Diagnosis
To diagnose mitral valve disease, including mitral valve stenosis and mitral valve regurgitation, a health care professional examines you and asks questions about your medical history.
The health care professional listens to your heart with a device called a stethoscope. A whooshing sound, called a heart murmur, may be a sign of a mitral valve condition.
Tests to diagnose mitral valve disease may include:
-
Echocardiogram. Sound waves are used to create pictures of the heart in motion. This test shows how blood moves through the heart and heart valves, including the mitral valve. An echocardiogram can help in the diagnosis of congenital mitral valve disease, rheumatic mitral valve disease and other heart valve conditions.
A standard echocardiogram is done from outside the body. But sometimes, a more-detailed echocardiogram is needed to get a closer look at the mitral valve. This type of echocardiogram is called a transesophageal echocardiogram. It is done from inside the body.
- Electrocardiogram (ECG or EKG). This quick and simple test measures the heart's electrical activity. It shows how fast or how slowly the heart is beating. Sticky patches called sensors or electrodes are attached to the chest and sometimes the arms and legs. Wires connect the patches to a computer, which prints or displays results.
- Chest X-ray. A chest X-ray is a picture of the heart and lungs. It can show whether the heart is enlarged, which can be a sign of certain types of heart valve disease.
- Cardiac MRI. This test uses magnetic fields and radio waves to create detailed pictures of the heart. A cardiac MRI might be done to determine the severity of mitral valve disease.
- Exercise tests or stress tests. These tests often involve walking on a treadmill or riding a stationary bike while the heart is checked. Exercise tests help reveal how the heart responds to physical activity and whether valve disease symptoms occur during exercise. If you can't exercise, you may get medicine that affects the heart like exercise does.
-
Cardiac catheterization. A doctor guides a thin tube called a catheter through a blood vessel to an artery in the heart. Dye flows through the catheter. This makes the heart arteries show up more clearly on an X-ray.
Cardiac catheterization isn't often used to diagnose mitral valve disease, but it may be used if other tests haven't diagnosed the condition. It also may be done to see if you have coronary artery disease.
Staging
After testing confirms a diagnosis of mitral or other heart valve disease, your health care team may tell you the stage of disease. Staging helps determine the most appropriate treatment.
The stage of heart valve disease depends on many things, including symptoms, disease severity, the structure of the valve or valves, and blood flow through the heart and lungs.
Heart valve disease is staged into four basic groups:
- Stage A: At risk. Risk factors for heart valve disease are present.
- Stage B: Progressive. Valve disease is mild or moderate. There are no heart valve symptoms.
- Stage C: Asymptomatic severe. There are no heart valve symptoms, but the valve disease is severe.
- Stage D: Symptomatic severe. Heart valve disease is severe and is causing symptoms.
More Information
Treatment
Mitral valve disease treatment depends on the symptoms, the severity of the condition, and whether the condition is worsening.
A doctor trained in heart disease, called a cardiologist, typically provides care for people with mitral valve disease. Treatment of mitral valve disease might include regular health checkups to see how well you're doing. If you have mitral valve disease, you might be asked to:
- Make healthy lifestyle changes.
- Take medicines to treat symptoms.
- Take blood thinners to reduce the risk of blood clots if you have an irregular heartbeat called atrial fibrillation.
Surgery or other procedures
Minimally invasive heart surgery
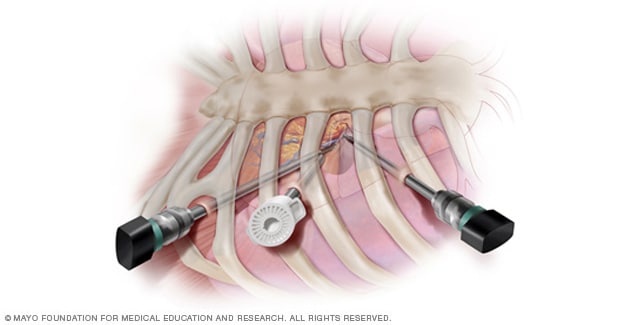
Minimally invasive heart surgery
In minimally invasive heart surgery, surgeons make small incisions in the side of the chest, between the ribs, to reach the heart. They do the surgery using long instruments.
A diseased or damaged mitral valve might eventually need to be repaired or replaced, even if you don't have symptoms. Surgery for mitral valve disease includes mitral valve repair and mitral valve replacement.
If you need surgery for another heart condition, a surgeon might do mitral valve repair or replacement at the same time.
Surgeons at some medical centers perform robot-assisted heart surgery, a type of minimally invasive heart surgery in which robotic arms are used to conduct the procedure.
