Diagnosis
SCAD is usually diagnosed in an emergency setting. You may be asked questions about your personal and family medical history. Tests are done to check your heart.
Tests
Cardiac catheterization procedure approaches
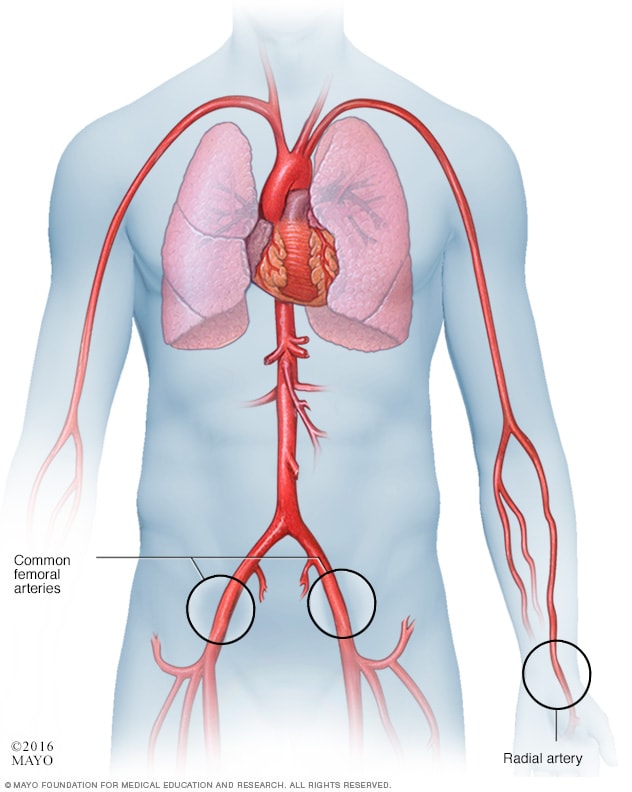
Cardiac catheterization procedure approaches
In a cardiac catheter procedure, a doctor inserts a flexible tube called a catheter into a blood vessel. Sometimes it's placed in the wrist artery, called the radial artery. Or it may be placed in an artery in the groin, called the femoral artery. The catheter is then guided to the heart.
Coronary angiogram
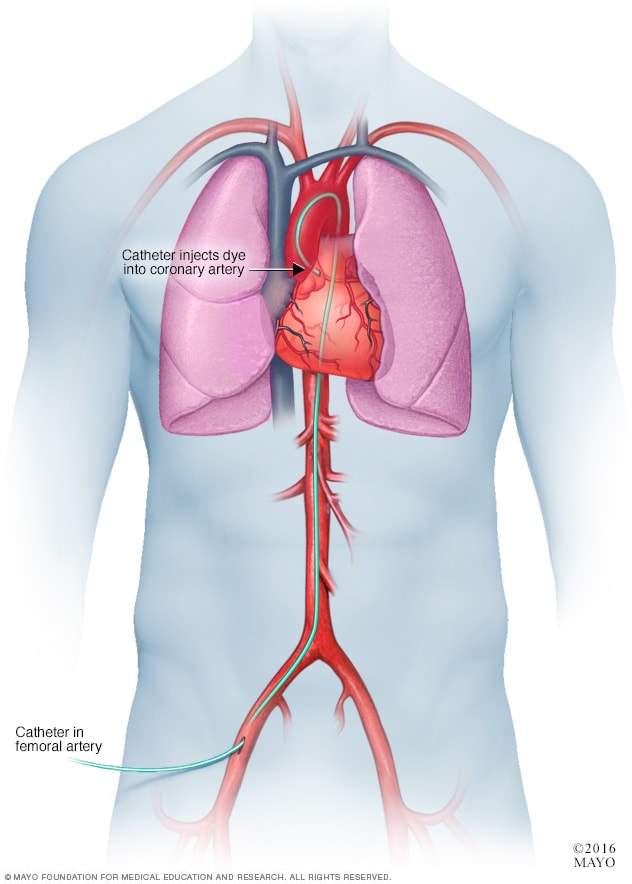
Coronary angiogram
In a coronary angiogram, a flexible tube called a catheter is inserted into an artery, usually in the groin, arm or neck. It's guided to the heart. A coronary angiogram can show blocked or narrowed blood vessels in the heart.
