often detect disease before symptoms develop, highlighting their importance in early diagnosis and effective treatment.
Symptoms in later stage colon cancer
In later stages of colon cancer, the cancer may have grown beyond the colon, possibly invading nearby tissues or lymph nodes. It also may have spread to distant organs and the lining of the abdominal cavity. This lining is called the peritoneum.
Because colon cancer symptoms can look like symptoms of other common health issues, such as hemorrhoids or stomachache, the symptoms may be easy to miss or mistake for something else. By the time symptoms become more noticeable, the cancer may be more advanced.
Symptoms often depend on the cancer’s size and where it is in the large intestine. Symptoms of colon cancer can include:
- A change in bowel habits, such as more-frequent diarrhea, constipation or changes in stool shape.
- Rectal bleeding or blood in the stool.
- Iron deficiency anemia, which can cause tiredness, weakness and a change in skin color.
- Ongoing discomfort in the belly area, such as cramps, gas, bloating or pain.
- Feeling full soon after eating.
- A feeling that the bowel doesn’t empty all the way during a bowel movement.
- Losing weight without trying.
- Swollen lymph nodes above the collarbone.
- A lump in the belly button area.
- Pain in the back, buttocks or legs.
Symptoms in people under 50 years old
There’s been an increase in younger people getting colon cancer, and the reason for this is not clear. Common symptoms in early-onset colon cancer may include:
- Blood in the stool.
- Belly pain.
- A change in bowel habits, such as constipation, diarrhea or alternating between the two.
- Losing weight without trying.
Symptoms based on cancer location
Colon cancer symptoms may differ depending on cancer location:
- Left-sided cancers. Left-sided cancers include those in the descending colon, sigmoid colon and about one-third of the transverse colon. These cancers are more likely to cause bowel habit changes and blood in the stool.
- Right-sided cancers. Right-sided cancers include those in the cecum, ascending colon and about two-thirds of the transverse colon. They are less common than are left-sided colon cancers. These cancers often cause iron deficiency anemia due to slow blood loss. Signs of right-sided colon cancer may include feeling tired and weight loss.
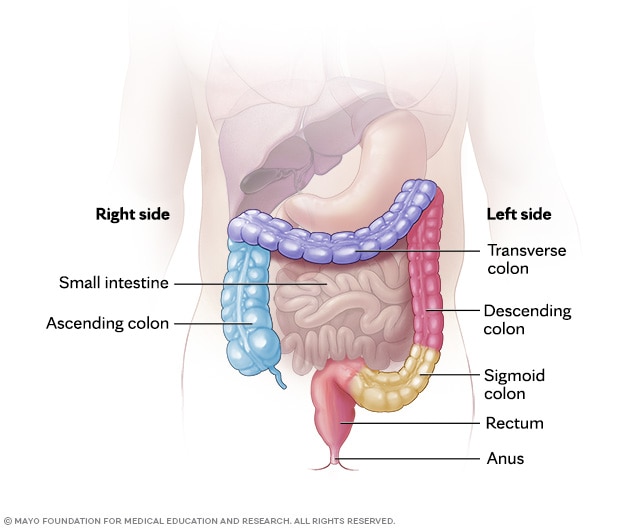
Colon cancer can develop in any part of the colon, including the ascending (right side), transverse, descending and sigmoid (left side) segments. Cancer can also grow in the rectum and, more rarely, the anus, areas that are part of the lower digestive tract.
When to see a doctor
Regular screening is essential because early colon cancer often has no symptoms. If you notice lasting symptoms that worry you, see a healthcare professional and have them checked out.
Colon cancer care at Mayo Clinic
Our team is standing by to help you schedule a colon cancer appointment.
Causes
The cause of most colon cancers isn’t clear. Researchers do know that colon cancer can have a genetic link, with certain inherited syndromes greatly increasing risk. But most colon cancers appear to be caused by environmental and lifestyle factors that may affect cells in the colon.
Colon cancer happens when the cells in the colon develop changes in their DNA. A cell’s DNA holds the instructions that tell the cell what to do. The changes tell the cells to multiply quickly. The changes let the cells continue living when healthy cells die as part of their natural life cycle.
