Diagnosis
A healthcare professional evaluates your condition based on your symptoms, an exam and tests. You may be referred to a sleep specialist for further evaluation.
The physical exam involves an examination of the back of your throat, mouth and nose. Your neck and waist circumference may be measured. Your blood pressure also may be checked.
A sleep specialist can diagnose and figure out how severe your sleep apnea may be. The specialist also can plan your treatment. The evaluation might involve staying at a sleep center overnight. At the sleep center, your breathing and other body functions are monitored as you sleep. Or you may undergo testing for sleep apnea at home.
Tests
Tests to detect obstructive sleep apnea include:
Polysomnography. During this sleep study, you're hooked up to equipment that monitors your heart, lung and brain activity and breathing patterns while you sleep. The equipment also measures arm and leg movements and blood oxygen levels.
You might be monitored all night or part of the night. If you're monitored for part of the night, it's called a split-night sleep study.
In a split-night sleep study, you'll be monitored during the first half of the night. If you're diagnosed with obstructive sleep apnea, staff members may wake you and give you continuous positive airway pressure therapy for the second half of the night.
The sleep study also can help look for other sleep disorders that can cause excessive daytime sleepiness but have different treatments. The sleep study can uncover leg movements during sleep, known as periodic limb movement disorder. Or the study can help evaluate people who have sudden bouts of sleep during the day, known as narcolepsy.
- Home sleep apnea testing. Under certain circumstances, you may have an at-home version of polysomnography to diagnose obstructive sleep apnea. Home sleep apnea testing kits monitor a limited number of variables to detect breathing pauses during sleep.
Treatment
Effective treatments are available for obstructive sleep apnea. Treatment can improve your sleep and make you feel better during the day. It also may decrease your risk of heart and blood vessel conditions.
Therapies
Continuous positive airway pressure (CPAP)

Continuous positive airway pressure (CPAP)
To eliminate snoring and prevent sleep apnea, a healthcare professional may recommend a device called a continuous positive airway pressure (CPAP) machine. A CPAP machine delivers just enough air pressure to a mask to keep the upper airway passages open, preventing snoring and sleep apnea.
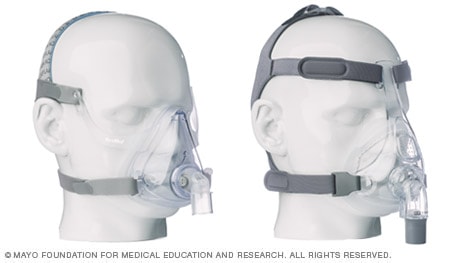
Many CPAP mask options available
Continuous positive airway pressure (CPAP) masks and headgear come in many styles and sizes to comfortably treat your sleep apnea. Everyone has different needs, preferences and face shapes, and sometimes you will need to try different mask styles before you find the one that works the best for you.
Sizes may vary across different mask styles and brands. You may need to try on several styles and sizes to find the best combination of comfort and efficiency.
For example, if you take a small in one type it does not necessarily mean you will need a small in a different brand. Proper sizing is very important to comfort and performance of masks.
Here's a look at a few CPAP mask styles and some possible benefits of each. Work with your doctor and CPAP mask supplier to make sure you have a mask that suits your needs and fits you properly.
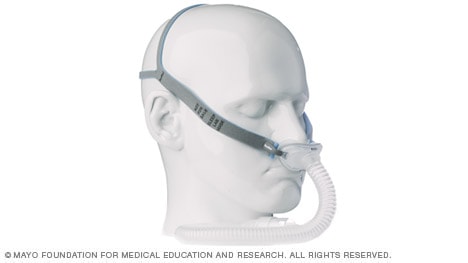
Nasal pillow mask
Nasal pillows fit at the nares to supply air pressure.
Might be good if:
- You feel claustrophobic in masks that cover more of your face
- You want a full field of vision for reading or watching TV
- You want to wear your glasses
- You have facial hair that interferes with other masks
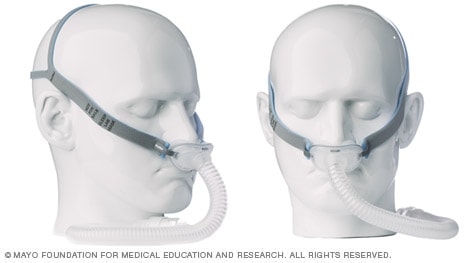
Nasal masks
The mask covering the nose supplies air pressure.
