Overview
Female reproductive system
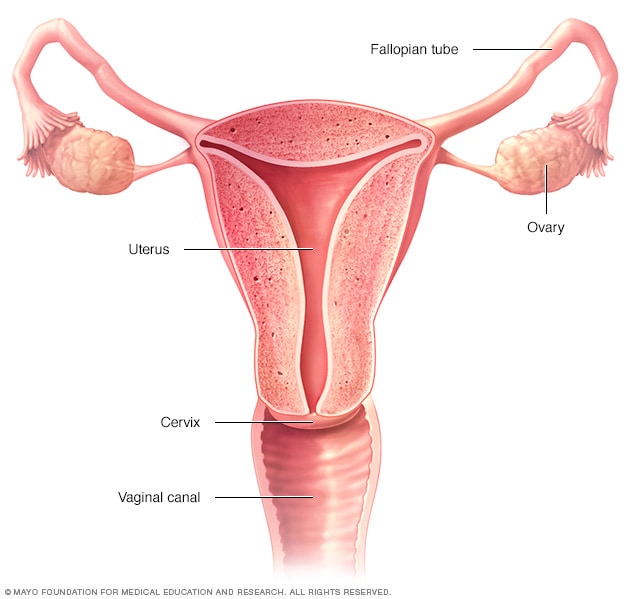
Female reproductive system
The ovaries, fallopian tubes, uterus, cervix and vagina, also called the vaginal canal, make up the female reproductive system.
A hysterectomy is surgery to remove the uterus. When a surgeon uses a robotic machine to do a hysterectomy, it's called a robotic hysterectomy. You also might hear it called a robot-assisted hysterectomy.
During robotic surgery, the surgeon sits at a computer console in the operating room and controls a robotic arm with surgical tools attached to it. The surgeon uses the arm to operate through small cuts called incisions. A small, lighted tool with a camera provides a highly detailed, magnified 3D view. Robotic hysterectomy helps the surgeon make precise, flexible movements with the surgical tools.
Because a robotic hysterectomy is done through small cuts, it can have advantages. You're likely to have less pain and lose less blood than is typical with a large incision in the stomach area. Surgery that involves a large cut is known as an open abdominal hysterectomy. Robotic surgery may help you get back to your daily routine more quickly than you would with open surgery.
Products & Services
Why it's done
With a hysterectomy, part or all of the uterus is removed. Sometimes, nearby parts of the reproductive system need to be removed as well: the fallopian tubes or one or both ovaries.
Healthcare professionals do hysterectomies to treat conditions such as:
- Uterine fibroids. These common growths of the uterus aren't cancer.
- Endometriosis. This is a condition in which tissue that is similar to the inner lining of the uterus grows outside the uterus.
- Cancer or irregular cells that may become cancer. These can affect the upper part of the uterus, the ovaries or the lower end of the uterus called the cervix.
- Uterine prolapse. This is when the uterus sags into the vagina or bulges out of the vagina.
- Irregular, heavy or very long periods.
- Ongoing pelvic pain, also called chronic pelvic pain.
Surgeons have various ways to do hysterectomies without the large incision of open surgery. A robotic hysterectomy is done through small cuts in the lower belly. A laparoscopic hysterectomy also is done this way, but the surgeon doesn't use robotic equipment.
A vaginal hysterectomy is performed through a small cut in the vagina. The surgeon doesn't need to use robotic or laparoscopic equipment, but using those tools may be an option. If the surgeon uses robotic or laparoscopic tools, there will also be a series of small cuts made to the lower belly.
Vaginal surgery is linked with better outcomes and fewer complications compared with open, robotic and laparoscopic hysterectomies. But vaginal surgery may not be an option for everyone.
Your healthcare professional might recommend a robotic or laparoscopic hysterectomy if a vaginal hysterectomy isn't right for you. This might be true if you have scars from a past surgery or a very large uterus. Your options depend on your medical history and the condition for which you're getting a hysterectomy. Robotic or laparoscopic surgery also lets the surgeon check other areas of the abdomen and pelvis if needed. The surgeon can take tissue samples or remove lymph nodes during a hysterectomy done to treat endometrial cancer, also called uterine cancer.
Risks
Although robotic hysterectomy is mostly safe, any surgery has risks. Risks of a robotic hysterectomy include:
- Heavy bleeding.
- Blood clots in the legs or lungs.
- Infection.
- Damage to the bladder and other nearby organs.
- Side effects from medicines called anesthetics that prevent pain and put you in a sleeplike state during surgery.
How you prepare
As with having any surgery, you may feel nervous about having a hysterectomy. Here's what you can do to prepare:
- Gather information. Before the surgery, get all the information you need to feel confident about it. Ask questions of your surgeon and healthcare team.
- Follow your healthcare team's instructions about medicine. Find out whether you should take your usual medicines in the days before your hysterectomy. Be sure to tell your healthcare team about all medicines, supplements or herbs that you take.
