Diagnosis
Diagnosing colon cancer
Colonoscopy exam
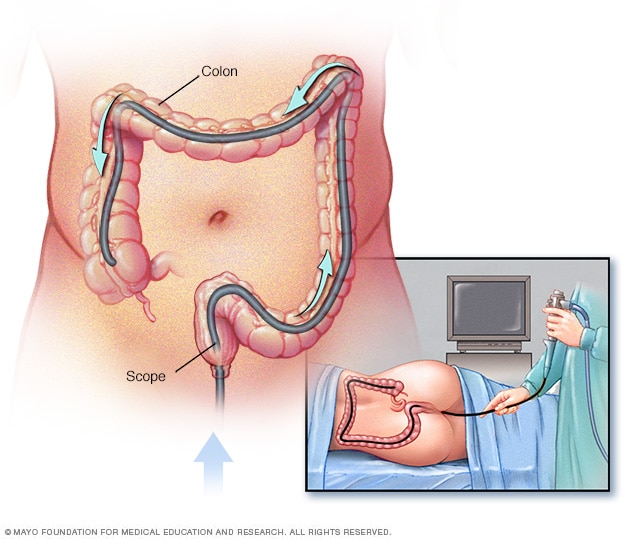
Colonoscopy exam
During a colonoscopy, a healthcare professional puts a colonoscope into the rectum to check the entire colon.
Tests and procedures used for colon cancer diagnosis include:
- Using a scope to examine the inside of the colon. Colonoscopy uses a long, flexible and slender tube attached to a video camera and monitor to view the whole colon and rectum. A doctor may pass surgical tools through the tube to take tissue samples and remove polyps.
- Removing a sample of tissue for testing. A biopsy is a procedure to remove a sample of tissue for testing in a lab. For colon cancer, the tissue sample is often collected during a colonoscopy. Sometimes surgery is needed to get the tissue sample. In the lab, tests can show whether the cells are cancerous and how quickly they're growing. Other tests can give more information about the cancer cells. Your health care team uses the results to understand your prognosis and create a treatment plan.
-
Blood tests. Blood tests aren't used to diagnose colon cancer. But blood tests can give clues about overall health, such as how well the kidneys and liver are working. A blood test might be used to look for a low level of red blood cells. This result might indicate that a colon cancer is causing bleeding.
Colon cancers sometimes make a protein called carcinoembryonic antigen, also called CEA. Blood tests can track the level of CEA over time. The results might show whether the cancer is responding to treatment. After treatment, CEA blood tests might detect if the cancer comes back.
Colon cancer stages
Colon cancer stages
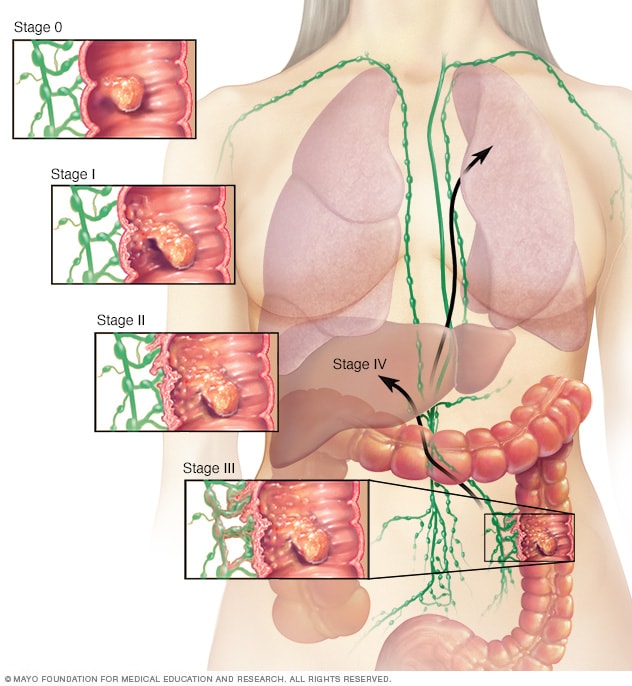
Colon cancer stages
The stages of colon cancer range from 0 to 4. At stage 0, the cancer only involves the inside the lining of the colon. As the cancer grows, it can go through the colon into nearby areas of the body. Stage 4 is the most advanced stage. At stage 4 the cancer has spread to other parts of the body, such as the liver or lungs.