Might be good if:
- Your doctor has prescribed a high air pressure setting
- You move around a lot in your sleep
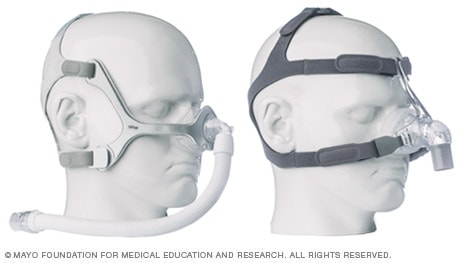
Full-face masks
The mask covering the nose and mouth supplies air pressure.
Might be good if:
- You have nasal obstruction or congestion that makes breathing through your nose difficult
- You breathe through your mouth at night despite a month of trying a nasal mask or nasal pillow interface combined with a heated humidity feature or chin strap or both to keep your mouth closed
Oral device

Oral device
An oral device is placed on the teeth and is designed to keep the throat open by moving the tongue and lower jaw forward.
The therapy most studied and most often recommended for obstructive sleep apnea is positive airway pressure. But other therapies also are available.
Positive airway pressure. If you have obstructive sleep apnea, you may benefit from positive airway pressure. In this treatment, a machine delivers air pressure through a piece that fits into your nose or is placed over your nose and mouth while you sleep.
Positive airway pressure reduces the number of times you stop breathing as you sleep. The therapy also reduces daytime sleepiness and improves your quality of life.
One of the most common types is called continuous positive airway pressure, also known as CPAP (SEE-pap). This treatment delivers continuous and constant pressure that is slightly stronger than the air pressure around you. The air pressure is just enough to keep your upper airway passages open so that you can breathe freely.
Although CPAP effectively treats obstructive sleep apnea, some people find the mask uncomfortable or loud. However, newer machines are smaller and less noisy than older machines. And there are a variety of mask designs for individual comfort.
Also, with some practice, most people learn to adjust the mask to obtain a comfortable and secure fit. You may need to try different types to find one that works well for you. Several options are available, such as nasal masks, nasal pillows or face masks.
If you're having trouble tolerating pressure, some machines have special adaptive pressure functions to improve comfort. You also might benefit from using a humidifier along with your CPAP system.
Another treatment option is autotitrating positive airway pressure, also called APAP. In CPAP, the pressure stays constant. The air pressure of an APAP varies, automatically adjusting when the device senses a change in airway resistance, such as the vibration of a snore. APAP can be helpful when the ideal fixed pressure for CPAP is difficult to identify — as is often the case during home sleep testing when no one is there to monitor your breathing patterns. There is less evidence supporting APAP compared with CPAP, but it seems to offer equivalent results.
Another type of positive airway pressure is bilevel positive airway pressure, also called BPAP. It's less commonly used than CPAP and APAP. BPAP delivers a preset amount of pressure when you breathe in and a different amount of pressure when you breathe out.
If you have stomach discomfort or bloating while using CPAP, check with your healthcare team to see what adjustments you can make to improve its comfort.
In addition, contact your healthcare team if you still snore or remain sleepy during the day despite treatment, if you begin snoring again, or if your weight changes by 10% or more.
Mouth devices. Also known as oral appliances, these are an alternative for some people with mild or moderate obstructive sleep apnea. They're also used for people with severe sleep apnea who can't use CPAP. The devices may reduce sleepiness and improve quality of life.
All these devices are designed to keep the throat open. Some devices keep the airway open by bringing the lower jaw forward, which can sometimes relieve snoring and improve obstructive sleep apnea. Other devices hold the tongue in a different position to keep the airway free.
If you decide to explore this option, see a dentist experienced in dental sleep medicine appliances for the fitting and follow-up therapy. Several devices are available. Close follow-up is needed to ensure successful treatment and that use of the device doesn't cause changes to your teeth.
A newer device uses electrical stimulation on the tongue. A small number of studies show the device may help people with very mild sleep apnea and snoring. This device isn't meant to be used in place of CPAP if you have moderate to severe obstructive sleep apnea. It also is not recommended for people who have a pacemaker or another implanted electrical device.