- Arrange for help. You're likely to recover sooner after a robotic hysterectomy than after an abdominal one, but recovery still takes time. Ask someone to help you out at home for the first week or so.
What you can expect
Talk with a member of your healthcare team about what to expect during and after a robotic hysterectomy. Ask about the ways it might affect your body and emotions.
During the procedure
Robotic hysterectomy incisions
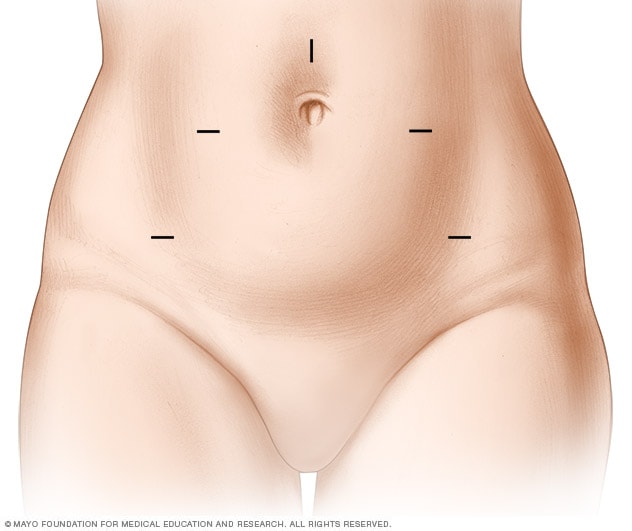
Robotic hysterectomy incisions
During a robotic hysterectomy, the surgeon makes five small cuts called incisions in the lower belly. This provides access for surgical tools. Through these cuts, the surgeon detaches the uterus. Sometimes, the cervix, one or both ovaries, or the fallopian tubes also may need to be removed. The surgeon may remove the organs through one of the small cuts in the lower belly or, more often, through the vagina.
You lie on your back, like you do for a Pap test. You might have a tube, called a urinary catheter, put into your urethra to empty your bladder. A member of your surgical team cleans the surgical area with a sterile solution before surgery.
You're given medicines, called anesthetics, that make you comfortable during surgery. You'll have five small cuts, called incisions, made in your lower belly. Slender surgical tools are placed through these cuts.
During the surgery:
- Your surgeon sits at a nearby robotic computer console and controls the surgical tools that remove your uterus.
- Your surgeon also might remove your cervix, one or both ovaries, or your fallopian tubes. It depends on the health condition for which the hysterectomy is being done.
- An assistant at the operating table places the robotic instruments in various positions as needed. The assistant also adds or removes surgical devices and provides other support to your surgeon.
- Members of the anesthesia team track your condition and comfort the whole time.
After the procedure
People recover at different rates. But most often, people who have a robotic hysterectomy are able to leave the hospital the same day as surgery. Some people need to stay in the hospital overnight.
You may take medicine for pain. And your healthcare team likely will encourage you to get up and move as soon as you're able. You also may be given medicine to prevent blood clots.
You can expect some bloody discharge from the vagina for a few weeks after your robotic hysterectomy.
How your body might feel
Recovery after robotic hysterectomy is shorter and less painful than that after an abdominal hysterectomy. A full recovery might take 3 to 4 weeks.
Even if you feel better, don't lift anything heavy for 6 weeks after surgery. In general, that means any object over 15 pounds (6.8 kilograms). Don't have vaginal sex until six weeks after surgery. Also, don't place anything in your vagina during this time, including tampons. You can use sanitary pads while you recover.
Call your healthcare professional right away if you have any of the following symptoms:
- Pain that becomes worse.
- Fever.
- Upset stomach or vomiting.
- Bleeding that's heavier than a menstrual period.
What emotions might come up
After a hysterectomy, you might feel relief because you no longer have heavy bleeding or pelvic pain.
For many people, there's no change in how they respond to sex after hysterectomy. Some who have their ovaries removed may have vaginal dryness and less interest in sex. But some have better sex after hysterectomy. That may be because they no longer have pain during sex.
Not being able to become pregnant might bring on a sense of loss and grief. Or you might become depressed, especially if you're young and hoped for a future pregnancy. If grief, stress or sadness affect your everyday life, talk with your healthcare professional. Treatment can help.
Results
After a hysterectomy, you no longer have periods. You can't get pregnant.
If you have your ovaries removed before you reach menopause, you'll go into menopause right after surgery. You might have symptoms such as vaginal dryness, hot flashes and night sweats. There are medicines to help manage these symptoms. Your healthcare professional might suggest hormone therapy for menopause even if you don't have symptoms.
If your ovaries weren't removed during surgery and you still had periods before your surgery, your ovaries keep making hormones and releasing eggs. This process happens until you reach natural menopause.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Jan. 17, 2025