Diagnosis
To diagnose a peripheral nerve tumor, your health care provider will ask about your symptoms and medical history. You may undergo a general physical exam and a neurological exam. Several tests may help pinpoint the cause of your symptoms.
- Magnetic resonance imaging (MRI). This scan uses a magnet and radio waves to produce a detailed 3D view of nerves and tissue.
- Computerized tomography (CT). A CT scanner rotates around the body to take a series of images. A computer uses the image to make a detailed view of the peripheral nerve tumor. A CT scan can help your provider determine how the tumor may be affecting you.
- Electromyogram (EMG). For this test, small needles are placed in the muscles. An instrument records the electrical activity in the muscle as they're moved.
- Nerve conduction study. This test is often done with an EMG. It measures how fast the nerves carry electrical signals to the muscles.
- Tumor biopsy. If you have a nerve tumor, you may need a biopsy. A small sample of cells from the tumor is removed and analyzed. Depending on the tumor's size and location, you may need to have medicine that numbs an area of the body, called local anesthesia, or medicine that puts you to sleep, called general anesthesia, during the biopsy. Sometimes a biopsy is the only way to determine whether a tumor is cancerous.
- Nerve biopsy. A biopsy of the nerve may be needed in people who have certain conditions, such as progressive peripheral neuropathy and enlarged nerves that mimic nerve tumors.
Peripheral nerve tumors aren't common. It's important to find a provider who is experienced in diagnosing and treating them. If needed, seek a second opinion.
More Information
Treatment

At Mayo Clinic, your surgeon will talk with you about the procedure beforehand and answer any questions you may have.
Treatment of a peripheral nerve tumor depends on the type of tumor, what nerves and other tissues it affects, and symptoms. Treatment options may include:
Monitoring
Watching and waiting to see if the tumor grows may be an option if it's in a place that makes removal difficult. Or it may be an option if the tumor is small, slow growing, and causes few or no symptoms. You'll have regular checkups and may have MRI scans, CT scans or ultrasounds done every 6 to 12 months to see if the tumor is growing. If repeat scans show that the tumor is stable, then it may be monitored every several years.
Surgery
Schwannoma
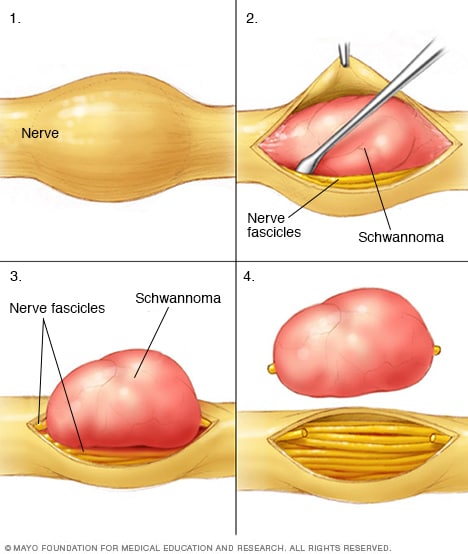
Schwannoma
Surgeons carefully remove schwannomas while taking care to preserve nerve fascicles that aren't affected by the tumors. Nerve fascicles are bundles of nerve fibers.
Some peripheral nerve tumors are removed with surgery. The goal of surgery is to take out the entire tumor without damaging nearby healthy tissue and nerves. When that isn't possible, surgeons remove as much of the tumor as they can.
New methods and tools allow surgeons to reach tumors that are difficult to access. High-powered microscopes used in microsurgery make it easier to tell the difference between a tumor and healthy tissue. And the function of nerves can be monitored during surgery, which helps preserve healthy tissue.
Risks of surgery include nerve damage and disability. These risks are often based on the size of the tumor, where it's located and the approach used for surgery. Some tumors also grow back.
Stereotactic radiosurgery
Gamma Knife stereotactic radiosurgery
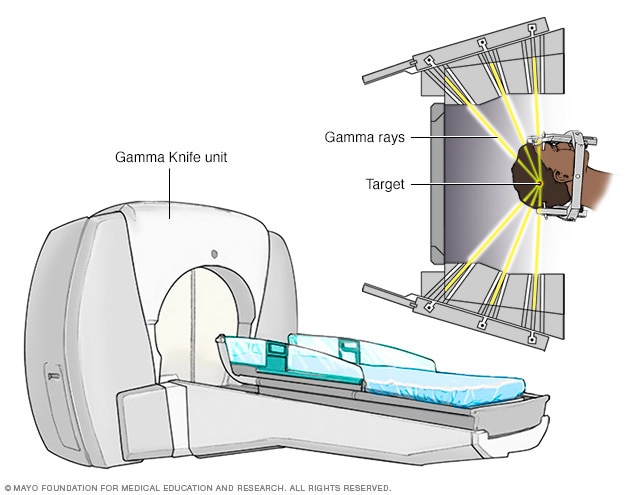
Gamma Knife stereotactic radiosurgery
Stereotactic radiosurgery technology uses many small gamma rays to deliver a precise dose of radiation to the target.
Stereotactic radiosurgery is used to treat some peripheral nerve tumors in or around the brain. Radiation is delivered precisely to a tumor without making an incision. One type of this kind of surgery is called Gamma Knife radiosurgery.
Risks of radiosurgery include weakness or numbness in the treated area. Or the tumor may continue to grow. Very rarely, the radiation could cause cancer in the treated area in the future.
Cancer treatment
Cancerous tumors are treated with standard cancer therapies. These include surgery, chemotherapy and radiation therapy. Early diagnosis and treatment are the most important factors for a good outcome. Tumors may come back after treatment.
Rehabilitation
After surgery, you may need physical rehabilitation. Your health care provider may use a brace or a splint to keep your arm or leg in a position that helps you to heal. Physical therapists and occupational therapists can help you recover function and mobility lost due to nerve damage or limb amputation.
More Information
Coping and support
It can be stressful to deal with the possibility of peripheral nerve tumor complications. Choosing which treatment would be best for you also can be a hard decision. These suggestions may help:
- Learn as much as you can about peripheral nerve tumors. The more you know, the better prepared you'll be to make good choices about treatment. Besides talking to your health care provider, you may want to talk to a counselor or a social worker. Or you may find it helpful to talk to other people who've had a condition like yours. Ask about their experiences during and after treatment.
- Maintain a strong support system. Family and friends can be a source of support. You may find the concern and understanding of other people with a condition like yours especially comforting. Your health care provider or a social worker may be able to put you in touch with a support group.
Preparing for your appointment
If your primary care provider thinks you have a peripheral nerve tumor, you'll be referred to a specialist. Specialists include doctors who are experts in disorders of the nervous system, called neurologists, and doctors trained in brain and nervous system surgery, called neurosurgeons.
What you can do
Before the appointment, you might want to prepare a list of answers to the following questions:
- When did you first notice this problem?
- Has it gotten worse over time?
- Have your parents or siblings ever had similar symptoms?
- Do you have other medical problems?
- What medicines or supplements do you take?
- What surgeries have you had?
What to expect from your doctor
Your doctor may ask some of the following questions:
- Do you have pain? Where is it?
- Do you have any weakness, numbness or tingling?
- Have your symptoms been constant or do they come and go?
- What treatments have you tried for these problems?