Overview
Supraventricular tachycardia (SVT) is a type of irregular heartbeat, also called an arrhythmia. It's a very fast or erratic heartbeat that affects the heart's upper chambers. SVT also is called paroxysmal supraventricular tachycardia.
The typical heart beats about 60 to 100 times a minute. During SVT, the heart beats about 150 to 220 times a minute. Occasionally it beats faster or slower.
Most people with supraventricular tachycardia don't need treatment. When recommended, treatment may include specific actions or movements, medicines, a heart procedure, or a device to control the heartbeat.
Types
Supraventricular tachycardia (SVT) falls into three main groups:
- Atrioventricular nodal reentrant tachycardia (AVNRT). This is the most common type of supraventricular tachycardia.
- Atrioventricular reciprocating tachycardia (AVRT). This is the second most common type of supraventricular tachycardia. It's most commonly seen in younger people.
- Atrial tachycardia. This type of SVT is more commonly seen in people who have heart disease. Atrial tachycardia doesn't involve the AV node.
Other types of supraventricular tachycardia include:
- Sinus nodal reentrant tachycardia (SNRT).
- Inappropriate sinus tachycardia (IST).
- Multifocal atrial tachycardia (MAT).
- Junctional ectopic tachycardia (JET).
- Nonparoxysmal junctional tachycardia (NPJT).
Symptoms
The main symptom of supraventricular tachycardia (SVT) is a very fast heartbeat that may last for a few minutes to a few days. The heart beats 100 or more times a minute. Usually during SVT, the heart beats 150 to 220 times a minute. The fast heartbeat may come and go suddenly.
Symptoms of supraventricular tachycardia may include:
- Pounding or fluttering feelings in the chest, called palpitations.
- A pounding sensation in the neck.
- Chest pain.
- Fainting or almost fainting.
- Lightheadedness or dizziness.
- Shortness of breath.
- Sweating.
- Weakness or extreme tiredness.
Some people with SVT do not notice symptoms.
In infants and very young children, symptoms of SVT may be vague. The symptoms can include sweating, poor feeding, a change in skin color and a rapid pulse. If your infant or young child has any of these symptoms, talk with a healthcare professional.
When to see a doctor
Supraventricular tachycardia (SVT) is usually not life-threatening unless you have heart damage or another heart condition. But if SVT is severe, the irregular heartbeat may cause all heart activity to suddenly stop. This is called sudden cardiac arrest.
Call a healthcare professional if you have a very fast heartbeat for the first time or if an irregular heartbeat lasts longer than a few seconds.
Symptoms of SVT may be related to a serious health condition. Call 911 or your local emergency number if you have a very fast heartbeat that lasts for more than a few minutes or if a fast heartbeat occurs with these symptoms:
- Chest pain.
- Dizziness.
- Shortness of breath.
- Weakness.
Causes
Supraventricular tachycardia (SVT) is caused by faulty signaling in the heart. Electrical signals in the heart control the heartbeat.
In SVT, a change in heart signaling causes the heartbeat to start too early in the heart's upper chambers. When this happens, the heartbeat speeds up. The heart can't fill with blood properly. Symptoms such as lightheadedness or dizziness can occur.
How does the heart beat?
Typical heartbeat
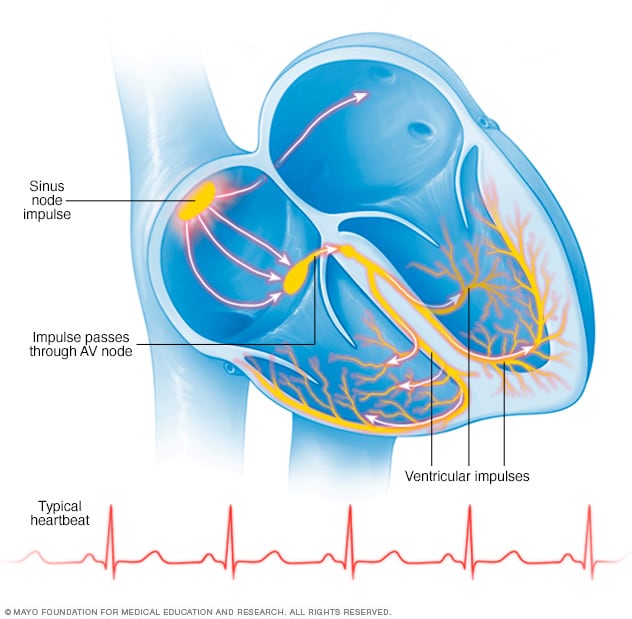
Typical heartbeat
In a typical heart rhythm, a tiny cluster of cells at the sinus node sends out an electrical signal. The signal then travels through the atria to the atrioventricular (AV) node and then passes into the ventricles, causing them to contract and pump out blood.
