Overview
Vulvar cancer
Vulvar cancer
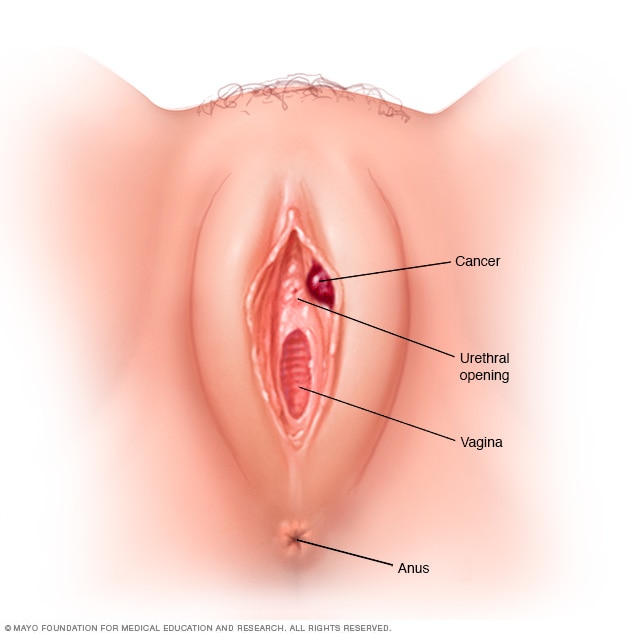
Vulvar cancer is cancer that starts as a growth of cells on the vulva. The vulva is the fleshy area that surrounds the vagina and the tube where urine leaves the body, called the urethra.
Vulvar cancer is cancer that starts as a growth of cells on the vulva. The vulva is the area of skin that surrounds the urethra and vagina. It includes the clitoris and labia.
Vulvar cancer commonly forms as a lump or sore on the vulva that often causes itching. Though it can happen at any age, vulvar cancer is usually diagnosed in older adults.
Vulvar cancer treatment often starts with surgery to remove the cancer and a small amount of surrounding healthy tissue. Sometimes vulvar cancer surgery requires removing the entire vulva. The earlier vulvar cancer is diagnosed, the less likely an extensive surgery is needed for treatment.
Products & Services
Symptoms
Signs and symptoms of vulvar cancer may include:
- A lump, wartlike bump or an open sore on the vulva.
- Bleeding in the genital area that isn't from menstruation.
- Itching of the skin of the vulva that doesn't go away.
- Pain and tenderness that affects the vulva.
- Skin changes, such as changes in the color of the skin of the vulva or thickening of the skin.
When to see a doctor
Make an appointment with a doctor, gynecologist or other healthcare professional if you have any symptoms that worry you.
Causes
It's not always clear what causes vulvar cancer. This cancer starts on the area of skin that surrounds the urethra and vagina. This area of skin is called the vulva.
Vulvar cancer happens when cells in the vulva develop changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells might form a growth called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
Exactly what causes the DNA changes that lead to vulvar cancer isn't always known. Healthcare professionals believe some vulvar cancers are caused by human papillomavirus. Human papilloma virus, also called HPV, is a common virus passed through sexual contact. It's associated with the most common type of vulvar cancer, which is vulvar squamous cell carcinoma.
Types of vulvar cancer
The type of cell in which the cancer begins tells your healthcare team what type of vulvar cancer you have. Knowing your vulvar cancer type helps your healthcare team plan the most effective treatment. Some types of vulvar cancer include:
- Vulvar squamous cell carcinoma. Squamous cell carcinoma of the skin is cancer that starts in cells called squamous cells. Squamous cell carcinoma of the skin happens most often in skin exposed to the sun. But it can happen on any skin, including the skin of the vulva. Most vulvar cancers are squamous cell carcinomas. This type of vulvar cancer is associated with HPV infection.
- Vulvar melanoma. Melanoma is cancer that starts in the pigment-producing cells called melanocytes. Melanoma most often happens on skin that's exposed to the sun. But it can happen anywhere on the skin, including the skin of the vulva.
- Extramammary Paget's disease of the vulva. Extramammary Paget's disease is a cancer that starts near sweat glands in the skin. It most often affects the skin of the vulva. Sometimes it happens at the same time as another kind of cancer. This can include a cancer in the breast, colon, urinary system or female reproductive system.
Risk factors
Factors that increase the risk of vulvar cancer include:
- Older age. The risk of vulvar cancer increases with age, though it can happen at any age. The average age at diagnosis is 65.
- Being exposed to human papillomavirus. Human papillomavirus, also called HPV, is a common virus that's passed through sexual contact. HPV increases the risk of several cancers, including vulvar cancer and cervical cancer. Many young, sexually active people are exposed to HPV. For most the infection goes away on its own. For some, the infection causes cell changes and increases the risk of cancer in the future.
- Smoking tobacco. Smoking tobacco increases the risk of vulvar cancer.
- Having a weakened immune system. If the body's germ-fighting immune system is weakened by medicines or illness, there might be a higher risk of vulvar cancer. People with a weakened immune system include those taking medicines to control the immune system, such as after an organ transplant. Certain medical conditions, such as infection with HIV, can weaken the immune system.
- Having a history of a precancerous condition of the vulva. Vulvar intraepithelial neoplasia is a precancerous condition that increases the risk of vulvar cancer. Most instances of vulvar intraepithelial neoplasia will never develop into cancer. But a small number do go on to become invasive vulvar cancer.
- Having a skin condition involving the vulva. Lichen sclerosus causes the vulvar skin to become thin and itchy. It also increases the risk of vulvar cancer.
Prevention
To lower the risk of vulvar cancer, don't smoke tobacco. Take steps to protect yourself from human papillomavirus infection. Human papillomavirus, also called HPV, is associated with the most common type of vulvar cancer.
Don't use tobacco
Smoking tobacco increases the risk of vulvar cancer. If you don't smoke, don't start. If you smoke, talk with a healthcare professional about things that can help you quit. This might include medicines and counseling.
Lower your risk of HPV infection
HPV is a common virus that's passed through sexual contact. It increases the risk of vulvar cancer. To help reduce the risk of HPV infection:
- Use a condom every time you have sex. Condoms may reduce the risk of contracting HPV but can't fully protect against it.
- Get the HPV vaccine. The vaccine protects against the strains of the virus that are thought to cause vulvar cancer. Talk with a healthcare professional about whether the HPV vaccine is right for you.
Jan. 10, 2025