This causes too many cells to grow. Uncontrolled cell growth may lead to the formation of small, noncancerous masses called polyps. While most polyps stay noncancerous, some can develop into colon cancer. There are a few different types of polyps. Adenomas, or adenomatous polyps, are the type of polyp most commonly associated with colon cancer. When an adenomatous polyp becomes cancerous it’s called an adenocarcinoma.
Cancer cells can invade and destroy healthy body tissue. If a cancerous polyp isn’t removed, it can lead to a larger growth that might grow deeper into the layers of the colon wall. With time, cancer cells can break away and spread. They may spread to nearby lymph nodes or to distant organs. When cancer spreads, it’s called metastatic cancer.
Risk factors
Factors that may increase the risk of colon cancer include:
Factors you can’t control
- Your age. Colon cancer can happen at any age. But most people with colon cancer are older than 50. The number of people younger than 50 who have colon cancer has been growing. Researchers don’t know why. About 10% of colon cancers are diagnosed in people before age 50 and only 1% before age 35.
- Your race. American Indian and Alaska Native people have the highest rates of colon cancer in the United States, followed by Black men and women. The risk is also higher for those of Ashkenazi Jewish descent.
Your sex. Colon cancer is more common in men than in women. This may be due to a variety of factors, such as diet, alcohol use, smoking and body fat distribution. Men tend to eat more red meat, smoke and drink more alcohol than women do. Men also have a greater tendency to store fat within their belly, called visceral fat. Visceral fat is associated with increased risk of colon cancer.
Some data suggests that women who have colon cancer are more likely to have right-sided colon cancer, especially if they no longer have periods due to menopause.
- A personal history of colorectal cancer or polyps. Having had colon cancer or colon polyps increases the risk of colon cancer.
- Inflammatory bowel disease. Conditions that cause pain and swelling of the intestines, called inflammatory bowel disease, can increase the risk of colon cancer. These conditions include ulcerative colitis and Crohn’s disease.
Inherited genes that increase colon cancer risk. Some genetic changes that increase the risk of colon cancer run in families. The most common inherited syndromes that increase colon cancer risk are Lynch syndrome and familial adenomatous polyposis, also called FAP.
FAP is a rare, inherited condition that causes polyps to form in the colon. In Lynch syndrome, genes involved in DNA repair don’t work as they should. Lynch syndrome used to be called hereditary nonpolyposis colorectal cancer. Many other genetic conditions are associated with colon cancer, including MUTYH-associated polyposis, juvenile polyposis syndrome, Cowden disease and Peutz-Jeghers syndrome.
But while some colon cancers can have a genetic component, most do not. Genetic conditions account for about 5% of colon cancers. Most colon cancers likely are caused by a combination of environmental and lifestyle factors.
- Family history of colon cancer. Having a blood relative who has colon cancer increases the risk of getting colon cancer. Having more than one family member who has colon cancer or rectal cancer increases the risk more.
- Radiation therapy for cancer. Radiation therapy directed at the abdomen to treat previous cancers increases the risk of colon cancer.
Factors you can control
- Diet. Colon cancer and rectal cancer might be linked with a typical Western diet. This type of diet tends to be low in fiber and high in sugar, fat and calories. Research in this area has had mixed results. Some studies have found an increased risk of colon cancer in people who eat a lot of red meat and processed meat. Other studies have found that long-term consumption of sugary drinks may be linked to higher rates of colon cancer.
- Not exercising regularly. People who are not active are more likely to develop colon cancer. Getting regular physical activity might help lower the risk.
- Diabetes. People with diabetes or insulin resistance have an increased risk of colon cancer.
- Obesity. People with obesity have an increased risk of colon cancer. Obesity also increases the risk of dying of colon cancer.
- Smoking. People who smoke can have an increased risk of colon cancer.
- Drinking alcohol. Drinking too much alcohol can increase the risk of colon cancer.
Possible risk factors that need more research
Researchers continue to study possible risk factors for colon cancer. More research needs to be done before these factors can be confirmed or ruled out:
- Seed oils. A recent study links ultraprocessed foods containing seed oils, such as corn, canola and soybean oils, to a higher risk of colon cancer. High in omega-6 fatty acids, these oils may promote inflammation in colon cells, potentially boosting cancer growth. However, more research is needed to prove this directly leads to colon cancer.
