Overview
Carotid artery
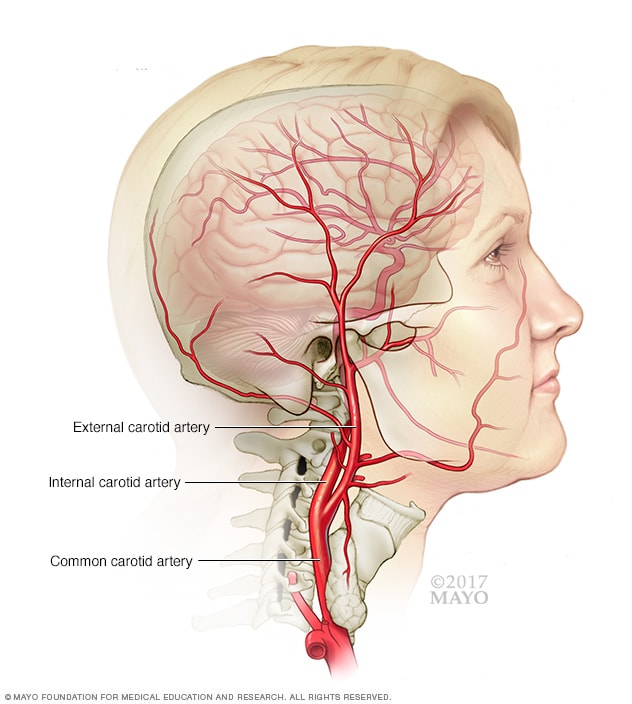
Carotid artery
The carotid arteries are a pair of blood vessels. There's one on each side of the neck. The carotid arteries deliver blood to the brain and head.
Carotid artery disease occurs when fatty deposits, called plaques, clog the blood vessels that deliver blood to the brain and head (carotid arteries). The clog increases the risk of stroke. Stroke is a medical emergency that occurs when the brain loses all or much of its blood supply.
During a stroke, the brain doesn't get oxygen and brain cells begin to die within minutes. Stroke is a leading cause of death and disability in the U.S.
Carotid artery disease often develops slowly. The first sign of the condition might be a stroke or transient ischemic attack (TIA). A TIA is a temporary shortage of blood flow to the brain.
Treatment of carotid artery disease usually involves lifestyle changes, medicines and sometimes surgery.
Symptoms
In its early stages, carotid artery disease often doesn't have symptoms. The condition might not be obvious until it's serious enough to deprive the brain of blood, causing a stroke or TIA.
Symptoms of a stroke or TIA include:
- Sudden numbness or weakness in the face or limbs, often on one side of the body.
- Sudden trouble speaking and understanding speech.
- Sudden trouble seeing in one or both eyes.
- Sudden dizziness or loss of balance.
- Sudden, severe headache with no known cause.
When to see a doctor
Seek emergency care for any symptoms of a stroke. Even if they last only a short while and then you feel OK, see a health care provider right away. You might have had a TIA. A TIA puts you at risk of a stroke.
Talk to your health care provider if you have risk factors for carotid artery disease even if you don't have symptoms. Managing the risk factors might protect you from a stroke. Seeing a provider early increases your chances of finding carotid artery disease and getting treatment before a stroke occurs.
Causes
A buildup of fatty deposits, known as plaques, in the arteries that send blood to the brain cause carotid artery disease. Plaques are clumps that include cholesterol, fat and blood cells that form in the artery. This process is called atherosclerosis.
Carotid arteries that are clogged with plaques narrow. A clog in carotid arteries makes it hard for oxygen and nutrients to reach the brain.
Risk factors
Factors that increase the risk of carotid artery disease include:
- High blood pressure. Too much pressure on artery walls can weaken them and make them easier to damage.
- Tobacco use. Nicotine can irritate the inner lining of the arteries. Smoking also increases heart rate and blood pressure.
