Overview
Brain stereotactic radiosurgery (SRS) is a radiation treatment for specific brain conditions. It works by delivering highly focused beams of energy to defined areas in the brain. It's not surgery in the traditional sense — it involves no cuts or openings in the skull. But the radiation is delivered with virtually the same precision as a surgical tool.
Doctors use detailed pictures of the brain along with special computer software to map the treatment area and guide the radiation. Each beam alone delivers a small dose of radiation. But where the beams meet, they deliver a concentrated dose that destroys the target cells while sparing surrounding tissues. This precision lessens side effects. And it allows many people to go back to their usual activities shortly after treatment.
Radiation works by damaging the DNA of the targeted cells. DNA is like a cell's instruction manual. When the DNA is damaged, the cells can't function or multiply, and they eventually die. These effects may take some time, but the treatment can be very effective.
Brain SRS can treat:
- Brain tumors.
- Tangles of blood vessels called arteriovenous malformations (AVMs).
- Nerve conditions such as trigeminal neuralgia.
- Other brain conditions.
Types of brain stereotactic radiosurgery
Gamma Knife radiosurgery
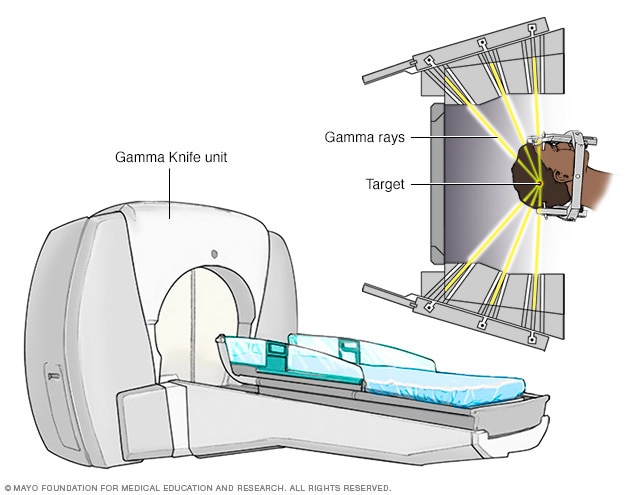
Gamma Knife radiosurgery
Gamma Knife surgery uses many small gamma rays to deliver a precise dose of radiation to the target.
LINAC system
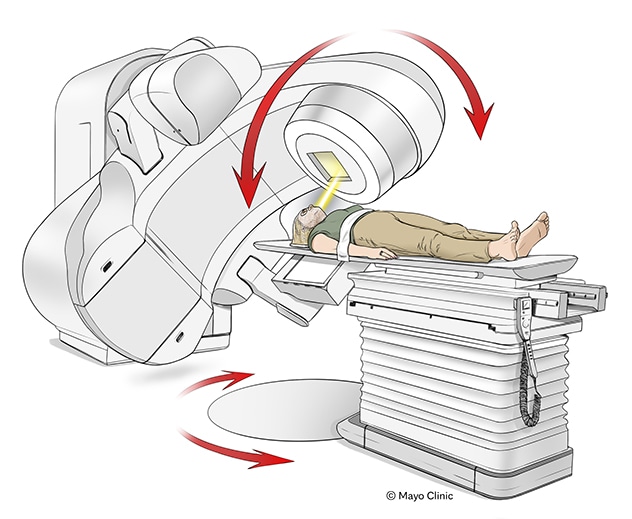
LINAC system
Linear accelerator (LINAC) systems typically rotate around the person receiving radiation.
Several types of technology are used to deliver radiation during brain SRS. The main difference between them is that their energy comes from different sources.
- Gamma Knife surgery uses tiny particles of energy called photons. With Gamma Knife surgery, the photons come from gamma rays. The machine points around 200 beams of gamma rays at the treatment area. Gamma Knife is often used to treat small- to medium-sized tumors, AVMs and trigeminal neuralgia.
- Linear accelerator (LINAC) systems also use photons, but from X-rays. Brand names include Varian Edge, CyberKnife and others. LINAC systems can treat larger tumors, and these systems can be used in other parts of the body. Some systems use robotic arms and motion tracking to ensure the radiation stays on target.
- Proton beam therapy uses protons to treat brain cancers. Protons are parts of atoms with a positive charge. Proton beams are unique because they deposit most of their energy directly at the tumor site, sparing healthy tissues nearby. This makes proton therapy especially useful for tumors near sensitive areas like the brainstem or optic nerves. And it's useful for longer courses of radiation.