- Constipation. The relationship between constipation and colon cancer is complex, and current research provides mixed results. While some studies suggest a potential link, others find no significant association.
- Diverticulitis. Recent research suggests that diverticulitis is associated with an increased risk of colon cancer, particularly right after diagnosis. But while these findings highlight an association, they do not prove that diverticulitis causes colon cancer. Further research is needed to fully understand the relationship between diverticulitis and colon cancer.
- Anal sex. No direct evidence links anal sex to colon cancer. Certain factors associated with anal sex, such as exposure to the human papillomavirus, also called HPV, may increase the risk of anal cancer. But anal cancer is different from colon cancer. So far, the relationship between HPV and colon cancer has been explored but not proved.
Prevention
Screening for colon cancer
Healthcare professionals recommend that people with an average risk of colon cancer start colon cancer screening around age 45. People with an increased risk may want to start screening sooner. People with an increased risk include those with a family history of colon cancer.
Several different tests are used for colon cancer screening. Talk about your options with your healthcare team.
Related
“If we’re able to detect the colon polyps at a small and early stage, and resect them completely, we can actually prevent colon cancer from developing in the first place.”

Johanna Chan, M.D.
Mayo Clinic gastroenterologist
Lifestyle changes to reduce the risk of colon cancer
Making changes in everyday life can reduce the risk of colon cancer. To lower the risk of colon cancer:
- Eat a variety of fruits, vegetables and whole grains. Fruits, vegetables and whole grains have vitamins, minerals, fiber and antioxidants, which may help prevent cancer. Choose a variety of fruits and vegetables so that you get a range of vitamins and nutrients.
- Limit red and processed meats. Eat no more than three servings of red meat a week. That’s about 12 to 18 ounces (340 to 510 grams) total for the week. Eat little, if any, processed meats.
- Drink alcohol in moderation, if at all. If you choose to drink alcohol, limit the amount you drink to no more than one drink a day for women and two for men.
- Stop smoking. Talk to your healthcare team about ways to quit.
- Exercise most days of the week. Try to get at least 30 minutes of exercise on most days. If you’ve been inactive, start slowly and build up gradually to 30 minutes. Also, talk with a healthcare professional before starting an exercise program.
- Maintain a healthy weight. If you are at a healthy weight, work to maintain your weight by combining a healthy diet with daily exercise. If you need to lose weight, ask your healthcare team about healthy ways to achieve your goal. Aim to lose weight slowly by eating fewer calories and moving more.
Colon cancer prevention for people with a high risk
Some medicines can reduce the risk of colon polyps or colon cancer. For instance, some evidence links a reduced risk of polyps and colon cancer to regular use of aspirin or aspirin-like medicines. But it’s not clear what dose and what length of time would be needed to reduce the risk of colon cancer. Taking aspirin daily has some risks, including ulcers and bleeding in the digestive system.
These options generally are reserved for people with a high risk of colon cancer. There isn’t enough evidence to recommend these medicines to people who have an average risk of colon cancer.
If you have an increased risk of colon cancer, discuss your risk factors with your healthcare team to see if preventive medicines are safe for you.
Support group discussions
From Mayo Clinic Connect, our online patient community.
Find more discussions:
Mayo Clinic’s approach to colon cancer
At Mayo Clinic, colon cancer experts treat all types of the disease — from the most common to the most complex. Our teams have created new and minimally invasive screenings, improved testing with AI technology, and found new treatments that are now used around the world.
If you or someone you care about has colon cancer symptoms, our team at Mayo Clinic is here to help. We know that regular screenings and finding cancer early give many patients the best outcomes. Diagnostic tests such as a colonoscopy can help you understand your symptoms and learn more about your risk for colon cancer.
You can also contact our helpful scheduling teams by calling:
Just diagnosed with colon cancer?
We’ve gathered resources and answers to common questions to help you get started on your path to recovery.