- Diabetes. Diabetes lowers the ability to process fats, creating a greater risk of high blood pressure and atherosclerosis.
- High blood-fat levels. High levels of low-density lipoprotein cholesterol and high levels of triglycerides, a blood fat, help the buildup of plaques.
- Family history. The risk of carotid artery disease is higher if a relative has atherosclerosis or coronary artery disease.
- Age. Arteries become less flexible and more likely to be injured with age.
- Obesity. Excess weight increases the chances of high blood pressure, atherosclerosis and diabetes.
- Sleep apnea. Spells of stopping breathing at night might increase the risk of stroke.
- Lack of exercise. Not exercising leads to conditions that can damage the arteries, including high blood pressure, diabetes and obesity.
Complications
Ischemic stroke
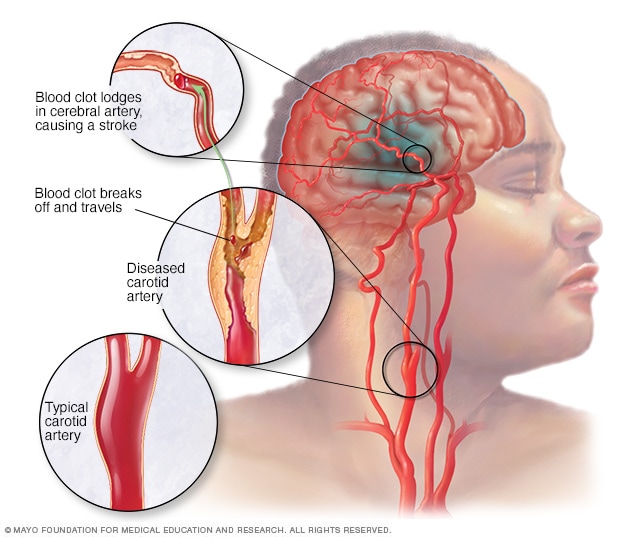
Ischemic stroke
An ischemic stroke occurs when a blood clot, known as a thrombus, blocks or plugs an artery leading to the brain. A blood clot often forms in arteries damaged by a buildup of plaques, known as atherosclerosis. It can occur in the carotid artery of the neck as well as other arteries.
Carotid artery disease causes about 10% to 15% of strokes. A stroke is a medical emergency that can cause brain damage, muscle weakness and possibly death.
Carotid artery disease can lead to stroke through:
- Reduced blood flow. A carotid artery might get so narrow because of atherosclerosis that not enough blood reaches parts of the brain.
- Ruptured plaques. A piece of a plaque can break off and travel to smaller arteries in the brain. The piece of plaque can get stuck in one of these smaller arteries. This blockage cuts off blood supply to part of the brain.
- Blood clot blockage. Some plaques are prone to cracking and forming irregular surfaces on the artery wall. The body reacts as it does to an injury. It sends blood cells that help the clotting process to the area. The result can be a large clot that blocks or slows blood flow to the brain, causing a stroke.
Prevention
These steps can help prevent carotid artery disease or keep it from getting worse:
- Don't smoke. Within a few years of quitting, a former smoker's risk of stroke is like a nonsmoker's.
- Maintain a healthy weight. Being overweight increases other risk factors, such as high blood pressure, cardiovascular disease, diabetes and sleep apnea.
- Eat a healthy diet. Focus on fruits and vegetables, whole grains and fish, nuts and legumes. Limit cholesterol and fat, especially saturated and trans fats.
- Limit salt. Too much salt can increase blood pressure in some people. Experts recommend that healthy adults eat less than 1,500 milligrams of salt a day.
- Exercise regularly. Exercise can lower blood pressure, increase high-density lipoprotein (HDL) cholesterol, the "good" cholesterol — and improve the overall health of your blood vessels and heart. It also helps you lose weight, control diabetes and reduce stress.
- Limit or avoid alcohol. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Control illnesses. Managing conditions such as diabetes and high blood pressure helps protect arteries.