Diagnosis and tests
To diagnose chordoma, a healthcare professional might do a physical exam and ask questions about your health history. Other tests and procedures might include imaging tests and taking a sample of tissue for lab testing.
Imaging tests, such as a CT scan or MRI
Imaging tests make pictures of the body. They can show the size and location of a cancer. CT scans are best for seeing bone changes. MRI scans are better for showing tumors and the tissues around them.
- CT scans. CT scans are good at showing bone changes, such as holes or weak spots. On a CT scan, chordomas usually look like light or dark spots with damaged bone around them. A CT scan also can show if the tumor has spread, such as near the skull and neck bones. Sometimes, a special dye called contrast medium is used for a CT scan. The dye appears bright on images. So it makes certain areas that are being scanned show up better.
- MRI scans. MRI scans are better at showing tumors and the blood vessels around them. MRI scans can show if the tumor has different sections and how it's affecting the tissues around the spine. Chordomas usually appear as bright spots with darker areas inside them.
Biopsy
A biopsy is a procedure to remove a sample of tissue for testing in a lab. A biopsy is essential to confirm whether what's seen on imaging is chordoma. That's because in imaging scans, chordoma can look like other conditions that need different treatments. For chordoma, the sample of tissue might be collected by:
- Inserting a needle through the skin. During a needle biopsy, a healthcare professional inserts a thin needle through the skin and guides it into the cancer. The health professional uses the needle to collect small samples of tissue. Biopsy before surgery may not be possible for some chordomas, such as those in the skull base.
- Taking out a sample during surgery. During surgical biopsy, a surgeon makes a cut, also called an incision, in the skin to access the cancer. The surgeon takes out a piece of cancer for testing.
Deciding how the biopsy should be done requires careful planning by your healthcare team. Your care team needs to do the biopsy in a way that allows for future surgery to take out the cancer. For this reason, it's a good idea to seek care at a medical center that sees many people with chordoma.
To confirm it's chordoma, your healthcare team looks for pathology signs of chordoma. These can include:
- Cells that look bubbly inside, called physaliphorous cells.
- A special protein called brachyury that's common in chordoma cells.
- Other proteins, such as S100, vimentin and pancytokeratins.
Genetic testing
Genetic tests are not a routine part of chordoma diagnosis. But sometimes genetic tests are suggested for families with a history of chordoma or for children and young adults with chordoma.
Treatment
Chordoma treatment depends on the size and location of the cancer, as well as whether it has invaded nerves or other tissue.
- Surgery is often the first step and an important chordoma treatment. If a tumor can be taken out fully, it offers the best chance at a cure.
- Radiation therapy usually follows surgery, to kill any cancer cells that might remain. Sometimes radiation therapy is used before surgery to make a tumor smaller and easier to take out. Sometimes radiation therapy might be used by itself, if it's not possible to take out the tumor through surgery.
- Targeted therapy medicines may be used for cancer that's spread in the body, called metastases, or for cancer that returns after initial treatment, called a recurrence.
In some cases, chordoma can be cured. But chordomas can be difficult to treat. It's hard to take them out fully because they grow so near the brain and spine. And they resist conventional radiation and chemotherapy. Often, chordomas return. This is called a recurrence. When that happens, treatment can help control or manage the cancer over time instead of cure it.
Surgery
Endoscopic skull base surgery
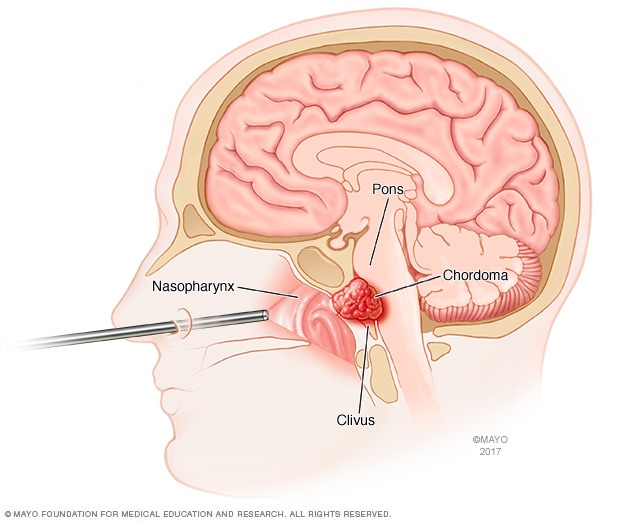
Endoscopic skull base surgery
Endoscopic skull base surgery uses a long, thin tube called an endoscope to access the base of the skull. The endoscope goes through the nose. A surgeon puts tools through the endoscope to do the surgery. This illustration shows an endoscope going through the nose to treat a chordoma, which is a type of bone cancer that often happens at the base of the skull.
In chordoma surgery, surgeons aim to take out as much of the tumor as possible in one piece. When done in the mobile spine or sacrum, this is called en bloc resection. When a chordoma can be taken out fully in one piece, the procedure lowers the chance of cancer cells spreading and the cancer coming back.
But it can be difficult to take out the whole chordoma. This is because chordomas grow around important structures, including the brain, spinal cord, nerves and blood vessels. Surgeons try to remove the cancer without damaging healthy structures. It's also challenging to safely reach parts of the skull base.
When a chordoma can't be taken out completely, surgeons try to take out as much as possible.
