Cancer risk: What the numbers mean
Take the time to understand what cancer risk is and how it's measured. This can help you put your own cancer risk into perspective.
By Mayo Clinic Staff
You might wonder about your chances of developing cancer. News reports can make it sound as if every day something is found to dramatically raise your risk. Sorting through all the information and figuring out what's valid can be tricky.
What is risk?
When scientists talk about risk, they're referring to a probability. Probability is the chance that something may occur, but not a guarantee that it will. For example, if you flip a coin, there is one chance in two, or a 50% chance, that the coin will land heads up.
Risk estimates for cancer and other diseases are determined by studying large groups of people. Researchers focus on the probability that any person or category of people will develop the disease over a certain period of time. They also look to see what characteristics or behaviors are related to an increased or decreased risk.
How is risk expressed?
Absolute risk
Absolute risk
Absolute risk
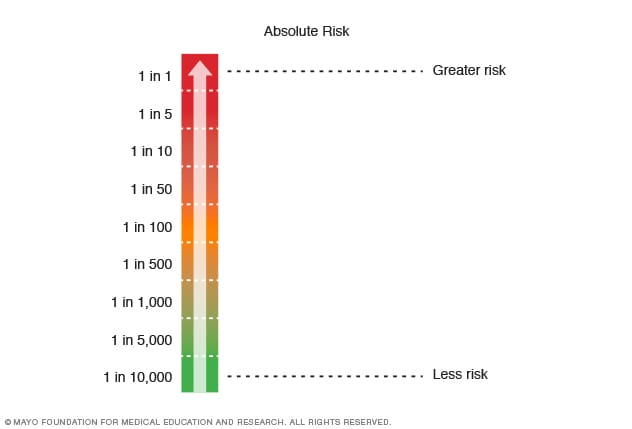
Use this chart to help you understand absolute risk. Absolute risk is often stated as risk of 1 in some number. A 1 in 5 risk is higher than a 1 in 50 risk.
Relative risk
Relative risk
Relative risk
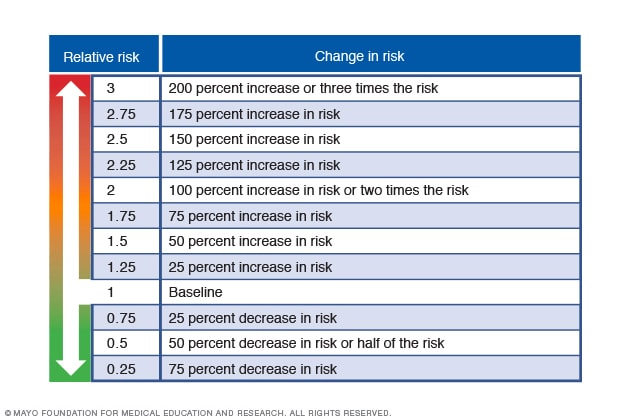
Use this scale to put relative risk in perspective. Risk seems greater when put in terms of relative risk. A 100% increase in risk may seem huge. However, if the risk began as 1 in 100 people, the risk is increased to 2 in 100. To some people, this will seem like a large increase in risk. To others, it won't. You and your healthcare professional have to decide what levels of risk are acceptable to you.
Risk is generally divided into two categories: absolute risk and relative risk.
Absolute risk
Absolute risk refers to the actual numeric chance or probability of developing cancer during a certain time period. The time period could be within the year, within the next five years, by age 50, by age 70, or during the course of a lifetime.
One type of absolute risk is lifetime risk. Lifetime risk is the probability that an individual will develop cancer during the course of a lifetime. For instance, an American man's absolute risk of developing prostate cancer in his lifetime is about 13%. Put another way, about 13 out of every 100 men will develop prostate cancer at some time in their lives. This also means that 87 out of every 100 men won't develop prostate cancer.
Lifetime risk isn't the risk that a person will develop cancer in the next year or the next five years. An individual's cancer risk has a lot to do with other factors, such as age. For instance, an American woman's lifetime risk of developing colon and rectal cancer is about 4%, or about 40 out of every 1,000 women. But her risk of developing colon and rectal cancer before the age of 50 is 0.4%, or about 4 out of every 1,000 women.
