Diagnosis
Diagnosing vulvar cancer
Tests and procedures used to diagnose vulvar cancer include:
- Examining your vulva. Your doctor will likely conduct a physical exam of your vulva to look for abnormalities.
- Using a special magnifying device to examine your vulva. During a colposcopy exam, your doctor uses a device that works like a magnifying glass to closely inspect your vulva for abnormal areas.
- Removing a sample of tissue for testing (biopsy). To determine whether an area of suspicious skin on your vulva is cancer, your doctor may recommend removing a sample of skin for testing. During a biopsy procedure, the area is numbed with a local anesthetic and a scalpel or other special cutting tool is used to remove all or part of the suspicious area.
Determining the extent of the cancer
Once your diagnosis is confirmed, your doctor works to determine the size and extent (stage) of your cancer. Staging tests can include:
- Examination of your pelvic area for cancer spread. Your doctor may do a more thorough examination of your pelvis for signs that the cancer has spread.
- Imaging tests. Images of your chest or abdomen may show whether the cancer has spread to those areas. Imaging tests may include X-ray, computerized tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography (PET).
The stages of vulvar cancer are indicated by Roman numerals that range from I to IV, with the lowest stage indicating cancer that is limited to the vulva. By stage IV, the cancer is considered advanced and has spread to nearby structures, such as the bladder or rectum, or to distant areas of the body.
More Information
Treatment
Vulvectomy
Vulvectomy
Vulvectomy
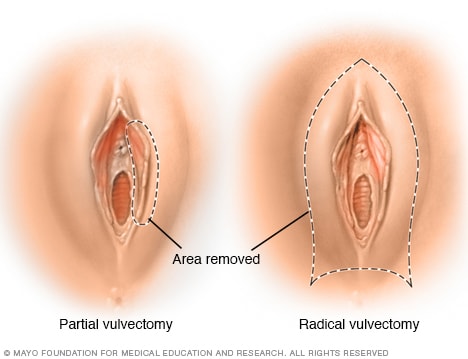
Treatment for vulvar cancer may involve removing part of the vulva (partial vulvectomy) or the entire vulva (radical vulvectomy).
Treatment options for vulvar cancer depend on the type, stage and location of your cancer, as well as your overall health and your preferences.
Surgery
Operations used to treat vulvar cancer include:
- Removing the cancer and a margin of healthy tissue (excision). This procedure, which may also be called a wide local excision or radical excision, involves cutting out the cancer and a small amount of normal tissue that surrounds it. Cutting out what doctors refer to as a margin of normal-looking tissue helps ensure that all of the cancerous cells have been removed.
- Removing part of the vulva or the entire vulva (vulvectomy). Surgery to remove part of the vulva (partial vulvectomy) or the entire vulva, including the underlying tissue (radical vulvectomy), may be an option for larger cancers. People with larger cancers may also consider treatment that combines radiation therapy and chemotherapy to shrink the tumor before surgery, which may allow for a less extensive operation.
- Removing a few nearby lymph nodes (sentinel node biopsy). To determine whether cancer has spread to the lymph nodes, the surgeon may use a procedure called sentinel node biopsy. This procedure identifies the lymph nodes most likely to contain cancer so they can be removed and analyzed. If cancer isn't found in those first lymph nodes, it's unlikely to be in any other lymph nodes.
- Removing many lymph nodes. If the cancer has spread to the lymph nodes, many lymph nodes may be removed to reduce the risk that cancer will spread to distant areas of the body.
Surgery carries a risk of complications, such as infection and problems with healing around the incision. Removing lymph nodes can cause fluid retention and leg swelling, a condition called lymphedema.
Radiation therapy
Radiation therapy uses high-powered energy beams, such as X-rays and protons, to kill cancer cells. Radiation therapy for vulvar cancer is usually administered by a machine that moves around your body and directs radiation to precise points on your skin (external beam radiation).
Radiation therapy is sometimes used to shrink large vulvar cancers in order to make it more likely that surgery will be successful. Radiation therapy is sometimes combined with chemotherapy, which can make cancer cells more vulnerable to the radiation.
If cancer cells are discovered in your lymph nodes, your doctor may recommend radiation to the area around your lymph nodes to kill any cancer cells that might remain after surgery. Radiation is sometimes combined with chemotherapy in these situations.