Types of surgery may differ depending on where the tumor is located:
- Skull base chordoma surgery. Sometimes surgeons can go through the nose to get to a skull base chordoma. This kind of surgery is called endoscopic skull base surgery. It uses a long, thin tube called an endoscope. The endoscope is inserted through the nose to access the cancer. Special tools can be passed through the endoscope to take out the cancer. Sometimes a traditional open surgery is needed. During open surgery, a surgeon uses surgical instruments inserted through a large cut, also called an incision, at the back of the head or neck. Other approaches also may be used.
- Mobile spine and sacral chordoma surgery. The goal of chordoma surgery in areas of the spine below the skull base is to take out as much of the tumor as possible. Other surrounding bone and tissues also may be taken out. If the tumor is in the sacrum, at the bottom of the spine, the whole sacrum may be taken out. This is called a sacrectomy. This surgery may be done through an incision in the belly or in the back.
Rarely, surgeons might suggest another surgery to stabilize the area where the cancer once was.
Complications of chordoma surgery include risks of any surgery, such as infection, blood clots and bleeding. Complications also can happen if nerves are damaged during surgery. Possible complications include:
- Double vision.
- Bowel or bladder changes.
- Loss of sexual function.
- Numbness or loss of feeling.
- Trouble walking or sitting.
- Leaking of the fluid that surrounds the brain and spinal cord, called cerebrospinal fluid.
Radiation
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, photons, protons or other sources.
During radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body.
In the past, chordomas have resisted standard radiation that needed to be given at a dose low enough not to damage any nearby spinal cord or brain tissue. Newer radiation treatments may help by delivering a higher dose of radiation more directly to the tumor while protecting the surrounding brain, spinal cord and nerves. Examples of radiation options include:
The type of radiation therapy used can vary depending on where the cancer is located and what options the surgical center has.
Side effects of radiation therapy may include:
- Tiredness.
- Skin swelling, irritation or other changes.
- Headache.
- Hormone changes, such as hypopituitarism.
- Brain changes or damage.
- Hearing and vision changes.
- Trouble swallowing.
There's also a slight risk that radiation therapy might cause a different cancer later on. This is called a secondary cancer.
Targeted therapy medicines
Chordoma usually does not shrink with standard chemotherapy. But targeted therapy for cancer is a treatment that uses medicines to attack specific chemicals in cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die.
Targeted therapy is sometimes used as part of a clinical trial. Or it's used off-label to treat chordoma that spreads to other areas of the body, called metastatic chordoma. Off-label means the drug has been approved by the Food and Drug Administration to treat a different condition. Targeted therapy also may be used to treat chordoma that comes back after treatment, called a recurrence.
Some examples of targeted therapy that might be used first for chordoma include:
- Imatinib.
- Dasatinib.
- Sunitinib.
Sometimes, other drugs might be used. These could include:
- Imatinib given with a chemotherapy drug or with sirolimus.
- Erlotinib.
- Lapatinib
- Sorafenib.
Side effects of targeted therapy may include:
- Tiredness.
- Upset stomach.
- Rash.
- Diarrhea.
- Swelling.
- Thyroid and kidney changes.
Treatments being studied
Scientists continue to research possible new treatments for chordoma. Some of those include:
- Checkpoint inhibitors. These are a type of drug that helps the immune system find and attack cancer cells.
- Brachyury-targeted therapies. Chordomas almost always make brachyury protein. So vaccines and new drugs that target brachyury are being tested.
More Information
Coping and support
With time, you'll find what helps you cope with the uncertainty and worry of a cancer diagnosis. Until then, you may find it helps to:
Learn enough about chordomas to make decisions about your care
Ask your healthcare team about your cancer, including your test results, treatment options and, if you want, your prognosis. As you learn more about your chordoma, you may become more confident in making treatment decisions.
In addition, assistive devices and equipment may help with some mobility concerns. And if you have cancer pain, some treatments are available. Your options may depend on what's causing your cancer pain and the intensity of the pain you're feeling.
Keep friends, family or community close
Friends, family or community resources can help provide the practical support you may need. For example, this might include taking care of your home if you're in the hospital.
Find someone to talk with
Find someone who is willing to listen to you talk about your hopes and worries. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your healthcare team about support groups in your area. Other sources of information include the National Cancer Institute, the American Cancer Society, the Chordoma Foundation and the Mayo Clinic Connect online sarcoma support group. The Chordoma Foundation also offers a directory of chordoma specialists.
Preparing for your appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you. If your healthcare professional thinks you might have a chordoma, you may be referred to a specialist.
Because appointments can be brief, it's a good idea to be prepared. Here's some information to help you get ready.
What you can do
- Be aware of anything you need to do ahead of time. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you have, including any that may not seem related to the reason for which you scheduled the appointment.
- Write down important personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins and supplements you're taking and the doses.
- Take a family member or friend along. It can be hard to remember all the information provided during an appointment. Someone who goes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Your time with your healthcare team is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For chordoma, some basic questions to ask include:
- Do I have a chordoma?
- What is the stage of my chordoma?
- Has my chordoma spread to other parts of my body?
- Will I need more tests?
- What are the treatment options?
- How much does each treatment increase my chances of a cure or prolong my life?
- What are the potential side effects of each treatment?
- How will each treatment affect my daily life?
- Is there one treatment option you believe is the best?
- What would you recommend to a friend or family member in my situation?
- Should I see a specialist?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
- What will determine whether I should plan for a follow-up visit?
Don't hesitate to ask other questions.
What to expect from your doctor
Be prepared to answer questions, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
Oct. 17, 2025