Diagnosis
To diagnose long QT syndrome (LQTS), a healthcare professional examines you. You are usually asked questions about your symptoms and medical and family history. The health professional listens to your heart with a device called a stethoscope that's placed against your chest. If your healthcare professional thinks you have an irregular heartbeat, tests can be done to check the heart.
Tests
Tests are done to check the health of the heart and confirm long QT syndrome (LQTS).
Electrocardiogram (ECG or EKG)
Prolonged QT interval
Prolonged QT interval
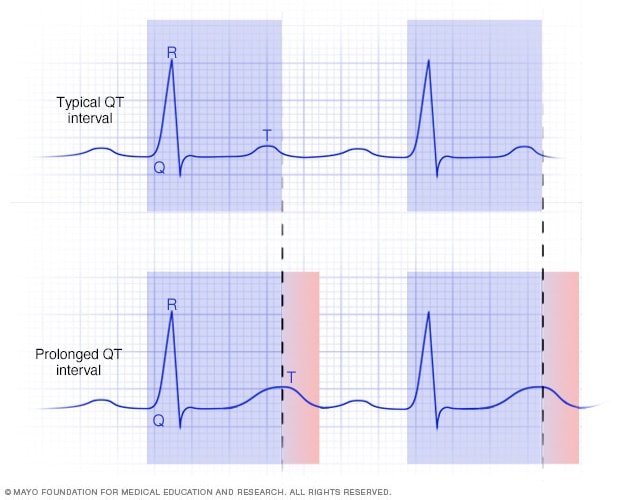
A prolonged QT interval is an irregular heart rhythm. It is a change in how the heart's bottom chambers send signals. In a prolonged QT interval, it takes longer than usual for the heart to recharge between beats. A prolonged QT interval can be seen on a heart test called an electrocardiogram.
An ECG is the most common test used to diagnose long QT syndrome. It records the electrical signals in the heart and shows how fast or how slow the heart is beating. Sticky patches called electrodes attach to the chest and sometimes the arms and legs. Wires connect the electrodes to a computer, which prints or displays the test results. The heart's signals are shown as waves on the test results.
- On an ECG, there are five waves. They use the letters P, Q, R, S and T.
- Waves Q through T show the heart signaling in the heart's lower chambers.
- The time between the start of the Q wave and the end of the T wave is called the QT interval. This is how long it takes for the heart to squeeze and refill with blood before it beats again. If the interval takes longer than usual to happen, it's called a prolonged QT interval.
An ideal QT interval depends on your age, your sex and your personal heart rate. In people who have a LQTS complication called torsades de pointes, the waves on the ECG results look twisted.
If long QT symptoms don't happen often, they may not be seen on a regular ECG. If so, your healthcare professional may ask you to wear a heart monitor at home. There are several different types.
- Holter monitor. This small, portable ECG device records the heart's activity. It's worn for a day or two while you do your regular activities.
- Event recorder. This device is like a Holter monitor, but it records only at certain times for a few minutes at a time. It's typically worn for about 30 days. You usually push a button when you feel symptoms. Some devices automatically record when an irregular heart rhythm is detected.
Some personal devices, such as smartwatches, have sensors that can take an ECG. Ask your healthcare professional if this is an option for you.
Exercise stress tests
These tests often involve walking on a treadmill or pedaling a stationary bike. A member of your care team checks your heart activity as you exercise. Exercise stress tests show how the heart reacts to physical activity. If you can't exercise, you may get medicine that increases the heart rate like exercise does. Sometimes an echocardiogram is done during a stress test.
Genetic testing
A genetic test is available to confirm long QT syndrome (LQTS). The test checks for gene changes that can cause the disorder. Check with your insurer to see if it is covered.
If you have long QT syndrome, your healthcare team may suggest that other family members also get genetic testing to check for the disorder.
Genetic tests for long QT syndrome can't find all inherited cases of long QT syndrome. It's recommended that families speak to a genetic counselor before and after testing.
More Information
Treatment
Treatment for long QT syndrome (LQTS) may include:
- Lifestyle changes.
- Medicines.
- A medical device.
- Surgery.
The goals of LQTS treatment are to:
- Prevent irregular heartbeats.
- Prevent sudden cardiac death.
Your healthcare professional talks with you about your treatment options. Treatment depends on your symptoms and your type of long QT syndrome. You may need treatment even if you don't often have symptoms.
Therapies
Some people with acquired long QT syndrome may get fluids or minerals, such as magnesium, through a needle in a vein.
Medications
If medicine causes long QT syndrome (LQTS), stopping the medicine may be all that's needed to treat the disorder. Your healthcare professional can tell you how to safely do so. Do not change or stop taking any medicines without talking to your healthcare team.
Some people with LQTS need medicines to treat symptoms and prevent life-threatening heart rhythm changes.
Medicines used to treat long QT syndrome may include:
- Beta blockers. These medicines slow the heart rate. They reduce the chances of having a long QT episode. Beta blockers used to treat long QT syndrome include nadolol (Corgard) and propranolol (Inderal LA, InnoPran XL).
- Mexiletine. Taking this heart rhythm medicine with a beta blocker might help shorten the QT interval. It can help lower the risk of fainting, seizure or sudden cardiac death.