Surgery or other procedures
Airway stimulation system
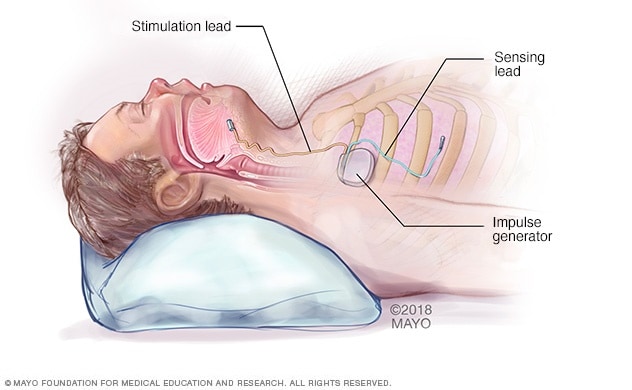
Airway stimulation system
An impulse generator is implanted in the chest and stimulates the nerve that controls tongue movements.
Upper jaw advancement
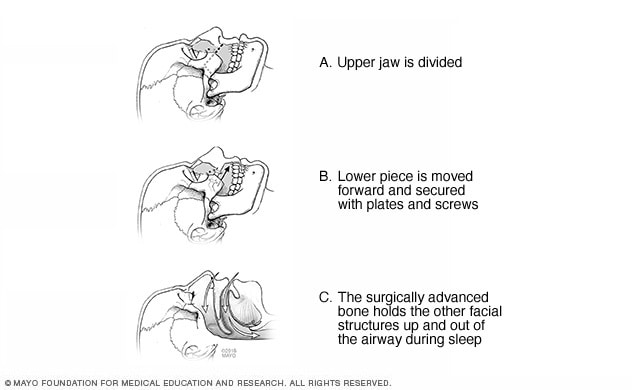
Upper jaw advancement
Upper jaw advancement surgery involves moving the jaw to reduce the risk of obstruction.
Surgery is usually considered only if other therapies haven't been effective or don't fit your lifestyle. Surgical options may include:
- Surgical removal of tissue. Uvulopalatopharyngoplasty, also known as UPPP, is a procedure in which a surgeon removes tissue from the back of the mouth and top of the throat. The tonsils and adenoids may be removed as well. UPPP usually is performed in a hospital and requires a medicine that puts you in a sleeplike state. This medicine is called a general anesthetic. The goal of surgery is to correct any anatomic obstructions so that the upper airway stays open during sleep.
Nerve stimulation implant. This device is approved for use in people with moderate to severe obstructive sleep apnea who can't tolerate CPAP or BPAP.
A small, thin impulse generator, known as a hypoglossal nerve stimulator, is implanted under the skin in the upper chest. When you inhale, the device stimulates the nerve that controls the movement of the tongue. The tongue moves forward instead of moving backward and blocking the throat.
Studies have found that hypoglossal nerve stimulation greatly improves obstructive sleep apnea symptoms and quality of life.
- Jaw surgery. In this procedure, the upper and lower parts of the jaw are moved forward compared with the rest of the facial bones. This enlarges the space behind the tongue and soft palate, making obstruction less likely. This procedure is known as maxillomandibular advancement.
Surgical opening in the neck, known as a tracheostomy. You may need this form of surgery if other treatments have failed and you have life-threatening obstructive sleep apnea.
During a tracheostomy, a surgeon makes an opening in the neck and inserts a metal or plastic tube for breathing. Air passes in and out of the lungs, bypassing the blocked air passage in your throat.
Other types of surgery may help reduce snoring and sleep apnea by clearing or enlarging air passages, including:
- Nasal surgery to remove polyps or straighten a crooked partition between the nostrils, called a deviated septum.
- Surgery to remove enlarged tonsils or adenoids.
- Bariatric surgery to shrink the size of the stomach and help you lose weight. Bariatric surgery can help improve symptoms of obstructive sleep apnea in people with obesity.
Weight-loss medications
Studies show that weight loss medications can help improve symptoms of obstructive sleep apnea. The U.S. Food and Drug Administration recently approved the weight-loss drug tirzepatide (Mounjaro, Zepbound), in combination with diet and exercise, for the treatment of moderate to severe obstructive sleep apnea.