Heart with tortuous coronary arteries
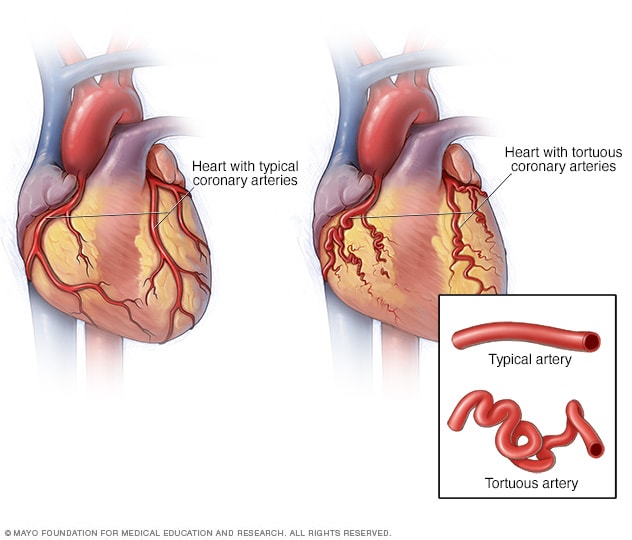
Heart with tortuous coronary arteries
In some health conditions, the arteries in the heart may be twisted. The heart arteries are called the coronary arteries. Twisted arteries also are called tortuous arteries.
Tests to diagnose SCAD are similar to tests used to detect a heart attack. They may include:
- Blood tests. Certain heart proteins slowly leak into the blood after heart damage from a heart attack. Blood tests can check for these proteins. Other blood tests also may be done.
- Electrocardiogram (ECG or EKG). This quick test checks the heart's electrical activity. It can show how fast or how slowly the heart is beating. Sticky patches called electrodes are attached to the chest and sometimes the arms and legs. An electrocardiogram (ECG) can tell if you are having or have had a heart attack.
- Coronary angiogram. This test looks inside the heart arteries. A doctor places a long, thin flexible tube called a catheter into a blood vessel, usually in the groin or wrist. It's guided to the heart. Dye flows through the tube to the arteries. The dye helps the arteries show up more clearly on images and video. A coronary angiogram can diagnose SCAD. It also can show any twisted arteries.
Other tests may be done during a coronary angiogram to confirm SCAD and plan treatment. These tests include:
- Optical coherence tomography (OCT). This test uses light to see inside the blood vessels and blood vessel walls. The doctor inserts a flexible tube called a catheter into a blood vessel and guides it to the heart. A beam of light shines from the catheter. The test can help accurately diagnose the cause of a heart attack.
- Intravascular ultrasound (IVUS). Sound waves are used to take pictures of the inside of the heart arteries. The doctor inserts a flexible tube called a catheter into a blood vessel and guides it to the heart. A device on the end of the tube gives off sound waves. A computer looks at the sound waves that bounce back and turns them into pictures of the heart arteries.
More Information
Treatment
The goals of SCAD treatment are to:
- Restore blood flow to the heart.
- Manage chest pain.
- Prevent SCAD from happening again.
Treatment may include medicines and a procedure or surgery to open the artery and restore blood flow. Sometimes SCAD heals on its own.
The type of treatment for SCAD depends on your overall health and the size and location of the tear in the artery.
Medications
Some people with SCAD only need medicines to treat symptoms. If chest pain or other symptoms continue, other treatments also might be needed.
Medicines to treat SCAD may include:
- Aspirin. Taking aspirin long-term may help to lower the risk of heart disease after SCAD. Talk to a health care professional to decide if daily aspirin therapy is right for you.
- Blood pressure medicines. Several medicines are available to lower blood pressure. You might need to take these medicines for life to reduce the risk of another SCAD.
- Medicines to control chest pain. Medicines called nitrates and calcium channel blockers can help treat chest pain after SCAD.
Surgery or other procedures
Some people with SCAD need a surgery or procedure to fix the artery and improve blood flow to the heart. These treatments may include:
-
Coronary angioplasty (AN-jee-o-plas-tee) and stent. This treatment may be needed if SCAD blocks blood flow to the heart or medicines don't control chest pain.