After a colon cancer diagnosis, other tests might be needed to find out the extent of the cancer. This is called the cancer's stage. The health care team considers the cancer's stage when creating a treatment plan.
Staging tests might include imaging scans of the abdomen, pelvis and chest. Imaging tests take pictures of the body. They show the location and the size of the colon cancer. Often, doctors can't be certain of the cancer's stage until after colon cancer surgery.
Colon cancer stages range from 0 to 4. The lowest numbers mean the cancer is all inside the lining of the colon. By stage 4, the cancer is considered advanced and has spread to other areas of the body. When cancer spreads, it's called metastatic cancer.
More Information
Treatment
Colon cancer treatment usually involves surgery to remove the cancer. Your health care team might recommend other treatments, such as radiation therapy and chemotherapy. Your treatment options depend on the cancer's location and its stage. Your health care team also considers your overall health and your preferences when creating a treatment plan.
Surgery for early-stage colon cancer
Treatment for a very small colon cancer might be a minimally invasive approach to surgery, such as:
- Removing polyps during a colonoscopy, called a polypectomy. If the cancer is contained within a polyp, removing the polyp may remove all of the cancer.
- Endoscopic mucosal resection. This procedure can remove larger polyps during colonoscopy. Special tools help remove the polyp and a small amount of the lining of the colon.
- Minimally invasive surgery, called laparoscopic surgery. This type of surgery can remove polyps that can't be removed during a colonoscopy. In this procedure, a surgeon performs the operation through several small cuts called incisions in the abdominal wall. Instruments with attached cameras go through the cuts and show the colon on a video monitor. The surgeon also may take samples from lymph nodes in the area around the cancer.
Surgery for more advanced colon cancer
Colostomy
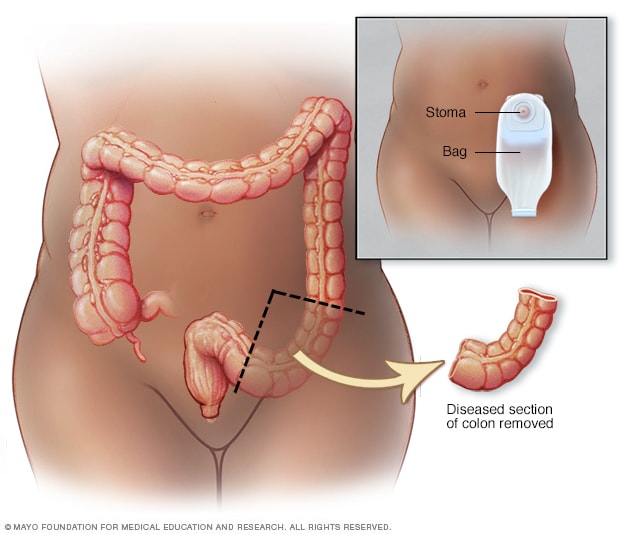
Colostomy
During colostomy surgery, an opening is made in the belly called a stoma. Part of the colon is brought through the stoma and attached to a pouch outside the body. Stools then pass through the stoma and go into the pouch.
If the cancer has grown into or through the colon, a surgeon might recommend:
- Partial colectomy. Surgery to remove part of the colon is called partial colectomy. During this procedure, the surgeon removes the part of the colon that has the cancer. The surgeon also takes some tissue on either side of the cancer. It's often possible to reconnect the healthy portions of the colon or rectum. This procedure can often be done by a minimally invasive approach called laparoscopy.
-
Surgery to create a way for waste to leave the body. Sometimes it's not possible to reconnect the healthy portions of the colon or rectum after colectomy. The surgeon creates an opening in the wall of the abdomen from a portion of what's left of the intestine. This procedure, called an ostomy, allows stool to leave the body by emptying into a bag that fits over the opening.
Sometimes the ostomy is only for a short time to let the colon or rectum heal after surgery. Then it's reversed. Sometimes the ostomy can't be reversed and stays for life.
- Lymph node removal. Nearby lymph nodes are usually removed during colon cancer surgery and tested for cancer.