Surgery or other procedures
Some people with long QT syndrome need surgery or a device to control the heartbeat. Surgery or other procedures used for LQTS treatment may include:
- Left cardiac sympathetic denervation (LCSD) surgery. This surgery may be done if you have long QT syndrome and continuing heart rhythm changes but beta blockers don't work for you. It doesn't cure long QT syndrome. Instead, the surgery helps lower the risk of sudden cardiac death. In this treatment, surgeons remove specific nerves along the left side of the spine. These nerves are part of the body's sympathetic nervous system, which helps control the heart rhythm.
-
Implantable cardioverter-defibrillator (ICD). This device is placed under the skin near the collarbone. It continuously checks the heart rhythm. If the device finds an irregular heartbeat, it sends out low- or high-energy shocks to reset the heart's rhythm.
Most people with long QT syndrome don't need an ICD. But the device may be suggested for some athletes to help them return to competitive sports. The decision to place an ICD, especially in children, needs to be carefully considered. Placing an ICD requires surgery. Sometimes the device may send out shocks that aren't needed. Talk with your healthcare team about the benefits and risks of an ICD.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Your healthcare professional may suggest lifestyle changes to help you manage long QT syndrome (LQTS). These changes can lower the risk of a fainting spell or sudden cardiac death linked with LQTS.
- Know which sports are safe. You may be able to stay fully active in sports, including competitive sports. But talk to your healthcare team first. In general, people with long QT syndrome should never swim alone. Physical activities are likely to be okay if you take someone along who can help if you faint.
- Check for startling sounds. Turn down the volume on doorbells and other devices such as phones that may startle you, especially during sleep. Things that startle you can cause you to pass out.
- Control emotions. Being very excited, angry or surprised can trigger heartbeat changes in some people with long QT syndrome. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to reduce stress.
- Check your medicines. Don't take medicines that could cause prolonged QT intervals. If you're not sure whether you take such medicines, ask your healthcare professional. It's a good idea to let your healthcare team know about all the medicines and supplements you take, even those you buy without a prescription.
- Get regular health checkups. If you have changes in your symptoms or overall health, your care team may update your treatment plan or suggest more treatments.
Coping and support
Worrying about possible dangerous heart rhythms linked with long QT syndrome (LQTS) may cause stress for you and your loved ones. Here are some things that might help you manage your condition.
- Tell other people you have LQTS. Make family, friends, teachers, neighbors, and anyone else who has regular contact with you aware of your heart rhythm disorder and your symptoms. Wear a medical alert identification to show others that you have LQTS.
- Have an emergency plan. Family members may want to learn cardiopulmonary resuscitation (CPR) so they can help if you ever need it. It may be appropriate to have or be able to rapidly get an automated external defibrillator (AED).
- Seek support or counseling. It might be helpful to join a support group, where you can share your experiences and feelings with others who are familiar with long QT syndrome. Families with inherited long QT syndrome also might find it helpful to talk to a genetic counselor.
Preparing for your appointment
If you have pounding, fast or irregular heartbeats, make an appointment for a health checkup. You may be sent to a doctor trained in heart conditions. This type of healthcare professional is called a cardiologist.
You also might see a doctor trained in heart rhythm disorders, called an electrophysiologist.
Here's some information to help you prepare for your appointment and know what to expect from your healthcare team.
What you can do
- Write down any symptoms you've had, and for how long. Include those that may not seem related to long QT syndrome.
- Write down important medical information, including any other health conditions you have and the names and doses of any medicines that you take. It's also important to share any family history of irregular heartbeats or sudden death with your healthcare professional.
- Write down the questions you want to be sure to ask your healthcare professional.
Questions to ask the healthcare professional at your first appointment include:
- What is likely causing my symptoms?
- Are there any other possible causes for these symptoms?
- What tests do I need?
- Should I see a specialist?
Questions to ask if you're sent to a cardiologist or electrophysiologist include:
- Do I have long QT syndrome? If so, which type?
- What is my risk of complications?
- What treatment do you recommend?
- If you're recommending medicines, what are the possible side effects?
Questions to ask if your healthcare professional recommends surgery include:
- How will this type of surgery help me?
- Where should I have my surgery done?
- What should I expect from my recovery and rehabilitation after surgery?
Other questions include:
- Do I need frequent health checkups and long-term treatment?
- What emergency symptoms of long QT syndrome should I be aware of?
- What activity restrictions do I need to follow?
- What type of lifestyle changes do you recommend?
- What medicines should I avoid taking?
- What is my long-term outlook with treatment?
- Is it safe for me to become pregnant in the future?
- What is the risk that my future children will have long QT syndrome?
- How can genetic counseling help my family?
Don't hesitate to ask other questions.
What to expect from your doctor
Your healthcare team may ask:
- What are your symptoms?
- When did the symptoms start?
- Have the symptoms gotten worse over time?
- Do strong emotions, such as anger, excitement or surprise, trigger your symptoms?
- Does exercise cause symptoms?
- Does being startled — such as by a doorbell or phone ringing — trigger your symptoms?
- Do you ever feel dizzy or lightheaded?
- Have you ever fainted?
- Have you ever had a seizure?
- What other medical conditions do you have?
- Does anyone in your family have a heart condition or heart rhythm disorder?
- Has a parent, brother, sister or child ever died by drowning or an unexpected cause?
- What medicines are you currently taking?
- Have you ever used illegal drugs? If so, which ones?
- Do you use caffeine? How much?
Knowing as much as possible about your health and your family's health history helps your healthcare team learn your diagnosis and plan treatment.
What you can do in the meantime
While you wait for your appointment, ask your family members if anyone you're related to has a family history of long QT syndrome or unexplained death.