Overview
Spinal anatomy
Spinal anatomy
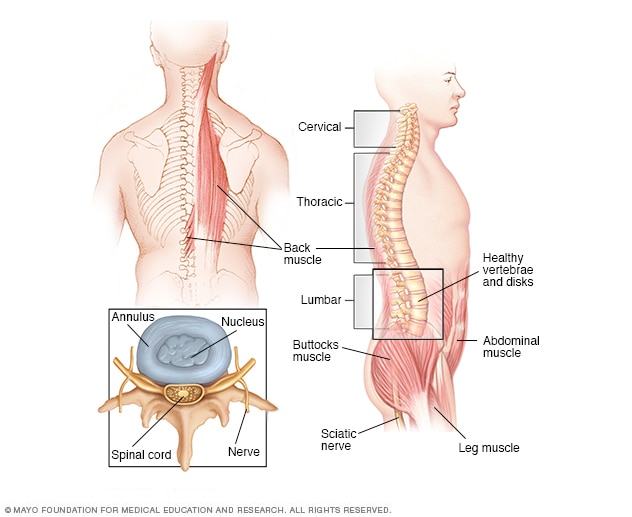
The spinal anatomy of a typical adult
A vertebral tumor is a growth of cells that happens in the bones of the spine. A vertebral tumor also is called a spinal tumor. The bones of the spine are called the vertebrae. The spine is made up of many small vertebrae stacked on top of one another. The vertebrae hold the body upright. They enclose and protect the spinal cord.
Vertebral tumors can be cancerous or not cancerous. A noncancerous vertebral tumor also is called a benign vertebral tumor. Vertebral tumors that are cancerous are called malignant vertebral tumors.
Most malignant vertebral tumors are caused by cancer that starts somewhere else in the body and spreads to the spine. Cancer that spreads from an organ to another part of the body is called metastatic cancer. Cancers that affect the blood cells and bone marrow also can cause malignant vertebral tumors.
Vertebral tumors that start in the bones of the spine and haven't spread from somewhere else are rare. Another name for these tumors is primary bone tumors.
Treatment for vertebral tumors includes surgery, radiation therapy and medicines, including chemotherapy. Small and slow-growing vertebral tumors might not need treatment right away. The treatment that's best for your vertebral tumor depends on your situation. Your healthcare team considers the type of tumor you have, whether it is cancerous and its location within the spine.
Products & Services
Symptoms
Signs and symptoms of vertebral tumors include:
- Back pain in the area of the tumor.
- Back pain that radiates or shoots from the back to a nearby area.
- Back pain that's worse at night.
- Changes in sensation, such as numbness or a feeling of pins and needles.
- Loss of the ability to move part of the body.
- Loss of control over the bladder and bowels.
- Muscle weakness.
When to see a doctor
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you.
Some vertebral tumor symptoms are similar to symptoms caused by other conditions. For example, back pain is very common, and most back pain isn't caused by a tumor. Sometimes it's hard to decide whether to see a healthcare professional when you have back pain.
Make an appointment if:
- The pain is constant and is getting worse.
- The pain doesn't seem to be caused by a certain activity.
- The pain is worse at night.
- You have a history of cancer and the back pain is something new.
Seek immediate medical care if you have back pain along with:
- Muscle weakness in the arms or legs.
- Loss of control of the bowel or bladder.
- Numbness or tingling in the genital area.
Causes
Most vertebral tumors are caused by cancer that starts somewhere else in the body. Cancer that spreads from an organ to somewhere else in the body is called metastatic cancer. Any cancer can spread to the spine. Most vertebral tumors are caused by cancer that spreads from the breasts, lungs or prostate. Other cancers that tend to spread to the spine include kidney cancer and thyroid cancer.
Cancers that affect the blood cells and bone marrow also can cause vertebral tumors. These cancers include multiple myeloma and lymphoma.
Vertebral tumors that start in the spine are rare. It's not clear what causes them.
Vertebral tumors that start in the spine happen when cells in the bones of the spine develop changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In the tumor cells, the DNA changes give different instructions. The changes tell the tumor cells to make many more cells quickly. Tumor cells can keep living when healthy cells would die. This causes too many cells.
Sometimes cells develop changes in their DNA that turn them into cancer cells. Cancer cells can invade and destroy healthy body tissue. They can break away and spread to other parts of the body.
Examples of vertebral tumors that start in the spine and aren't cancerous include:
- Hemangioma.
- Osteoid osteoma.
- Osteoblastoma.
- Aneurysmal bone cyst.
- Osteochondroma.
- Enchondroma.
- Chondroblastoma.
Examples of vertebral tumors that start in the spine and are cancerous include:
- Chondrosarcoma.
- Ewing sarcoma.
- Osteosarcoma.
- Chordoma.
Risk factors
The risk of vertebral tumors is higher in people who have cancer or have been treated for cancer. Most vertebral tumors are caused by cancer that starts somewhere else in the body and spreads to the spine. Cancer that spreads to the spine most often starts in the breasts, lungs or prostate.
Complications
Complications caused by vertebral tumors include:
- Spinal cord compression. Spinal cord compression happens when a tumor grows to press on the spinal cord or nearby nerves. It often causes back pain at first. Later it can cause weakness and numbness in the part of the body controlled by the affected nerves. There may be difficulty walking and a loss of control of the bladder and bowels.
- Spinal instability. Spinal instability can happen if a vertebral tumor weakens the bones in the spine. Bones weakened by tumors can break or go out of alignment. This can make it hard for the spine to hold the body upright. Spinal instability typically causes pain and can lead to weakness.
Treatments may help prevent or treat these complications.
Nov. 21, 2024