Overview
Cushing syndrome
Cushing syndrome
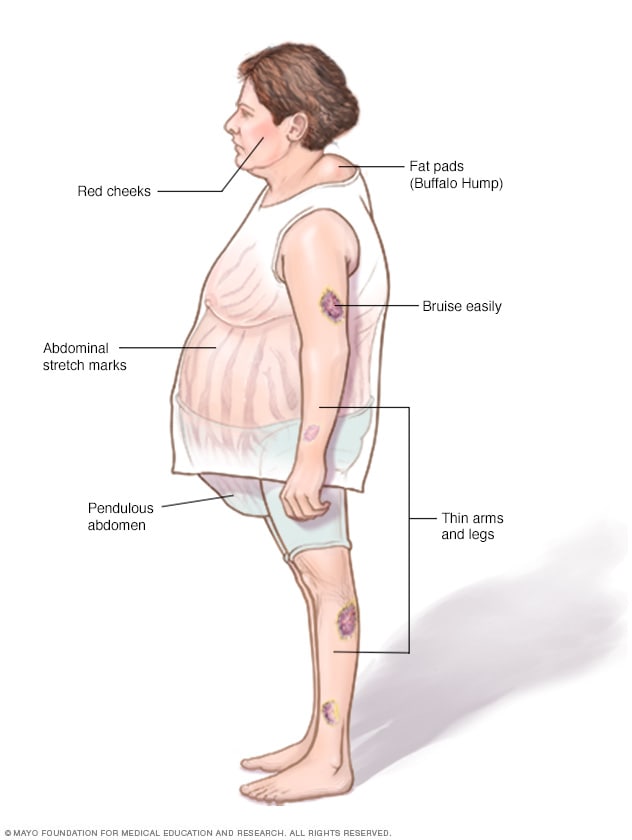
Without treatment, Cushing syndrome can cause facial roundness, weight gain around the middle body and upper back, thinning of the arms and legs, easy bruising, and stretch marks.
Cushing syndrome happens when the body has too much of the hormone cortisol for a long time. This can result from the body making too much cortisol, or from taking medicines called glucocorticoids, which affect the body the same way as cortisol.
Too much cortisol can cause some of the main symptoms of Cushing syndrome — a fatty hump between the shoulders, a rounded face, and pink or purple stretch marks on the skin. Cushing syndrome also can cause high blood pressure or bone loss. Sometimes, it can cause type 2 diabetes.
Treatments for Cushing syndrome can lower the body's cortisol levels and improve symptoms. The sooner treatment starts, the better the chances for recovery.
Products & Services
Symptoms
Symptoms of Cushing syndrome can vary depending on the level of extra cortisol.
Common symptoms of Cushing syndrome
- Weight gain in the trunk, with thin arms and legs.
- Weight gain in the face. This is sometimes called moon face.
- A fatty lump between the shoulders. This may be referred to as a buffalo hump.
- Pink or purple stretch marks on the stomach, hips, thighs, breasts and underarms.
- Thin, frail skin that bruises easily.
- Slow wound healing.
- Acne.
Symptoms women with Cushing syndrome may experience
- Thick, dark hair on the face and body. This condition is called hirsutism.
- Periods that are irregular or that stop.
Symptoms men with Cushing syndrome may experience
- Lower sex drive.
- Reduced fertility.
- Problems getting an erection.
Other possible symptoms of Cushing syndrome
- Extreme tiredness.
- Muscle weakness.
- Depression, anxiety and irritability.
- Emotions that are hard to control.
- Trouble concentrating or remembering.
- Sleeplessness.
- High blood pressure.
- Headache.
- Infections.
- Skin darkening.
- Bone loss, which can lead to broken bones.
- Stunted growth in children.
When to see a doctor
Call your health care provider if you have symptoms of Cushing syndrome, especially if you're taking glucocorticoid medicine to treat a health issue such as asthma, arthritis or inflammatory bowel disease.