Surgery for advanced cancer
When it's not possible to remove the cancer with surgery, a surgeon might try to relieve symptoms rather than cure the cancer. This surgery can remove colon blockages and ease symptoms, such as bleeding or pain.
Sometimes the cancer has spread only to the liver or lung in someone who is otherwise healthy. Surgery or other localized treatments might remove the cancer. Chemotherapy might be used before or after this type of procedure. This approach provides a chance to be free of cancer over the long term.
Chemotherapy
Chemotherapy uses strong medicines to kill cancer cells. Chemotherapy for colon cancer is usually given after surgery if the cancer is large or has spread to the lymph nodes. Chemotherapy can kill cancer cells that might be left after surgery. This helps reduce the risk of the cancer coming back.
Chemotherapy might also be used before surgery to shrink a large cancer so that it's easier to remove.
Chemotherapy also can be used to relieve symptoms of colon cancer that can't be removed with surgery or that has spread to other areas of the body. Sometimes it's used with radiation therapy.
Radiation therapy
Radiation therapy uses powerful energy beams to kill cancer cells. The energy can come from X-rays, protons or other sources.
Radiation therapy can shrink a large cancer before an operation to make it easier to remove. When surgery isn't an option, radiation therapy might be used to relieve symptoms, such as pain. Some people have radiation and chemotherapy at the same time.
Targeted therapy
Targeted therapy uses medicines that attack certain chemicals in cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die.
Targeted therapy is usually combined with chemotherapy. Targeted therapy is typically used for people with advanced colon cancer.
Immunotherapy
Immunotherapy is a treatment with medicine that helps the body's immune system kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn't be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells.
Immunotherapy is usually reserved for advanced colon cancer.
Palliative care
Palliative care is a special type of health care that focuses on relieving pain and other symptoms of a serious illness. Palliative care is done by a team of health care professionals. The team can include doctors, nurses and other specially trained professionals. Their goal is to improve the quality of life for people with serious illness and their families.
Palliative care is an extra layer of support during cancer treatment. When palliative care is used with all other appropriate treatments, people with cancer may feel better and live longer.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
It can be hard to cope with a cancer diagnosis. In time, people learn to cope in their own ways. Until you find what works for you, you might try to:
- Learn enough about your cancer to make treatment decisions. Ask your health care team about the type and stage of your cancer, as well as your treatment options and their side effects. The more you know, the more you'll be able to take part in decisions about your care. Ask your health care team to recommend other sources of information, such as websites you can trust.
- Keep friends and family close. Keeping people you care about close to you can help you deal with cancer. Friends and family can help you take care of things if you're in the hospital. And they can offer you support when you feel like you have too much to handle.
-
Find someone to talk with. Find a good listener who will listen to you talk about your hopes and fears. This may be a friend or family member. Talking to a counselor, medical social worker, clergy member or cancer support group also might be helpful.
Ask your health care team about support groups in your area or contact a cancer organization, such as the National Cancer Institute or the American Cancer Society.
Preparing for your appointment
If you have colon cancer, you'll likely be referred to specialists who treat the disease. You might meet with:
- A doctor who treats digestive diseases, called a gastroenterologist.
- A doctor who uses medicines to treat cancer, called an oncologist.
- A doctor who removes colon cancer using surgery, called a surgeon.
- A doctor who uses radiation to treat cancer, called a radiation oncologist.
Here's some information to help you get ready for your appointment.
What you can do
Ask a family member or friend to go to your appointment with you to help you remember the information you're told.
Make a list of:
- Your symptoms and when they began.
- Key medical information, including other conditions you have and your family medical history.
- All medicines, vitamins or supplements you take, including doses.
- Questions to ask your health care team.
Some basic questions to ask include:
- Where in my colon is my cancer?
- What is the stage of my colon cancer?
- Can you explain the lab report of my cancer to me?
- Can I have a copy of my lab report?
- Has my colon cancer spread? Where to?
- Will I need more tests?
- What are the treatment options for my colon cancer?
- What is the chance that my colon cancer can be cured?
- What are the potential side effects of each treatment?
- How will each treatment affect my daily life?
- How much time can I take to decide about treatment?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
What to expect from your doctor
Be prepared to answer some basic questions about your symptoms, such as:
- Have your symptoms been ongoing, or do they come and go?
- How bad are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
Dec. 19, 2024