Why it's done
Brain SRS may be used to treat the following conditions:
- Brain tumor. SRS can manage small tumors in the brain. Small tumors that are not cancer are called benign. Those that are cancer are called malignant. The intense radiation damages tumor cells so they can't grow and divide. Eventually the cells die, causing the tumor to shrink.
- Brain arteriovenous malformation (AVM). An AVM is a tangle of blood vessels that creates irregular connections between arteries and veins in the brain. Untreated, it can cause a stroke or bleeding in the brain. SRS causes the blood vessels to close off over time, lowering the risk of bleeding.
- Trigeminal neuralgia. Trigeminal neuralgia is a chronic pain condition that causes sudden, severe facial pain, often triggered by touch or movement. It affects the trigeminal nerve, which carries sensation from the face to the brain. If medicines for trigeminal neuralgia aren't effective or cause too many side effects, SRS can target the nerve root and reduce pain signals.
- Acoustic neuroma. An acoustic neuroma is a benign tumor that forms on the nerve responsible for hearing and balance. It can cause hearing loss, dizziness, balance problems or ringing in the ears. SRS may stop the growth of the tumor and help preserve hearing and nerve function.
- Pituitary tumors. These tumors form in the pituitary gland, which controls many body hormones. SRS can shrink the tumor and stabilize hormone production.
Brain SRS may be chosen over traditional brain surgery because it avoids risks of open surgery, such as bleeding, infection and nerve damage.
Brain SRS may be recommended when:
- The area to be treated is small, clearly defined and not too close to vital brain areas.
- The targeted area is hard to reach with traditional brain surgery.
- A person isn't healthy enough for traditional brain surgery.
- A person prefers a less invasive option.
Risks
Brain SRS is generally safe and effective. Like any medical procedure, it carries risks of side effects. Some arise soon after treatment; others may be delayed.
Early side effects may include:
- Fatigue. Fatigue is common after radiation and may peak within 1 to 2 weeks after treatment. It typically resolves over several months.
- Headache and upset stomach. Some people experience mild headaches or an upset stomach shortly after treatment. These symptoms are usually temporary and manageable with medicine.
- Swelling. Swelling in the brain after treatment can mimic tumor growth and worsen preexisting symptoms. Medicines such as steroids are often prescribed to manage this.
- Pin-site discomfort. If a head frame is used for your procedure, you may experience minor bleeding, bruising or tenderness at the pin sites.
- Seizures. Rarely, seizures may occur due to temporary brain swelling or irritation. Antiseizure medicine may be used as a precaution.
Delayed side effects are rare. They may include:
- Radiation necrosis. Dead tissue that builds up in the treated area can cause swelling and put pressure on brain tissue. Treatment may include steroids, oxygen therapy or surgery.
- Nerve damage. Radiation near sensitive cranial nerves, such as nerves that link the eyes or ears to the brain, can cause vision or hearing changes. This risk is lessened with careful dose planning.
How you prepare
Food and medicines
- Don't eat or drink anything after midnight the night before the procedure.
- Talk with a member of your healthcare team about whether you can take your regular medicines the night before or morning of the procedure.
- If you'll need multiple sessions, ask your healthcare team for specific instructions about food and medicine.
Clothing and personal items
Wear comfortable, loose clothing.
Avoid wearing the following items during the procedure:
- Jewelry.
- Eyeglasses.
- Contact lenses.
- Makeup.
- Nail polish.
- Dentures.
- Wigs or hairpieces.
Other precautions
Tell a member of your healthcare team if you:
- Are taking pills or injections to manage diabetes.
- Are allergic to intravenous contrast medium or iodine.
- Have implanted medical devices in your body, such as a pacemaker, artificial heart valve, aneurysm clips, neurostimulators or stents.
- Experience claustrophobia.
What you can expect
Before the procedure
Careful planning is required to deliver radiation to exactly the place in your brain that needs treatment. Two things need to happen: Your head needs to stay still while the treatment area is mapped out. And your head needs to be in the exact same position relative to radiation beams on the day of treatment. To get ready, you go through a planning session called simulation.
To help keep your head firmly in place, your healthcare team may use a fixed head frame or a custom mask. This frame or mask also serves as a point of reference for focusing the beams of radiation.
- Fixed head frame. A lightweight metal frame is fitted to your head with four pins. You receive numbing shots where the pins will be inserted — two points on the forehead and two at the back of the head.
- Custom mask. A custom mask is made of lightweight thermoplastic material. Your team warms the mask and places it over your face. As the mask cools on your face, it hardens and keeps the shape of your face. The mask is less rigid than the frame system and makes it easier to conduct multiple treatment sessions. This may be helpful for treating larger brain tumors.