Supraventricular tachycardia
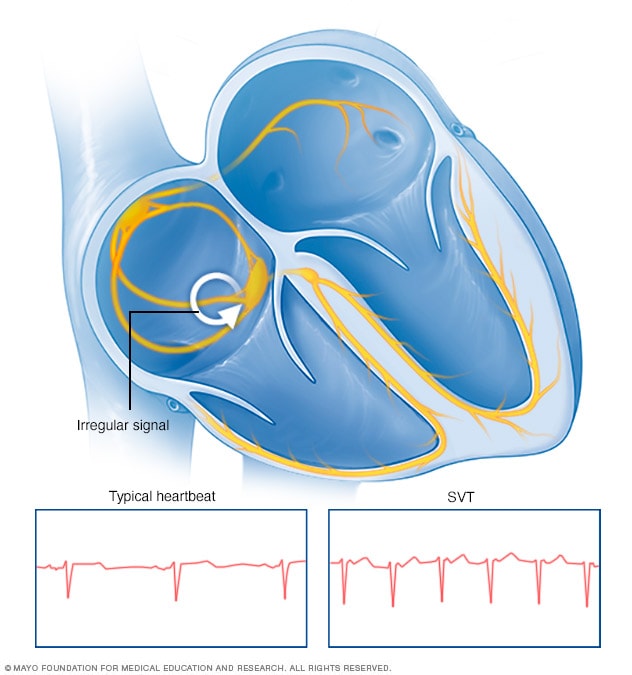
Supraventricular tachycardia
Supraventricular tachycardia (SVT) is an irregularly fast or erratic heartbeat. It occurs when faulty electrical signaling in the heart set off a series of early beats in the upper chambers of the heart.
To understand the cause of supraventricular tachycardia (SVT), it might help to know how the heart usually works.
The heart has four chambers:
- The two upper chambers are called the atria.
- The two lower chambers are called the ventricles.
Inside the upper right heart chamber is a group of cells called the sinus node. The sinus node makes the signals that start each heartbeat.
The signals move across the upper heart chambers. Then the signals arrive at a group of cells called the AV node, where they usually slow down. The signals then go to the lower heart chambers.
In a healthy heart, this heart signaling process usually goes smoothly. The heart usually beats about 60 to 100 times a minute at rest. But in SVT, the heart beats faster than 100 beats a minute. The heart may beat 150 to 220 times a minute.
Risk factors
Supraventricular tachycardia (SVT) is the most common type of arrhythmia in infants and children. It also tends to occur more often in women, particularly during pregnancy.
Health conditions or treatments that may increase the risk of supraventricular tachycardia include:
- Coronary artery disease, heart valve disease and other heart diseases.
- Heart failure.
- A heart problem present at birth, also called a congenital heart defect.
- Previous heart surgery.
- A sleep disorder called obstructive sleep apnea.
- Thyroid disease.
- Uncontrolled diabetes.
- Some medicines, including those used to treat asthma, allergies and colds.
Other things that may increase the risk of SVT include:
- Emotional stress.
- Too much caffeine.
- Excessive alcohol use, which is defined as 14 or more drinks a week for men and seven or more drinks a week for women.
- Smoking and nicotine use.
- Stimulant drugs, including cocaine and methamphetamine.
Complications
When the heart beats too fast, it may not send enough blood to the body. As a result, the organs and tissues may not get enough oxygen.
Over time, untreated and frequent attacks of supraventricular tachycardia (SVT) may weaken the heart and lead to heart failure. This is especially true in people who also have other medical conditions.
A severe attack of SVT may cause fainting or a sudden loss of all heart activity, called sudden cardiac arrest.
Prevention
The same lifestyle changes used to manage supraventricular tachycardia (SVT) also may help prevent it. Try these tips.
- Follow a heart-healthy lifestyle. Eat a nutritious diet, don't smoke, get regular exercise and manage stress.
- Don't use a lot of caffeine. Avoid large amounts of caffeine. For most people with supraventricular tachycardia, moderate amounts of caffeine do not trigger episodes of SVT.
- Keep a notebook or diary of when symptoms happen. Include the symptoms, your heart rate and what you were doing at the time of the fast heartbeat. This information can help you learn the things that trigger the very fast heartbeat.
- Use medicines carefully. Some medicines, including those bought without a prescription, may contain stimulants that can trigger SVT.