Overview
Gamma Knife radiosurgery is a type of radiation therapy. It can be used to treat tumors, veins that have developed differently than usual and other differences in the brain.
Similar to other types of stereotactic radiosurgery (STS), Gamma Knife radiosurgery is not a standard surgery because there is no cut, called an incision.
Instead, Gamma Knife radiosurgery focuses many tiny beams of radiation on a tumor or other target with extreme accuracy. Each beam has very little effect on the brain tissue it passes through. But a strong dose of radiation is delivered to the place where all the beams meet.
Gamma Knife stereotactic radiosurgery
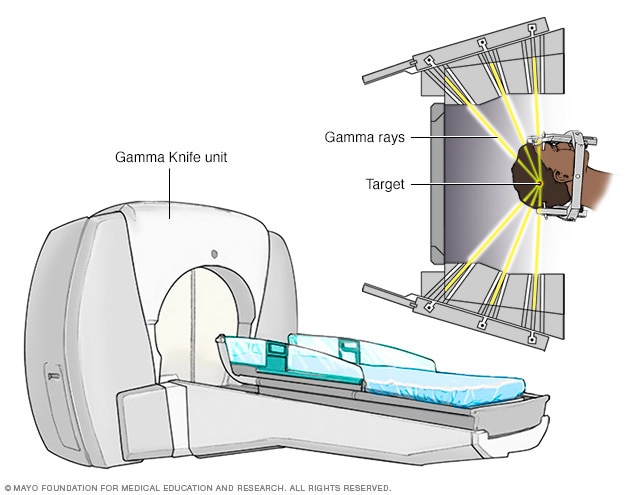
Gamma Knife stereotactic radiosurgery
Stereotactic radiosurgery technology uses many small gamma rays to deliver a precise dose of radiation to the target.
The ability to deliver radiation so precisely means that very little radiation gets to healthy tissues surrounding the target.
Gamma Knife radiosurgery is usually done one time in a single day.
Why it's done
Gamma Knife radiosurgery is often safer than standard brain surgery, also called neurosurgery. Standard surgery requires making incisions in the scalp, skull and membranes surrounding the brain, and cutting into brain tissue. This type of radiation treatment is usually performed when:
- A tumor or other difference in the brain is too hard to reach with standard neurosurgery.
- A person isn't healthy enough for standard surgery.
- A person prefers a less invasive treatment.
In most cases, Gamma Knife radiosurgery has fewer side effects compared with other types of radiation therapy. This type of surgery can be done in one day compared with up to 30 treatments with typical radiation therapy.
Gamma Knife radiosurgery is most commonly used to treat the following conditions:
-
Brain tumor. Radiosurgery can manage small noncancerous, also called benign, brain tumors. Radiosurgery also can manage cancerous, also called malignant, brain tumors.
Radiosurgery damages the genetic material known as DNA in the tumor cells. The cells cannot reproduce and may die, and the tumor may gradually get smaller.
-
Arteriovenous malformation (AVM). AVMs are tangles of arteries and veins in the brain. These tangles are not typical. In an AVM, blood flows from the arteries to veins, moving past smaller blood vessels, also called capillaries. AVMs, if not treated, may "steal" the typical flow of blood from the brain. This can cause a stroke or lead to bleeding in the brain.
Radiosurgery causes the blood vessels in the AVM to close off over time. This lowers the risk of bleeding.
-
Trigeminal neuralgia. The trigeminal nerves move sensory information between the brain and areas of the forehead, cheek and lower jaw. Trigeminal neuralgia causes facial pain that feels like an electric shock.
After treatment, pain relief can happen within a few days to a few months.
-
Acoustic neuroma. An acoustic neuroma, also called a vestibular schwannoma, is a noncancerous tumor. This tumor develops along the nerve that controls balance and hearing and leads from the inner ear to the brain.
When the tumor puts pressure on the nerve, you can experience hearing loss, dizziness, loss of balance and ringing in the ear, also called tinnitus. As the tumor grows, it also can put pressure on the nerves that control sensations and muscle movement in the face.
Radiosurgery may stop the growth of an acoustic neuroma.
-
Pituitary tumors. Tumors of the bean-sized gland at the base of the brain, called the pituitary gland, can cause several problems. The pituitary gland controls hormones in the body that control various functions, such as stress response, metabolism and sexual function.
Radiosurgery can be used to shrink the tumor and lessen the irregular secretion of pituitary hormones.
Risks
Gamma Knife radiosurgery doesn't involve surgical openings, so it's generally less risky than standard neurosurgery. In standard neurosurgery, there are possible complications associated with anesthesia, bleeding and infection.
Early complications or side effects are usually temporary. Some people experience mild headaches, a tingling sensation on the scalp, nausea or vomiting. Other side effects may include:
- Fatigue. Tiredness and fatigue may occur for the first few weeks after Gamma Knife radiosurgery.