Chemotherapy
Chemotherapy is a drug treatment that uses chemicals to kill cancer cells. Chemotherapy drugs are typically administered through a vein in your arm or by mouth.
For those with advanced vulvar cancer that has spread to other areas of the body, chemotherapy may be an option.
Chemotherapy is sometimes combined with radiation therapy to shrink large vulvar cancers in order to make it more likely that surgery will be successful. Chemotherapy may also be combined with radiation to treat cancer that has spread to the lymph nodes.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Targeted therapy might be an option for treating advanced vulvar cancer.
Immunotherapy
Immunotherapy uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process.
Immunotherapy might be an option for treating advanced vulvar cancer.
Follow-up tests after treatment
After completing vulvar cancer treatment, your doctor may recommend periodic follow-up exams to look for a cancer recurrence. Even after successful treatment, vulvar cancer can return. Your doctor will determine the schedule of follow-up exams that's right for you, but doctors generally recommend exams two to four times each year for the first two years after vulvar cancer treatment.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
Living with vulvar cancer can be challenging. Although there are no easy answers for coping with vulvar cancer, the following suggestions may help:
- Learn enough about vulvar cancer to feel comfortable making treatment decisions. Ask your doctor to explain the basics of your cancer, such as what types of cells are involved and the stage of your cancer. Also ask your doctor or nurse to recommend good sources of information. Learn enough about your cancer so that you feel comfortable asking questions and discussing your treatment options with your doctor.
- Talk to someone about your feelings. When you feel ready, consider talking to someone you trust about your hopes and fears as you face cancer treatment. This might be a friend, a family member, your doctor, a social worker, a spiritual adviser or a counselor.
- Connect with other cancer survivors. You may find it helpful to talk to other people with vulvar cancer. They can tell you how they've coped with problems similar to the ones you're facing. Ask your doctor about support groups in your area. Or contact support organizations, such as the American Cancer Society. Online message boards, such as those offered by the American Cancer Society's Cancer Survivors Network, also can connect you to others with vulvar cancer.
- Don't be afraid of intimacy. Your natural reaction to changes in your body may be to avoid intimacy. Although it may not be easy, discuss your feelings with your partner. You may also find it helpful to talk to a therapist, either on your own or together with your partner. Remember that you can express your sexuality in many ways. Touching, holding, hugging and caressing may become far more important to you and your partner.
Preparing for your appointment
Your first appointment will usually be with either your primary care doctor or a gynecologist. If your doctor or gynecologist suspects or diagnoses cancer, you'll likely be referred to a gynecologic oncologist who specializes in surgery for gynecologic cancers.
Because appointments can be brief, and it can be difficult to remember everything you want to discuss, it's a good idea to be prepared. Here are some suggestions for preparing, and what you can expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions, such as restricting your diet before your appointment.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements that you're taking.
- Ask a relative or friend to accompany you, to help you remember what the doctor says.
- Write down questions to ask your doctor.
Your time with your doctor is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For vulvar cancer, some basic questions to ask include:
- What kinds of tests will I need?
- Do I need to do anything to prepare for these tests?
- Other than vulvar cancer, are there any other possible causes for these symptoms?
- What type of vulvar cancer do I have?
- What stage is my cancer?
- What types of surgical options are available to me?
- What kind of success rates does each type of surgery have?
- What are the drawbacks to each type of surgery?
- Will I need to wear an ostomy bag?
- What about radiation or chemotherapy? Are those options available to me?
- What kind of success rates do those therapies have?
- What types of side effects does each treatment have?
- How will these treatments affect my sexuality?
- Will I be able to have children after treatment?
- How should I prepare for treatment?
- Which course of action do you recommend?
- What are the odds of recurrence?
- What is my prognosis?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask other questions that occur to you.
What to expect from your doctor
Your doctor will likely have a number of questions for you. Some questions your doctor might ask include:
- When did you first notice these symptoms?
- How often do you experience these symptoms?
- How severe are your symptoms?
- Does anything improve your symptoms?
- Does anything make your symptoms worse?
- Have you ever been diagnosed with lichen sclerosus?
- Have you ever had an abnormal Pap test?
- Have you ever been diagnosed with HPV?
Sept. 08, 2022