Robot-assisted minimally invasive mitral valve repair at Mayo Clinic
In robot-assisted mitral valve repair surgery at Mayo Clinic, two board-certified cardiac surgeons use robotic equipment to perform the exact same procedure conducted in traditional open chest heart surgery, without needing to make a large incision through your breast bone. Your surgeons perform the procedure through small incisions in your right chest, using finger-sized instruments that are slipped in between your ribs. In this procedure, one surgeon sits at a remote console and views your heart using a magnified high-definition 3D view on a video monitor. Another surgeon works at the operating table and ensures the safe movement of the robotic arms. You'll need to be supported by a heart-lung bypass machine during the procedure. This will allow your surgeons to stop your heart briefly and insert instruments into the inner chambers to repair the mitral valve. Your surgeon uses robotic arms to duplicate specific maneuvers used in open-chest surgeries. The procedure is performed through small openings in your chest, through which will be inserted micro instruments and a thin high-definition camera tube or thoracoscope. One opening will be a mini working port through which surgeons will insert materials used during the procedure. Your surgeon performs the procedure from the remote console. Your surgeon's hand movements are translated precisely to the robotic arms at the operating table, which move like a human wrist. At the operating table, another surgeon works together with the surgeon at the console to perform the procedure and ensure it is conducted safely and efficiently. Your surgeon at the console can closely examine the complicated mitral valve problem using the high-definition 3D video monitor. This allows your surgeon to have a clearer, more lifelike perspective of your heart than is possible during open heart surgery, in which surgeons view the heart from a further distance.
To repair the mitral valve, your surgeon makes an incision in the left upper chamber or left atrium of your heart to access the mitral valve. Your surgeon can then identify the problem with your mitral valve and repair the valve itself. In mitral valve prolapse, the mitral valve, located between your heart's left atrium and the left lower chamber or left ventricle, doesn't close properly. The leaflets of the valve bulge or prolapse upward or back into the left atrium as your heart contracts. This leads to blood leaking backward into the left atrium, a condition called mitral valve regurgitation. To repair this condition, various complicated technical procedures are performed. Sometimes a small section of the leaflet, the part of the valve that doesn't close properly, is identified, and a triangular section is removed, as shown. Your surgeon then stitches the cut edges of the leaflet together to repair the valve.
In other cases, new chords or chordae supporting the broken leaflet are inserted. An annuloplasty band is then placed around the circumference of the valve to stabilize the repair. Your surgeon will close the incisions in your chest after the procedure. Mayo's staff will assist you during your recovery over a three-day period in the hospital. In robot-assisted heart surgery, most people have a quicker recovery, smaller incisions, and less pain than following open-chest surgery. Studies have also found that this procedure performed at Mayo Clinic is cost effective, with similar or lower total costs compared with traditional open-chest surgery.
Mitral valve repair
Mitral valve repair
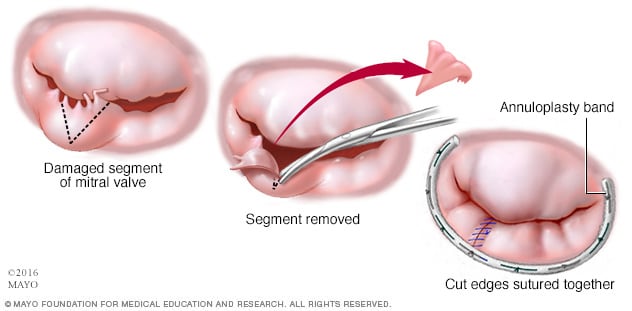
Mitral valve repair
In mitral valve repair, the surgeon removes and repairs part of the damaged mitral valve to allow the valve to fully close and stop leaking. The surgeon may tighten or reinforce the ring around a valve, called the annulus, by placing an artificial ring called an annuloplasty band.
Mitral valve repair

Mitral valve repair
In mitral valve repair, a surgeon removes the part of the mitral valve that doesn't close properly, as shown in the top image. Then the surgeon sutures together the edges and places an annuloplasty band to support the valve, as shown in the bottom image.
During mitral valve repair surgery, the surgeon might:
- Patch holes in a heart valve.
- Reconnect the valve flaps.
- Remove extra tissue from the valve so that the flaps can close tightly.
- Repair the structure of the mitral valve by replacing cords that support it.
- Separate valve leaflets that have fused.
Other mitral valve repair procedures include:
- Annuloplasty. A surgeon tightens or reinforces the ring around the valve. Annuloplasty may be done with other techniques to repair a heart valve.
- Valvuloplasty. This treatment is used to repair a mitral valve with a narrowed opening. Valvuloplasty might be done even if you don't have symptoms. The surgeon inserts a catheter with a balloon on the tip into an artery in the arm or groin and guides the catheter to the mitral valve. The balloon is inflated, widening the mitral valve opening. The balloon is deflated, and the catheter and balloon are removed.
- Mitral valve clip. In this treatment, a surgeon guides a catheter with a clip on its end to the mitral valve through an artery in the groin. The clip is used to fix a torn or leaky mitral valve leaflet. This procedure is an option for people who have severe mitral valve regurgitation or who aren't a good candidate for mitral valve surgery.