- Swelling. Swelling in the brain at or near the treatment site can cause several symptoms depending on what areas of the brain are involved. If post-treatment swelling and symptoms do occur from the Gamma Knife treatment, these symptoms usually show up about six months after treatment rather than immediately after the procedure like with standard surgery. Your health care professional may prescribe anti-inflammatory medicines, such as corticosteroids, to prevent such problems or to treat symptoms if they appear.
-
Scalp and hair problems. The skin on the scalp may change color or be irritated or sensitive at the four sites where the head frame was attached to the head during the treatment. But the head frame does not leave any permanent marks on the scalp. Rarely, some people temporarily lose a small amount of hair if the area being treated is right under the scalp.
Rarely, people may experience late side effects, such as other brain or nerve problems, months or years after Gamma Knife radiosurgery.
How you prepare
Food and medicines
- Don't eat or drink anything after midnight the night before the procedure.
- Talk to a member of your health care team about whether you can take your regular medicines the night before or morning of the procedure.
Clothing and personal items
Wear comfortable, loose clothing.
Avoid wearing the following items during the procedure:
- Jewelry.
- Eyeglasses.
- Contact lenses.
- Makeup.
- Nail polish.
- Dentures.
- Wigs or hairpieces.
Other precautions
Tell a member of your health care team if you:
- Are taking pills or injections to control diabetes.
- Are allergic to shellfish or iodine — both are chemically related to special dyes that may be used during the procedure.
- Have implanted medical devices in your body, such as a pacemaker, artificial heart valve, aneurysm clips, neurostimulators or stents.
- Experience claustrophobia.
What you can expect
Before the procedure
Before the procedure begins, a lightweight frame will be attached to your head with four pins. This frame will keep your head stable during the radiation treatment. The frame also will serve as a point of reference for focusing the beams of radiation. During this process:
- Your hair will not be shaved, but your forehead and the back of your head will be cleaned with rubbing alcohol.
- You'll receive numbing shots in the four places on the scalp where the pins will be inserted — two points on the forehead and two at the back of the head.
After the head frame is attached, imaging of the brain is performed to show the location of the tumor or other target in relation to the head frame. The type of scan used depends on the condition being treated:
-
Tumors. Imaging for tumors may include computerized tomography (CT) or magnetic resonance imaging (MRI). In a CT scan, a series of X-rays creates a detailed image of the brain. In an MRI scan, a magnetic field and radio waves create detailed images of the brain.
A small needle may be placed in the back of the hand or in the arm to inject a dye into a blood vessel. The dye helps with viewing the blood vessels in the brain and highlights blood circulation. In some cases, you may have both MRI and CT scans.
-
Arteriovenous malformations (AVMs). Imaging for brain AVMs usually includes MRI scans, and cerebral angiograms.
In a cerebral angiogram, a doctor inserts a small tube in a blood vessel in your groin and threads it to the brain using X-ray imaging. Dye is injected through the blood vessels so they can be seen on X-rays. Your doctor may inject a dye into a blood vessel during CT or MRI scans to view the blood vessels and highlight blood circulation.
- Trigeminal neuralgia. An MRI is used to create images of nerve fibers to select a target area for treating trigeminal neuralgia.
The results of the brain scans are fed into a computer. A specialized planning program helps the radiosurgery team to figure out which areas to treat, doses of radiation and how to focus the radiation beams to treat the areas. This planning process usually takes less than an hour. During that time, you can relax in another room, but the frame must remain attached to your head.
Children often get medicines to put them in a sleep-like state for the imaging tests and the radiosurgery. Adults are usually awake, but may be given a medicine to help them relax.
During the procedure
You'll lie on a bed that slides into the Gamma Knife machine. The head frame attaches securely to a helmet inside the machine.
You'll get an intravenous (IV) tube that delivers fluids to your bloodstream to keep you hydrated during the day. A needle at the end of the IV is placed in a vein, most likely in your arm.
The time needed to complete the procedure may range from less than an hour to about four hours. It depends on the size and shape of the target. During the procedure:
- You won't feel the radiation.
- You won't hear any noise from the machine.
- You'll be able to talk with the health care team via a microphone.
Radiation oncologist monitoring Gamma Knife procedure

Radiation oncologist monitoring Gamma Knife procedure
A radiation oncologist monitors the Gamma Knife procedure in progress.
Gamma Knife radiosurgery is usually an outpatient procedure, but the entire process may last into the afternoon. You may be asked to bring along a family member or friend who can be with you during the day and who can take you home. Rarely, you may stay overnight in the hospital.
