Overview
Adrenal glands
Adrenal glands
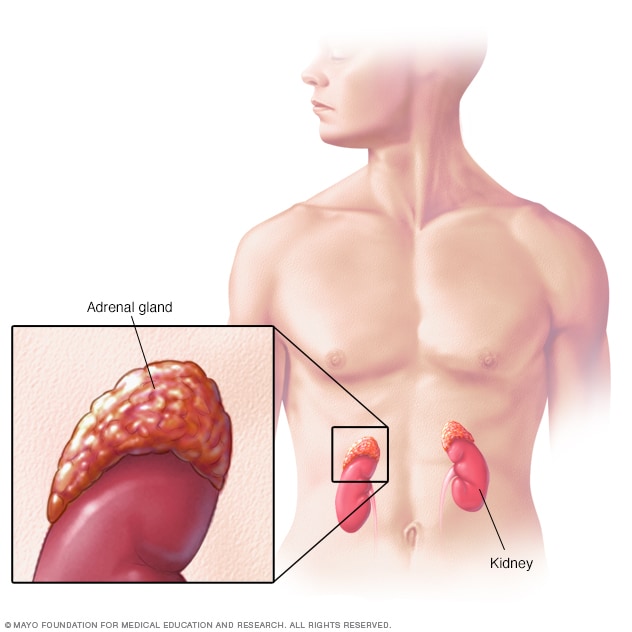
Located on top of the kidneys, the adrenal glands make hormones that help regulate metabolism, the immune system, blood pressure and other important functions. Although small, these glands control much of what happens in the body.
Neuroblastoma is a cancer that starts in cells called neuroblasts. Neuroblasts are immature nerve cells. They are found in several areas of the body.
Neuroblastoma most often starts in the neuroblasts in the adrenal glands. The adrenal glands are located on top of each kidney. The glands make hormones that control important functions in the body. Other cancers and tumors can happen in the adrenal glands, such as pheochromocytomas. These are different from neuroblastomas but may cause similar symptoms.
Neuroblastoma can happen in other parts of the body that have neuroblasts, such as in the spine, belly, chest and neck. It also can affect other places in the body if it spreads. When the cancer spreads, it's called metastatic neuroblastoma.
Neuroblastoma mostly affects children age 5 or younger. Symptoms vary, depending on where it occurs in the body.
Some forms of neuroblastoma may go away on their own. Other forms of neuroblastoma need treatment. Treatments include surgery, chemotherapy, radiation therapy and bone marrow transplant. Your child's healthcare team will select the neuroblastoma treatments that are best for your child.
Neuroblastoma is different from other cancers that have similar names, such as glioblastoma and nephroblastoma, also called Wilms tumor. All of these names contain the term "blastoma," which means a cancer or tumor that's made up of blasts. Blasts are cells that haven't fully developed yet. Neuroblastoma starts in nerve cells that are in the blast stage, called neuroblasts.
Products & Services
Symptoms
Signs and symptoms of neuroblastoma may vary depending on what part of the body is affected. This cancer starts in immature nerve cells called neuroblasts. Neuroblasts are found in several areas of the body.
When the cancer is only in the place where it starts, called localized neuroblastoma, it doesn't always cause symptoms. Symptoms are more likely to occur when the cancer grows to involve nearby areas, called regional neuroblastoma, or spreads to distant parts of the body, called metastatic neuroblastoma.
Neuroblastoma in the adrenal glands and belly may cause symptoms such as:
- Belly pain.
- A lump under the skin that typically isn't tender when touched.
- Diarrhea or constipation.
Neuroblastoma in the chest and neck may cause symptoms such as:
- Wheezing.
- Difficulty breathing.
- Changes to the eyes, including drooping eyelids and pupils that are different sizes.
Neuroblastoma near the spine may cause symptoms such as:
- Back pain.
- Trouble urinating or passing a bowel movement.
- Weakness in the legs.
Metastatic neuroblastoma may cause symptoms such as:
- Bone pain, which might cause young children to limp when walking.
- Dark, bruiselike circles around the eyes, which are said to look like racoon eyes.
- Fever.
- Fussiness.
- Lumps of tissue under the skin that typically don't hurt.
- Not growing or gaining weight as expected.
When to see a doctor
Contact your child's healthcare professional if your child has any symptoms that worry you. Mention any changes in your child's behavior, habits or appearance.
Causes
It's not clear what causes neuroblastoma. This cancer starts in immature nerve cells called neuroblasts. Neuroblasts are found in several areas of the body.
Neuroblastoma starts when neuroblasts develop changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to grow and multiply quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells might form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
Risk factors
Risk factors for neuroblastoma include:
- Young age. The risk of neuroblastoma is higher in children. This cancer happens mostly in children age 5 and younger.
- Genetic syndromes. Some DNA changes that run in families can raise the risk of neuroblastoma. Genetic syndromes thought to raise the risk include Turner syndrome, Costello syndrome and familial neuroblastoma. Yet, healthcare professionals think only a small number of neuroblastomas are inherited.
There are no known ways to prevent neuroblastoma.
Complications
Complications of neuroblastoma may include:
- Spread of the cancer. With time, the cancer cells may spread to other parts of the body. When it spreads, it's called metastatic neuroblastoma. Neuroblastoma most often spreads to the lymph nodes, bone marrow, liver, skin and bones.
- Pressure on the spinal cord. A neuroblastoma may grow and press on the spinal cord, causing spinal cord compression. Spinal cord compression may cause pain and paralysis.
- Symptoms caused by cancer secretions. Neuroblastoma cells may secrete chemicals that irritate other tissues. The irritated tissues can cause symptoms called paraneoplastic syndromes. Symptoms of paraneoplastic syndromes may include rapid eye movements and difficulty with coordination. Other symptoms include abdominal swelling and diarrhea.
Sept. 30, 2025