Causes
Adrenal gland endocrine system
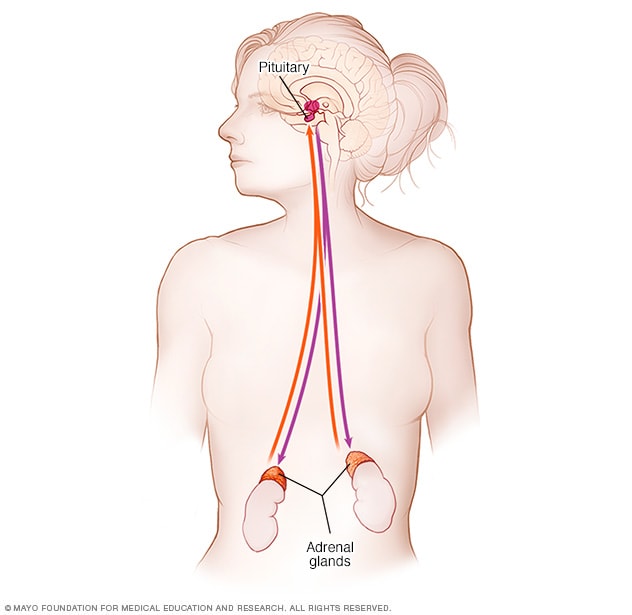
Adrenal gland endocrine system
The adrenal gland endocrine system includes the adrenal glands and pituitary gland. Signals from the pituitary gland tell the adrenal glands to make cortisol. The pituitary gland knows if the body has the right amount of cortisol.
Cushing syndrome is caused by having too much cortisol in the body. Cortisol is a hormone that is made in the adrenal glands. It helps the body respond to stress and plays many other important roles, including:
- Controlling blood pressure.
- Reducing inflammation.
- Helping the heart and blood vessels work correctly.
- Controlling blood sugar.
- Helping the body use food for energy.
The role of glucocorticoid medicines (exogenous Cushing syndrome)
Cushing syndrome can happen from taking glucocorticoid medicines. These are often used to treat inflammatory diseases such as rheumatoid arthritis, lupus and asthma. Pain or injury in the back or joints and many skin rashes may be treated with glucocorticoids. They also may be used to stop the body from rejecting a new organ after a transplant.
Glucocorticoids may be taken by mouth, given as a shot, rubbed into the skin or breathed into the lungs by an inhaler. Any form of glucocorticoid, if taken in large amounts for a long time, can cause Cushing syndrome.
When the body makes too much cortisol (endogenous Cushing syndrome)
A hormone made in the pituitary gland controls how much cortisol the body makes. This is called adrenocorticotropic hormone (ACTH). Some tumors make ACTH, which creates more cortisol and can cause Cushing syndrome. Problems with the adrenal glands also can affect cortisol and cause Cushing syndrome.
When Cushing syndrome happens this way, it may be caused by:
- ACTH-producing pituitary adenoma. Pituitary adenomas are tumors that grow in the pituitary gland. They are found at the base of the brain and are usually not cancer. These tumors sometimes make too much ACTH. This causes the adrenal glands to make extra cortisol. When Cushing syndrome happens this way, it's called Cushing disease. It happens more often in women and is the most common type of endogenous Cushing syndrome.
- Ectopic ACTH-producing tumor. Rarely, a tumor that makes too much ACTH grows in an organ that usually doesn't make ACTH. This is called ectopic ACTH production. It causes the body to make too much cortisol. These tumors can be cancerous, but aren't always. They are usually found in the lungs, pancreas, thyroid or thymus gland.
-
Adrenal gland tumors or disease. Problems with the adrenal glands can cause them to make too much cortisol. The most common is a tumor in the outer part of the adrenal gland called an adrenal adenoma. These tumors are not cancer, and only some make too much cortisol.
Cancerous tumors in the outer part of the adrenal glands, known as adrenocortical carcinoma, are rare. But they can make cortisol and cause Cushing syndrome. Sometimes, several lumps that make cortisol can grow in the adrenal glands and cause Cushing syndrome. This is called adrenal nodular hyperplasia.
- Familial Cushing syndrome. Rarely, people inherit a tendency to get tumors on one or more of their endocrine glands, which are glands that make hormones. If these tumors make ACTH or cortisol, Cushing syndrome can happen.
Complications
Without treatment, Cushing syndrome can cause complications, including:
- Bone loss, also called osteoporosis, which can lead to broken bones.
- High blood pressure, also called hypertension.
- Type 2 diabetes.
- Serious or multiple infections.
- Loss of muscle mass and strength.