Relative risk
Relative risk gives you a comparison or ratio rather than an absolute value. It shows the strength of the relationship between a risk factor and a certain type of cancer. It does this by comparing the number of cancers in a group of people who have a certain trait with the number of cancers in a group of people who don't have that trait.
For instance, compare the lung cancer risk for people who smoke with the lung cancer risk in a similar group of people who don't smoke. You might hear relative risk being expressed like this: The risk of lung cancer for people who smoke is 25 times higher than the risk for people who don't smoke. So the relative risk of lung cancer for people who smoke is 25.
Relative risk also can be given as a percentage. For example, the risk of lung cancer for people who smoke is 2,500% higher than it is for people who don't smoke.
When you hear about relative risk, there's no upper limit to the percentage increase in risk. Most people think 100% is the highest possible risk, but that isn't true with relative risk.
A relative risk of 100% means your risk is twice as high as that of someone without that risk factor. A 200% relative risk means that you are three times as likely to develop that condition.
Risk seems greater when put in these terms. A 100% increase in risk may seem huge. However, if the risk began as 1 in 100 people, a 100% increase in risk means that 2 out of 100 will be affected.
Where do cancer risk statistics come from?
Most information about cancer risk and risk factors comes from studies that focus on large, well-defined groups of people. Cancer researchers have identified many of the major environmental factors that contribute to cancer. These include smoking for lung cancer and sunlight for skin cancer. Uncovering more subtle cancer risks is more difficult.
Many studies of cancer risk factors rely on observational approaches. In these studies, researchers keep track of a group of people for several years without trying to change their lives or provide special treatment. This can help scientists find out who develops a disease, what those people have in common and how they differ from those who didn't get sick.
How do cancer risk statistics relate to you?
Risk statistics can be frustrating because they can't tell you your risk of cancer. Studies may have found that American men have about a 40% chance of developing cancer in their lifetimes. However, that doesn't mean your risk is 40% if you're a man. Your individual risk is based on many different factors. These factors may include age and habits, family history of cancer, and the environment in which you live.
Even then, the combination of risk factors might not apply to you. Cancer depends on the individual. You can have two people with the same age, sex, race, socio-economic status and similar lifestyles and still have different experiences. Risk statistics are helpful in general statements such as "exercising regularly can reduce the risk of chronic diseases, such as cancer." But exercising regularly won't guarantee that you won't get cancer.
Talk with your healthcare professional about your risk of cancer. Your health professional can review what elements in your life may increase your risk. You can then discuss what to do to help lower this risk.
Keep cancer risk statistics in perspective
You might hear a news report about a study that seems to indicate you may be at increased risk of a certain type of cancer. Don't jump to conclusions based on this one report. Take a step back and think about what the risk really means.
Observational studies aren't foolproof. Researchers agree that one study by itself isn't reliable. This is why you sometimes see studies with different results.
Scientists weigh the evidence of many research studies over time to better determine whether a finding is true. News reports, though, focus on each new study in isolation, rather than as a part of an evolving picture. This can sometimes cause unnecessary alarm or confusion.
When you read or see a report about cancer risk statistics, pay attention to these details:
- Who's being observed? A news report may say a certain activity increases the risk of cancer for a group of people. But who was being observed in the study? Pay attention to the ages of the people and their characteristics. For instance, some people are more likely to develop certain types of cancer because of their genetics.
- How many people were studied? In general, studies involving thousands of people are more accurate than are those that examine a small group of people.
- Have similar studies been done? The findings of one study are more reliable if they're similar to findings by other studies. Sometimes, the study wasn't carried out for enough years to make it statistically significant.
News reports that focus on alarming statistics, such as a 300% increase in risk, but don't give you context aren't helpful. If you're concerned about the risk, gather more information and talk to your healthcare professional.
March 29, 2024
- Understanding cancer risk. Cancer.Net. https://www.cancer.net/navigating-cancer-care/prevention-and-healthy-living/understanding-cancer-risk. Accessed Oct. 13, 2023.
- Cancer facts & figures 2023. American Cancer Society. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html. Accessed Oct. 13, 2023.
- Cancer stat facts: Cancer of any site. National Cancer Institute. https://seer.cancer.gov/statfacts/html/all.html. Accessed Oct. 13, 2023.