April 03, 2021
Dyspnea, cough, sputum production and recurrent respiratory infections are frequently encountered clinical concerns leading patients to seek medical care. Recognition of dynamic central airway obstruction or collapse during respiration has also been associated with these symptoms.
"Identification of expiratory central airway collapse (ECAC) is usually challenging," says Sebastian Fernandez-Bussy, M.D., Pulmonary Medicine, at Mayo Clinic in Jacksonville, Florida. "Patients with ECAC often present with multiple comorbidities — such as chronic obstructive pulmonary disease, bronchiectasis, asthma, gastroesophageal reflux disease, vocal cord dysfunction, obstructive sleep apnea and laryngopharyngeal reflux — that manifest with similar symptoms. These comorbidities often coexist with ECAC and these conditions are not mutually exclusive."
Inspiration view of the distal trachea
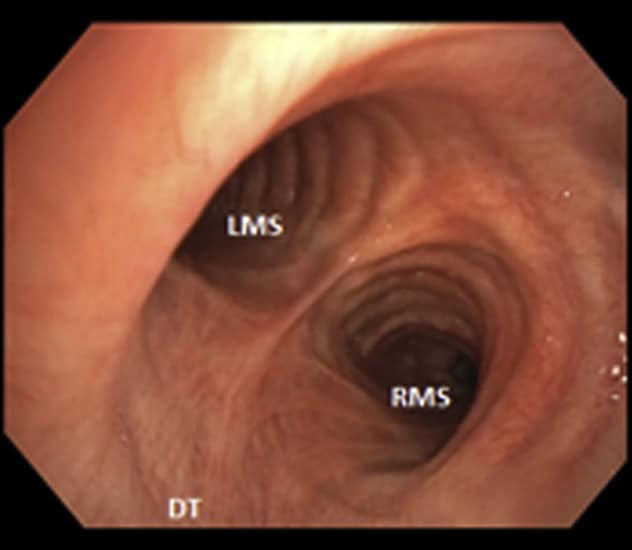
Inspiration view of the distal trachea
Distal trachea (DT), left main stem (LMS) and right main stem (RMS) on inspiration
Expiration view of the distal trachea
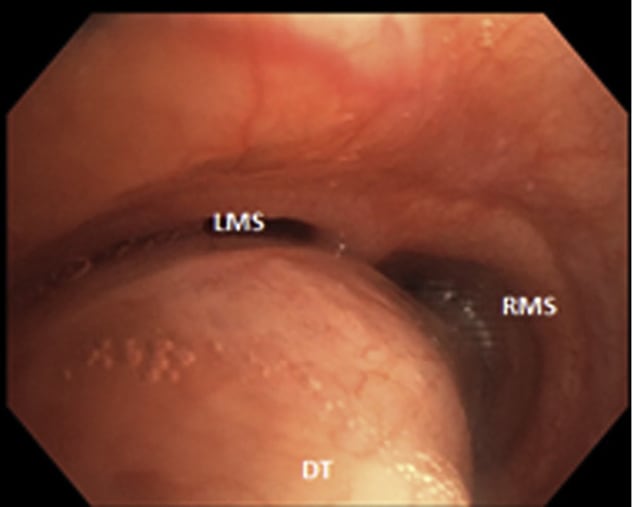
Expiration view of the distal trachea
Distal trachea (DT), left main stem (LMS) and right main stem (RMS) on forced expiration exhibiting severe excessive dynamic airway collapse
ECAC comprises two pathophysiologic entities: excessive dynamic airway collapse and tracheobronchomalacia. Excessive dynamic airway collapse refers to an excessive forward displacement of the posterior membranous portion of the tracheal wall due to weakness and atrophy of the longitudinal elastic fibers. Abnormal motion of the anterolateral or cartilaginous portion of the tracheobronchial wall is termed tracheobronchomalacia.
The true prevalence of ECAC is unknown, although an overall prevalence of 13% has been suggested in research published in Archivos de Bronconeumologia and Journal of Cardiothoracic and Vascular Anesthesia in 2019. The prevalence increases to 37% in patients with chronic obstructive pulmonary disease and other airway diseases. The etiology of ECAC is uncertain, but the following all have been linked to the development of ECAC:
- Small airway obstruction
- Chronic inflammation
- Trauma or previous tracheostomy
- Relapsing polychondritis and other autoimmune diseases
- Chronic obstructive pulmonary disease
- Asthma
- Obesity
- Gastroesophageal reflux disease
Diagnosis of ECAC
"The clinical manifestations of ECAC are so common and nonspecific that diagnosis is often delayed," says Dr. Fernandez-Bussy. Pulmonary function tests may reveal obstructive (44%) or restrictive (17.8%) changes, but test results are normal in 20% of patients with ECAC, as noted in research published in Thoracic Surgery Clinics in 2018 and Archivos de Bronconeumologia in 2019. Dynamic computerized tomography of the chest with images obtained at end inspiration and during forced expiration is increasingly used to establish the presence of ECAC, but its utility is predicated on radiology expertise for both image collection and interpretation.