Mitral valve replacement
Repair of previously replaced valve
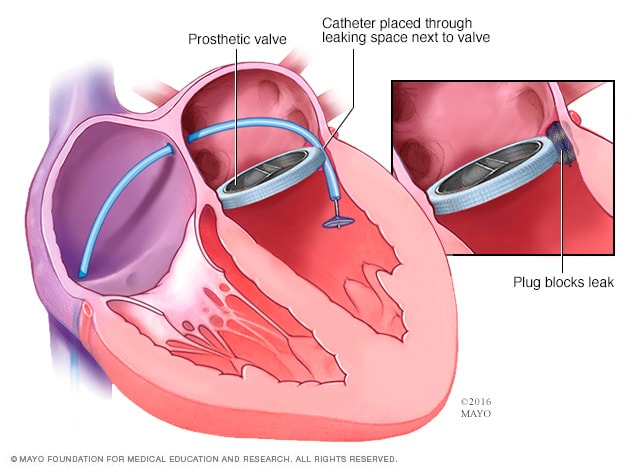
Repair of previously replaced valve
If a previously replaced mitral valve has a leak surrounding the artificial valve, a cardiologist may insert a device to stop the leak.
During mitral valve replacement, the heart surgeon removes the mitral valve and replaces it with a mechanical valve or a valve made from cow, pig or human heart tissue. A tissue valve is often called a biological tissue valve.
Sometimes, a heart catheter treatment may be done to insert a replacement valve into a biological tissue valve that is no longer working properly. This is called a valve-in-valve procedure.
If you had mitral valve replacement with a mechanical valve, you need blood thinners for life to prevent blood clots. Biological tissue valves break down over time and usually need to be replaced.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
If you have heart valve disease, including mitral valve disease, it's important to follow a healthy lifestyle. Your health care team may tell you to make lifestyle changes, including:
- Eating a heart-healthy diet. Eat a variety of fruits and vegetables, low-fat or fat-free dairy products, poultry, fish, and whole grains. Avoid saturated and trans fat, and excess salt and sugar.
- Maintaining a healthy weight. Being overweight increases the risk of heart disease. Talk with a health care professional to set realistic goals for body mass index and weight.
- Getting regular physical activity. Aim to include about 30 minutes of physical activity, such as brisk walks, into your daily fitness routine. Talk to your health care team about the amount and type of exercise that's best for you, especially if you're considering competitive sports.
- Managing stress. Find ways to help manage your stress, such as through relaxation activities, meditation, physical activity, and spending time with family and friends.
- Avoiding tobacco. If you smoke, quit. Ask a health care professional about resources to help you quit smoking. Joining a support group may be helpful.
- Avoid or limit alcohol. Heavy alcohol use can cause irregular heartbeats. Ask your health care team about the effects of drinking alcohol.
- Get regular health checkups. Establish a regular schedule with your cardiologist or primary care doctor. Tell your health care team if you have any changes in your signs or symptoms.
- Practice good sleep habits. Poor sleep may increase the risk of heart disease and other chronic conditions. Go to bed and wake at the same time every day, including on weekends. If you have trouble sleeping, talk to a health care professional about strategies that might help.
Pregnancy
If you have mitral valve disease and are thinking about getting pregnant, talk to your health care team first. Pregnancy causes the heart to work harder. How a heart with mitral valve disease tolerates this extra work depends on many things. A health care professional also can explain how to safely treat mitral valve disease during pregnancy. Frequent health checkups are needed if you have heart valve disease during pregnancy.
Coping and support
Connecting with friends and family or a support group is a good way to reduce stress. You may find that talking about mitral valve disease and your concerns with others in similar situations can help.
Preparing for your appointment
If you think you have mitral valve disease, make an appointment for a health checkup. Here's some information to help you get ready for your appointment.
What you can do
- Be aware of pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do beforehand.
- Write down your symptoms, including any that seem unrelated to mitral valve disease.
- Write down important personal information, including a family history of heart disease, and any major stresses or recent life changes.
- Make a list of all medications, vitamins and supplements you take. Include the dosages.
- Take a family member or friend along, if possible, to help you remember information you receive.
- Be prepared to discuss your diet and exercise habits. If you don't already eat well and exercise, be ready to talk about challenges you might face in getting started.
- Write down questions to ask your health care team.
For mitral valve disease, some basic questions to ask your health care team include:
- What is likely causing my symptoms or condition?
- What are other possible causes for my symptoms or condition?
- What tests will I need?
- What's the best treatment?
- What are the options to the main treatment you're suggesting?
- Is there a generic option to the medicine you're prescribing?
- I have other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Should I see a specialist?
- If I need surgery, which surgeon do you recommend for heart valve surgery?
- Are there brochures or other printed material I can take with me? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your health care team is likely to ask you several questions, including:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
Sept. 20, 2023