Overview
Mitral valve prolapse and regurgitation
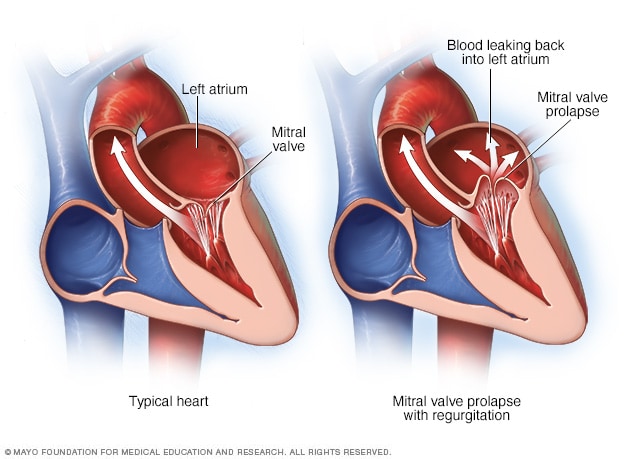
Mitral valve prolapse and regurgitation
The mitral valve separates the two chambers of the left side of the heart. In mitral valve prolapse, the valve flaps bulge into the upper left chamber during each heartbeat. Mitral valve prolapse can cause blood to leak backward, a condition called mitral valve regurgitation.
Typical heart and heart with mitral valve stenosis
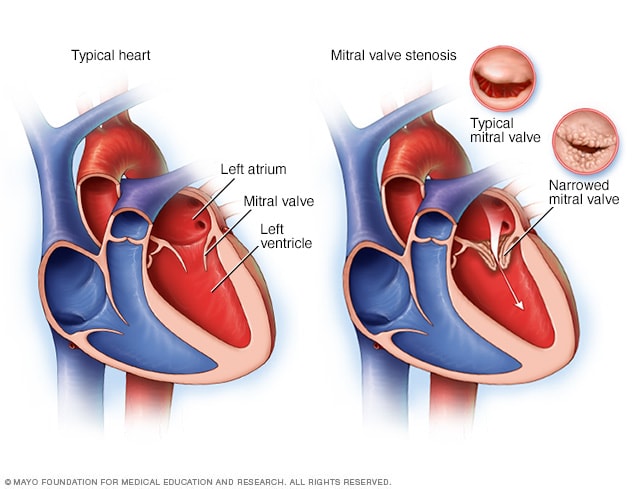
Typical heart and heart with mitral valve stenosis
Mitral valve stenosis, shown in the heart on the right, is a condition in which the heart's mitral valve is narrowed. The valve doesn't open properly, blocking blood flow coming into the left ventricle, the main pumping chamber of the heart. A typical heart is shown on the left.
Mitral valve disease is a problem with the valve located between the left heart chambers. The upper left heart chamber is called the left atrium. The bottom left heart chamber is called the left ventricle.
Mitral valve disease includes:
- Mitral valve regurgitation. The mitral valve flaps, also called leaflets, may not close tightly. This causes blood to leak backward.
- Mitral valve stenosis. The flaps of the mitral valve become thick or stiff, and they can fuse together. This narrows the valve opening, which reduces blood flow from the left atrium to the left ventricle.
Treatment for mitral valve disease depends on the severity of the condition and whether it is worsening. Sometimes, surgery is recommended to repair or replace the mitral valve.
Mayo Clinic Health Letter & Books
Join thousands of readers who trust Mayo Clinic Health Letter for reliable health tips and insights. Start your journey to better health today.
Types
Symptoms
Some people with mitral valve disease might not have symptoms for many years, if at all.
Symptoms of mitral valve disease can include:
- Fatigue.
- Irregular heartbeat.
- Shortness of breath.
When to see a doctor
If you have symptoms of mitral valve disease, you may be referred to a doctor trained in heart diseases, called a cardiologist.
Causes
Chambers and valves of the heart
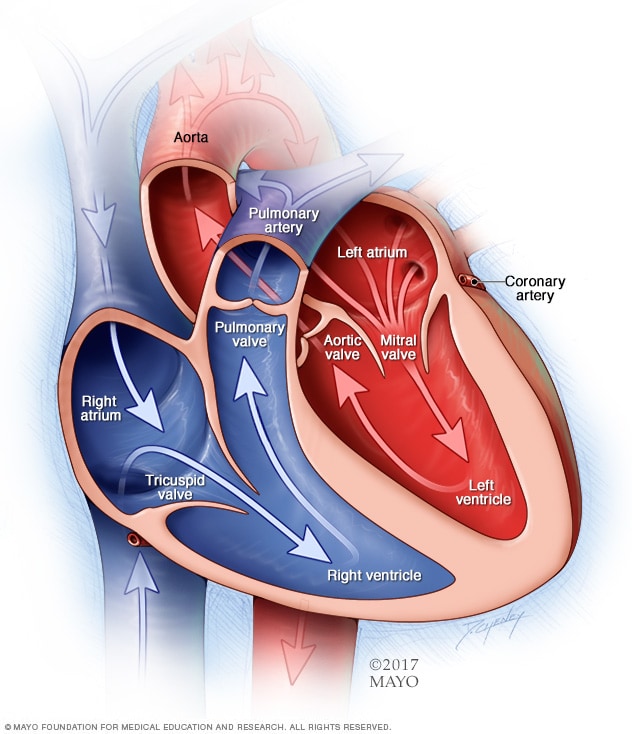
Chambers and valves of the heart
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves help keep blood flowing in the right direction.
To understand the causes of mitral valve disease, it may be helpful to know how the heart works.
The mitral valve is one of four valves in the heart that keep blood flowing in the right direction. Each valve has flaps, called leaflets, that open and close once during each heartbeat. If a valve doesn't open or close properly, blood flow through the heart to the body can be reduced.
- In mitral valve regurgitation, the flaps don't close tightly. Blood flows backward when the valve is closed, making it harder for the heart to work properly.
- In mitral valve stenosis, the valve opening narrows. The heart now must work harder to force blood through the smaller valve opening. If the opening in the valve becomes small enough, it can reduce blood flow between the left heart chambers.
Mitral valve disease has many causes. Some forms of mitral valve disease can be present at birth. A heart problem that you're born with is called a congenital heart defect.
Mitral valve disease also may develop later in life. This means it is acquired. For example, mitral valve stenosis is often caused by rheumatic fever. This fever is a complication of a strep infection that can affect the heart. When this happens, it's called rheumatic mitral valve disease.
Other causes of acquired mitral valve disease include:
- Other heart conditions.
- Infection.
- Age-related changes.
- Autoimmune disease, such as lupus.
Risk factors
Several things can increase the risk of mitral valve disease, including:
- Older age.
- Certain infections that affect the heart.
- Heart attack and some types of heart disease.
- Use of certain drugs.
- Heart condition present at birth, called a congenital heart defect.
- Radiation to the chest.
Complications
Mitral valve disease can cause many complications. Severe mitral valve regurgitation, for example, causes the heart to work harder, which can cause the left ventricle to enlarge and the heart muscle to weaken.
Other complications of mitral valve disease may include:
- Irregular and often rapid heartbeat, called atrial fibrillation.
- High blood pressure in the blood vessels in the lungs, called pulmonary hypertension.
- Blood clots.
- Congestive heart failure.
- Stroke.
Sept. 20, 2023