You use the same frame or mask every time you have a treatment.
Your SRS team conducts imaging tests to pinpoint the location of the treatment area in relation to the frame or mask.
- CT and MRI scans are often used to visualize brain tumors.
- A cerebral angiogram lets your team see detailed images of the blood vessels in your brain. It may be used along with an MRI before treatment for an arteriovenous malformation (AVM).
- An MRI scan can create images of nerve fibers in your head and neck. Your team uses these images to select a target area for treating trigeminal neuralgia.
The images are entered into a computer to plan exactly how much radiation to deliver and from what angles. This planning process usually takes less than an hour.
During that time, you can relax in another room. The frame, if it is used, must remain attached to your head. If a mask is used instead of a frame, some of the planning takes place before the mask is placed.
Children often get medicines to put them in a sleeplike state for the simulation and the procedure. Adults are usually awake but may be given a medicine to help them relax.
During the procedure
If a head frame is used, the frame is attached to your head. The head frame attaches securely to a docking device on the table you lie on.
If a custom mask is used, you may lie on a specialized neck support and a healthcare professional puts the mask on your face.
The machine may rotate around you, move on robotic arms or slide you into a treatment unit depending on the system used.
You get fluids directly into your bloodstream through an intravenous (IV) line. The fluids keep you hydrated during the procedure.
It can take up to four hours to complete the procedure. The time depends on the size and shape of the target. During the procedure:
- You won't feel or see the radiation.
- You may hear some noise as the machine moves into place.
- Usually you are able to talk with your healthcare team via a microphone.
Brain SRS usually is an outpatient procedure, which means you probably won't have to stay overnight in the hospital. But the entire process may take most of the day. You may be asked to bring a family member or friend who can be with you during the day and who can take you home. Rarely, you may stay overnight in the hospital.
After the procedure
After the procedure:
- The head frame or mask is removed.
- You may have minor bleeding or tenderness at the pin sites if a head frame was used.
- You may receive medicines to help prevent or ease symptoms that can happen after treatment. Symptoms may include headache, upset stomach or vomiting.
An advantage of brain SRS over some other types of treatment, such as traditional brain surgery, is that recovery is short and major side effects are not common. Most people can go back to their usual activities within a day or two after the procedure.
Small tumors are often treated in a single session. Larger tumors or those near important brain areas may require 3 to 5 sessions. Recovery time varies depending on the condition treated and individual response.
Results
Gamma Knife surgery results

Gamma Knife surgery results
Gamma Knife surgery uses multiple tiny beams of radiation to shrink tumors. The left brain scan shows a pretreatment image of a noncancerous tumor — an image enhanced by the use of a special medium, called a contrast agent. At six months after treatment (middle image), the tumor appears slightly larger but doesn't take up as much of the contrast medium — it isn't as bright in the center. This indicates a positive treatment effect. At seven years (right scan), the tumor appears much smaller.
Brain AVM before and after Gamma Knife treatment

Brain AVM before and after Gamma Knife treatment
Brain arteriovenous malformation before Gamma Knife treatment (left) and 52 months after the procedure (right)
Brain tumor before and after Gamma Knife treatment
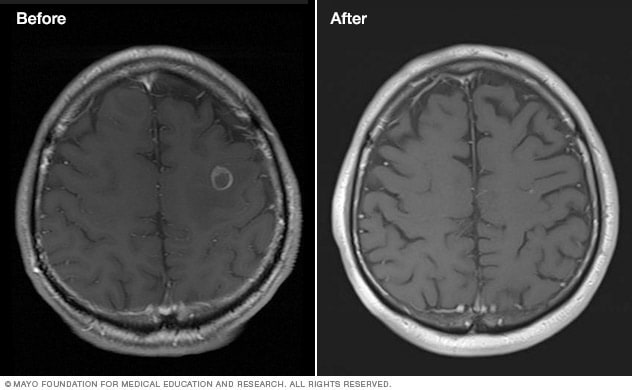
Brain tumor before and after Gamma Knife treatment
Malignant brain tumor before (left) and 111 months after Gamma Knife stereotactic radiosurgery (right)
The effects of brain SRS happen gradually depending on the condition being treated:
- Benign tumors may shrink over a period of months to years.
- Malignant tumors may shrink quickly, often within a few months.
- Brain AVM blood vessels thicken and close off in 1 to 3 years.
- Trigeminal neuralgia pain relief may take several months.
Your healthcare team may schedule follow-up exams to monitor your progress.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Sept. 26, 2025