Associated procedures
News from Mayo Clinic
- Mayo Clinic Minute: Liver transplant for patients with advanced colorectal cancer
- Liver transplants offer new hope for colorectal cancer patients with liver metastasis
- Mayo Clinic Q and A: Colorectal cancer in young adults
- You're at risk of colorectal cancer. Know the symptoms. Get screened.
- (VIDEO) Treatment options for advanced colorectal cancer
- Mayo Clinic Minute: Warning signs of colorectal cancer in younger adults
- Mayo Clinic researchers identify proteins linked to immunotherapy resistance in metastatic colorectal cancer
- Mayo Clinic Minute: Are colon and rectal cancers treated differently?
- Mayo Clinic Q and A: Understanding colorectal cancer
- Clinical trials team brings hope and dedication to colorectal cancer study
- New gene markers detect Lynch syndrome-associated colorectal cancer, Mayo Clinic study
- Mayo Clinic researchers publish key findings about cell proteins to determine effectiveness of immunotherapy for colon cancer
- Goldman L, et al., eds. Neoplasms of the small and large intestine. In: Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Feb. 15, 2023.
- AskMayoExpert. Colorectal cancer (adult). Mayo Clinic; 2022.
- Rodriguez-Bigas, MA, et al. Overview of the management of primary colon cancer. https://www.uptodate.com/contents/search. Accessed Feb. 15, 2023.
- Colon cancer. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelinesdetail?category=1&id=1428. Accessed Feb. 8, 2023.
- NCCN guidelines for patients: Colon cancer. National Comprehensive Cancer Network. https://www.NCCN.org/patients. Accessed Feb. 14, 2023.
- Palliative care. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelinesdetail?category=3&id=1454. Accessed Feb. 8, 2023.
- Ami TR. Allscripts EPSi. Mayo Clinic. Feb. 1, 2023.
- Colorectal cancer. American Cancer Society. https://www.cancer.org/cancer/types/colon-rectal-cancer.html. Accessed March 11, 2025.
- Do I have colorectal cancer? Signs, symptoms and work-up. American Cancer Society. https://www.cancer.org/cancer/latest-news/signs-and-symptoms-of-colon-cancer.html. Accessed March 11, 2025.
- White A, et al. A review of sex-related differences in colorectal cancer incidence, screening uptake, routes to diagnosis, cancer stage and survival in the UK. BMC Cancer. 2018; doi:10.1186/s12885-018-4786-7.
- Macrae FA, et al. Clinical presentation, diagnosis, and staging of colorectal Cancer. https://www.uptodate.com/contents/search. Accessed March 11, 2025.
- Demb J, et al. Red flag signs and symptoms for patients with early-onset colorectal cancer: A systematic review and meta-analysis. JAMA Network Open. 2024; doi:10.1001/jamanetworkopen.2024.13157.
- Odze RD, et al., eds. Epithelial neoplasms of the large intestine. In: Odze and Goldblum Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas. 4th ed. Elsevier; 2023. https://www.clinicalkey.com. Accessed March 11, 2025.
- Limit consumption of red and processed meat. American Institute for Cancer Research. https://www.aicr.org/cancer-prevention/recommendations/limit-consumption-of-red-and-processed-meat. Accessed March 18, 2025.
- Genetics of colorectal cancer (PDQ) – Health professional version. National Cancer Institute. https://www.cancer.gov/types/colorectal/hp/colorectal-genetics-pdq. Accessed March 18, 2025.
- Joh HK, et al. Simple sugar and sugar-sweetened beverages intake during adolescence and risk of colorectal cancer precursors. Gastroenterology. 2021; doi:10.1053/j.gastro.2021.03.028.
- Staller K, et al. Chronic constipation as a risk factor for colorectal cancer: Results from a nationwide, case-control study. Clinics in Gastroenterology and Hepatology. 2022; doi:10.1016/j.cgh.2021.10.024.
- Soundararajan R, et al. Integration of lipidomics with targeted, single cell, and spatial transcriptomics defines an unresolved pro-inflammatory state in colon cancer. Gut. 2025; doi:10.1136/gutjnl-2024-332535.
- Hsu CH, et al. Human papillomavirus and risk of colorectal cancer: An analysis of nationwide claims data. Medicina; 2022; doi:10.3390/medicina58101461.