During the procedure, a doctor places a long, thin flexible tube called a catheter in a blood vessel, usually in the groin or wrist. It's guided to the heart. A small balloon on the tip of the catheter widens to open the artery. Then, the doctor places a tiny mesh tube called a stent inside the artery. The stent holds the artery open and improves blood flow. The balloon is removed. The stent stays in place.
Another name for this treatment is percutaneous coronary intervention or PCI.
- Coronary artery bypass surgery. This open-heart surgery creates a new path for blood to flow around a blocked or partially blocked artery. It may be done if other SCAD treatments don't work or if you have more than one tear. The surgeon takes a healthy blood vessel from the chest or leg area. This healthy vessel is called a graft. One end of the graft is stitched to the artery below the blockage. The other end is stitched to the heart. Other names for this surgery are heart bypass surgery, coronary artery bypass grafting or CABG — pronounced "cabbage."
Pregnancy
If you've had SCAD, talk to a health care professional before becoming pregnant. Pregnancy may not be safe after having SCAD.
Cardiac rehabilitation
After treatment for SCAD, you need regular checkups with your health care team.
A personalized program of exercise and education may be suggested. This is called cardiac rehabilitation, also known as cardiac rehab. It's created to help you recover from a serious heart condition. The program often includes supervised exercise, emotional support and education about a heart-healthy diet.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
It's important to take steps to keep the heart healthy. Try these tips:
- Don't smoke. Smoking is a major risk factor for heart disease. Not smoking is the best way to reduce the risk of heart disease and its complications. Also stay away from secondhand smoke. If you need help quitting, ask your care team for strategies that can help.
- Eat healthy foods. Choose whole grains, fruits, vegetables, and lean proteins, such as fish and beans. Avoid or limit foods with a lot of saturated fat, trans fats, salt and sugar.
- Exercise. Regular exercise helps control diabetes, high cholesterol and high blood pressure — all risk factors for heart disease. With your provider's OK, aim for 30 to 60 minutes of physical activity most days of the week. Talk to your health care provider about the amount and type of exercise that's best for you. You may be told to avoid intense lifting, competition and extreme temperatures.
- Maintain a healthy weight. Too much weight strains the heart. Being overweight increases the risk of high cholesterol, high blood pressure and diabetes.
- Limit alcohol. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for females and up to two drinks a day for males.
- Control blood pressure, cholesterol and blood sugar. Ask your health care team how often you need to have your blood pressure, blood sugar and cholesterol levels checked.
- Practice good sleep habits. Poor sleep may increase the risk of heart disease and other health problems. Adults should aim to get 7 to 9 hours of sleep daily. Go to bed and wake at the same time every day, including on weekends. If you have trouble sleeping, talk to a health care professional about strategies that might help.
- Manage stress. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to ease stress.
Coping and support
Some people might feel scared, sad, frustrated or depressed after having SCAD. Understanding your health and talking to others may help. Try these tips:
- Learn about SCAD. Knowing the details may make you feel more comfortable when talking to your care team. Ask about the size of your artery tear and where it is. Understand the treatments you'll receive and why you need them. Ask where you can find more information.
- Join a support group. It may be helpful to connect with others who know what you're going through. Ask your health care team if there are any SCAD or heart disease support groups in your area.
Preparing for your appointment
You may not have time to prepare. SCAD usually is diagnosed in an emergency situation. If you have chest pain or think that you're having a heart attack, immediately call 911 or your local emergency number.
After a SCAD diagnosis, you may have questions about your health. Prepare a list of questions to ask your health care provider at your next appointment, such as:
- What caused my SCAD?
- What tests do I need?
- What's the most appropriate treatment?
- Will the tear in my artery heal on its own?
- What is my risk of having another SCAD?
- Do I have a blood vessel condition, such as fibromuscular dysplasia, also called FMD?
- I have other health conditions. How can I best manage them together?
- Are there any activity or eating restrictions I need to follow?
- Is it safe for me to get pregnant?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions you have.
Sept. 16, 2023