Dynamic flexible bronchoscopy under light or moderate sedation remains the most reliable test to confirm ECAC and is still considered the criterion standard. Throughout the procedure, the patient must be able to purposefully produce a forced expiration as the bronchoscopist evaluates each segment of the central airways. Disease severity is described as mild disease with airway collapse of 70% to 80%, moderate with airway collapse of 81% to 90%, and severe with airway collapse of 91% or higher.
Stent trial confirms potential benefit
Dr. Fernandez-Bussy notes: "Corrective tracheobronchoplasty surgery can be beneficial for many patients; however, some degree of certainty about its potential benefit for patients is required before it can be performed. This certainty can be obtained through a stent trial. Before surgery, all treatments for respiratory comorbidities should be optimized for at least four to eight weeks, because up to 40% of patients will report substantial improvement in symptoms, even in the absence of airway stabilization.
"In addition, not treating the comorbidities may negatively affect the outcome of surgical central airway stabilization. Commonly, airway stents are placed for a short period of time (five to 10 days) to assess clinical improvement and help identify those patients who may benefit from surgery."
Dr. Fernandez-Bussy also notes that these evaluations should be made using validated scoring scales before and during stenting:
- Subjective and objective assessment of respiratory symptoms
- Health-related quality of life via the St. George's Respiratory Questionnaire and Cough Quality of Life Questionnaire
- Lung function (forced expiratory volume)
- Exercise capacity (six-minute walk test)
- Functional status via the Karnofsky performance status scale
Treatment recommendations
Therapy for ECAC is determined by disease severity — degree of collapse and severity of symptoms — and comorbid conditions. "Optimization of pulmonary status with attention to appropriate treatment of recurrent infections, maximization of medical therapy for concomitant airway diseases, and use of bronchial hygiene measures are critical to management," Dr. Fernandez-Bussy continues. "Maximal treatment of any potential alternative cause of symptoms for four to eight weeks is recommended before diagnosing ECAC as the primary cause of symptoms.
"Mild to moderate cases can be treated with intermittent continuous or bilevel positive airway pressure, but tracheobronchoplasty or surgical central airway stabilization by posterior mesh splinting should be considered for patients with severe disease. Surgical planning for tracheobronchoplasty requires distinguishing excessive dynamic airway collapse from tracheobronchomalacia. In patients with excessive dynamic airway collapse, the transverse diameter of the airway is not excessively large; therefore, lateral downsizing of the trachea is less pronounced than in the technique for repairing tracheobronchomalacia.
"When repairing excessive dynamic airway collapse, the posterior wall tension may be predominantly developed by suture placement to achieve axial tension. Tracheobronchoplasty is performed by suturing a knitted polypropylene mesh to the posterior membrane of the trachea and bilateral main bronchi, with the goal of splinting the trachea to promote the development of normal rigidity and configuration with healing. Robotic tracheobronchoplasty has reported promising results and favorable outcomes.
"Bronchoscopic application of thermoablative techniques to the posterior tracheal wall to induce fibrosis and wall rigidity holds promise as a less invasive therapy; however, more clinical trials are needed to establish its real value."
Dr. Fernandez-Bussy concludes: "Expiratory central airway collapse is an underdiagnosed disorder that can coexist with and mimic asthma, chronic obstructive pulmonary disease and bronchiectasis. Common manifestations include dyspnea, chronic cough and recurrent respiratory infections.
"Dynamic flexible bronchoscopy is the diagnostic criterion standard. Optimization of bronchial hygiene, treatment of coexisting conditions, and use of positive airway pressure therapy are used in mild to moderate cases of ECAC. Definitive surgical treatment should be considered for those with severe disease, especially if a diagnostic stent trial reports quantified improvement."
For more information
Kheir F, et al. Excessive dynamic airway collapse or tracheobronchomalacia: Does it matter? Archivos de Bronconeumologia. 2019;55:69.
Diaz Milian R, et al. Expiratory central airway collapse in adults: Anesthetic implications (Part 1). Journal of Cardiothoracic and Vascular Anesthesia. 2019;33:2546.
Wright CD. Tracheobronchomalacia and expiratory collapse of central airways. Thoracic Surgery Clinics. 2018;28:163.
St. George's Respiratory Questionnaire. St. George's University of London.
Cough Quality of Life Questionnaire. Mapi Research Trust.
Karnofsky performance status scale. MDCalc.