- Ambrosio MR, et al. Immune landscape and oncobiota in HPV‑associated colorectal cancer: An explorative study. Clinical and Experimental Medicine. 2023; doi:10.1007/s10238-023-01165-3.
- Mortensen LQ, et al. Diverticulitis is associated with increased risk of colon cancer: A nationwide register-based cohort study. Journal of Clinical Medicine. 2024; doi:10.3390/jcm13092503.
- Symptoms of colorectal cancer. Canadian Cancer Society. https://cancer.ca/en/cancer-information/cancer-types/colorectal/signs-and-symptoms. Accessed March 13, 2025.
- Doubeni C. Tests for screening for colorectal cancer. https://www.uptodate.com/contents/search. Accessed March 11, 2025.
- Colorectal cancer screening: Where does the Shield liquid biopsy fit in? https://www.cancer.gov/news-events/cancer-currents-blog/2024/shield-blood-test-colorectal-cancer-screening. Accessed March 18, 2025.
- Colorectal cancer stages. American Cancer Society. https://www.cancer.org/cancer/types/colon-rectal-cancer/detection-diagnosis-staging/staged.html. Accessed Dec. 3, 2024.
- Stages of colorectal cancer. Colorectal Cancer Alliance. https://colorectalcancer.org/basics/stages-colorectal-cancer. Accessed Dec. 3, 2024.
- Treatment of colon cancer, by stage. https://www.cancer.org/cancer/types/colon-rectal-cancer/treating/by-stage-colon.html. American Cancer Society. Accessed Jan. 28, 2025.
- Colon and rectal cancer follow-up care expanded version. American Society of Colon and Rectal Surgeons. https://fascrs.org/patients/diseases-and-conditions/a-z/colon-and-rectal-cancer-follow-up-care-expanded-ve#. Accessed Feb. 5, 2025.
- Siegel RL, et al. Cancer statistics, 2024. CA: A Cancer Journal for Clinicians. 2024; doi:10.3322/caac.21820.
- Cancer stat facts: Colorectal cancer. National Cancer Institute. https://seer.cancer.gov/statfacts/html/colorect.html. Accessed Jan. 24, 2025.
- Colorectal cancer. American Cancer Society. https://www.cancer.org/cancer/types/colon-rectal-cancer.html. Accessed Jan. 24, 2025.
- Siegel RL, et al. Cancer statistics, 2024. CA: A Cancer Journal for Clinicians. 2024; doi:10.3322/caac.21820.
- Boyle T, et al. Lifestyle factors associated with survival after colorectal cancer diagnosis. British Journal of Cancer. 2013; doi:10.1038/bjc.2013.310.
- Alese OB, et al. Predictive and prognostic effects of primary tumor size on colorectal cancer survival. Frontiers in Oncology. 2021; doi:10.3389/fonc.2021.728076.
- Treatment of colon cancer, by stage. American Cancer Society. https://www.cancer.org/cancer/types/colon-rectal-cancer/treating/by-stage-colon.html. Accessed Jan. 28, 2025.
- Alwers E, et al. Smoking behavior and prognosis after colorectal cancer diagnosis: A pooled analysis of 11 studies. JNCI Cancer Spectrum. 2021; doi:10.1093/jncics/pkab077.
- Aeschbacher P, et al. Obesity and overweight are associated with worse survival in early-onset colorectal cancer. Surgery. 2024; doi:10.1016/j.surg.2024.03.037.
- Campbell AL, et al. Exercise guidelines for cancer survivors: Consensus statement from international multidisciplinary roundtable. Medicine & Science in Sports & Exercise. 2019; doi:10.1249/MSS.0000000000002116.
- Diet, nutrition, physical activity and body weight for people living with and beyond colorectal cancer. The latest evidence, our guidance for patients, carers and health professionals, and recommendations for future research. World Cancer Research Fund International. https://www.wcrf.org/diet-activity-and-cancer/global-cancerupdate-programme/cancer-survivors/. Accessed Feb. 5, 2025.
- Obesity and cancer. National Cancer Institute. https://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/obesity-fact-sheet. Accessed April 7, 2025.
- Symptoms & causes