Some people still may need treatment for obstructive sleep apnea after weight loss, although the symptoms are usually milder. Continue to work with your healthcare professional even if you lose a substantial amount of weight so that you're not missing out on any needed treatment.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
In many cases, self-care may be the most appropriate way for you to deal with obstructive sleep apnea. Try these tips:
- Lose weight. If you're overweight or obese, even moderate weight loss may help relieve narrowing of your airway. Losing weight also can improve your health and quality of life and might reduce your daytime sleepiness.
- Exercise. Exercising, such as aerobic exercise and strength training, can help improve your condition. Aim to exercise about 150 minutes a week, and generally try to exercise most days of the week.
- Don't drink alcohol or use certain anti-anxiety medicines or sleeping pills. Alcohol, some anti-anxiety medicines and some sleeping pills can worsen obstructive sleep apnea and sleepiness.
Sleep on your side or stomach rather than on your back. Snoring may be loudest and apneas more common when you sleep on your back. Sleeping on your back can cause your tongue and soft palate to rest against the back of your throat and block your airway.
Devices that vibrate when you try to sleep on your back may help. These devices are usually worn around your neck or chest. Ask your healthcare professional if such a device might be appropriate for you. You also might try sewing a tennis ball in the back of your pajama top or place pillows behind you to keep you sleeping on your side.
- Keep your nasal passages open while you sleep. If you have congestion, use a saline nasal spray to help keep your nasal passages open. Talk to a member of your healthcare team about using nasal decongestants or antihistamines, because some medicines may be recommended for only short-term use.
Preparing for your appointment
If you suspect that you have obstructive sleep apnea, you'll likely first see your primary doctor or other healthcare professional. You might be referred to a sleep specialist.
Here's some information to help you get ready for your appointment.
What you can do
Be aware of pre-appointment requests. When you make your appointment, ask if there's anything you need to do in advance, such as keeping a sleep diary.
In a sleep diary, you record your sleep patterns such as bedtime, number of hours slept, nighttime awakenings and awake time. You also can record your daily routine, naps and how you feel during the day.
- Write down your symptoms, including any that may seem unrelated to the reason for your appointment, and when they began.
- Write down key personal information, including new or ongoing health concerns, major stresses, or recent life changes.
- Bring a list of all medicines, vitamins or supplements you take, including doses. Include anything you've taken to help you sleep.
- Take your bed partner along, if possible. Your partner can provide information about how much and how well you're sleeping. If you can't bring your partner with you, ask about how well you sleep and whether you snore and then share this information at your appointment.
- Write down your questions. Preparing a list of questions can help you make the most of your time during your appointment.
For obstructive sleep apnea, some basic questions to ask include:
- What's the most likely cause of my symptoms?
- What tests do I need? Do I need to go to a sleep clinic?
- What treatments are available and which do you recommend for me?
- I have other health conditions. How can I best manage these conditions together?
Don't hesitate to ask other questions.
What to expect from your doctor
A key part of the evaluation of obstructive sleep apnea is a detailed history, meaning your healthcare professional likely will ask you many questions. These may include:
- When did you first notice symptoms?
- Have your symptoms been off and on, or do you always have them?
- Do you snore? If so, does your snoring disrupt anyone else's sleep?
- Do you snore in all sleep positions or just when sleeping on your back?
- Do you ever snore, snort, gasp or choke yourself awake?
- Has anyone seen you stop breathing during sleep?
- How refreshed do you feel when you wake up? Are you tired during the day?
- Do you have a headache or dry mouth when you awaken?
- Do you doze off or have trouble staying awake while sitting quietly or driving?
- Do you nap during the day?
- Do you have family members with sleep disorders?
What you can do in the meantime
- Try to sleep on your side. Most forms of obstructive sleep apnea are milder when you sleep on your side.
- Don't drink alcohol close to bedtime. Alcohol makes obstructive sleep apnea worse.
- If you're drowsy, don't drive. If you have obstructive sleep apnea, daytime sleepiness can put you at higher risk of motor vehicle accidents. To be safe, schedule rest breaks. If a close friend or family member tells you that you appear sleepier than you feel, don't drive.
Dec. 04, 2025