Gamma Knife delivery of radiation
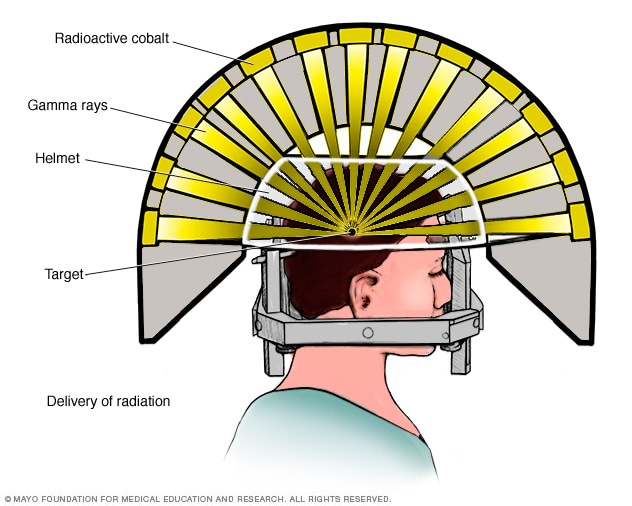
Gamma Knife delivery of radiation
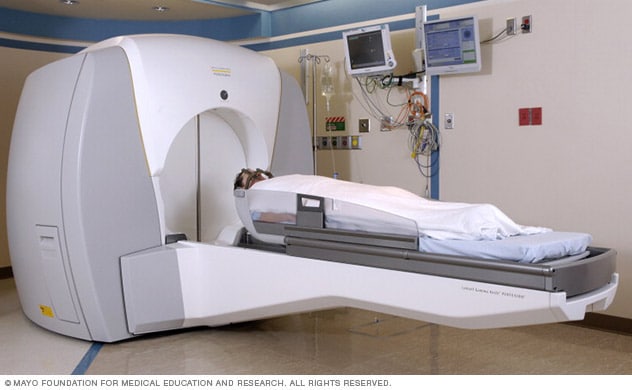 Stereotactic radiosurgery system at Mayo Clinic
Stereotactic radiosurgery system at Mayo Clinic
After the procedure
After the procedure, you might expect the following:
- The head frame will be removed.
- You may have minor bleeding or tenderness at the pin sites.
- If you experience headache, nausea or vomiting after the procedure, you'll receive medicines.
- You'll be able to eat and drink after the procedure.
Results
Gamma Knife radiosurgery results

Gamma Knife radiosurgery results
Gamma Knife radiosurgery uses multiple tiny beams of radiation to shrink tumors. The left brain scan shows a pretreatment image of a noncancerous tumor — an image enhanced by the use of a special dye, called a contrast agent. At six months after treatment (middle image), the tumor appears slightly larger but doesn't take up as much of the contrast agent — isn't as bright in the center. This indicates a positive treatment effect. At seven years (right scan), the tumor appears much smaller.
Brain AVM before and after Gamma Knife treatment

Brain AVM before and after Gamma Knife treatment
Brain arteriovenous malformation (AVM) before Gamma Knife treatment (left) and 52 months after the procedure (right)
Brain tumor before and after Gamma Knife treatment
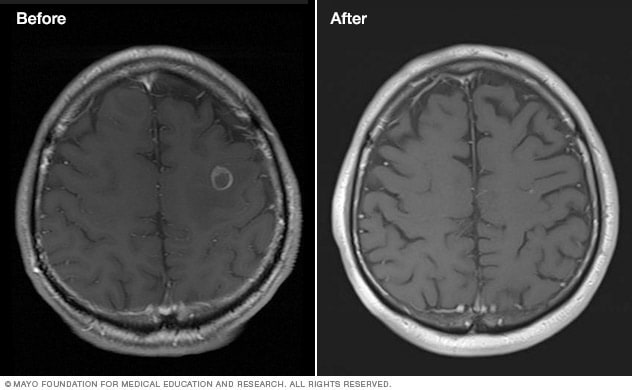
Brain tumor before and after Gamma Knife treatment
Malignant brain tumor before (left) and 111 months after Gamma Knife stereotactic radiosurgery (right)
The treatment effect of Gamma Knife radiosurgery occurs slowly, depending on the condition being treated:
- Benign tumors. Gamma Knife radiosurgery keeps tumor cells from reproducing. The tumor may shrink over a period of months to years. But the main goal of Gamma Knife radiosurgery for noncancerous tumors is to prevent any future tumor growth.
- Malignant tumors. Cancerous tumors may shrink quickly, often within a few months.
- Arteriovenous malformations (AVMs). The radiation therapy causes the atypical blood vessels of brain AVMs to thicken and close off. This process may take two years or more.
-
Trigeminal neuralgia. Gamma Knife radiosurgery creates a wound that blocks pain signals from moving along the trigeminal nerve. Pain relief may take several months.
You'll have follow-up exams to monitor your progress.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.