Overview
Bradycardia
Bradycardia
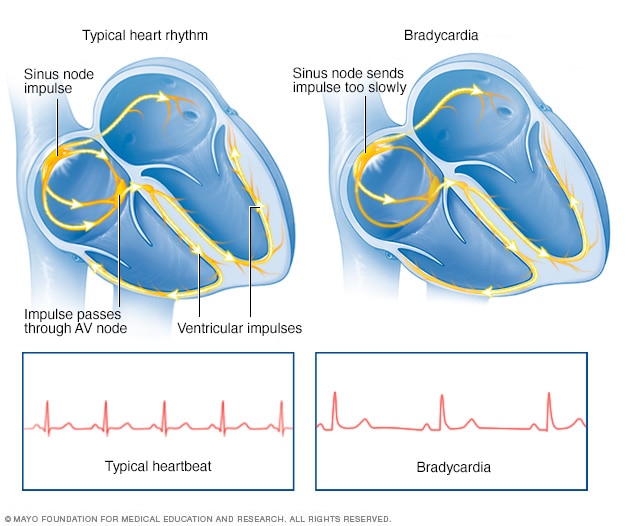
Bradycardia, shown on the right, is a slower than typical heart rhythm that often starts in the area of the heart called the sinus node. A typical heart rhythm is shown in the image on the left.
Bradycardia (brad-e-KAHR-dee-uh) is a slow heart rate. The hearts of adults at rest usually beat between 60 and 100 times a minute. If you have bradycardia, your heart beats fewer than 60 times a minute.
Bradycardia can be a serious problem if the heart rate is very slow and the heart can't pump enough oxygen-rich blood to the body. If this happens, you may feel dizzy, very tired or weak, and short of breath. Sometimes bradycardia doesn't cause symptoms or complications.
A slow heart rate isn't always a concern. For example, a resting heart rate between 40 and 60 beats a minute is common in some people, particularly healthy young adults and trained athletes. It also is quite common during sleep.
If bradycardia is severe, a pacemaker may be needed to help the heart beat at an appropriate rate.
Symptoms
A slower than typical heartbeat is called bradycardia. If the slow heartbeat stops the brain and other organs from getting enough oxygen, symptoms may include:
- Chest pain.
- Confusion or memory problems.
- Dizziness or lightheadedness.
- Feeling very tired, especially during physical activity.
- Fainting or near-fainting.
- Shortness of breath.
When to see a doctor
Many things can cause symptoms of bradycardia. It's important to get a fast, accurate diagnosis and appropriate care. Make an appointment for a health checkup if you are worried about a slow heart rate.
If you faint, have difficulty breathing or have chest pain lasting more than a few minutes, call 911 or emergency medical services.
Causes
Typical heartbeat
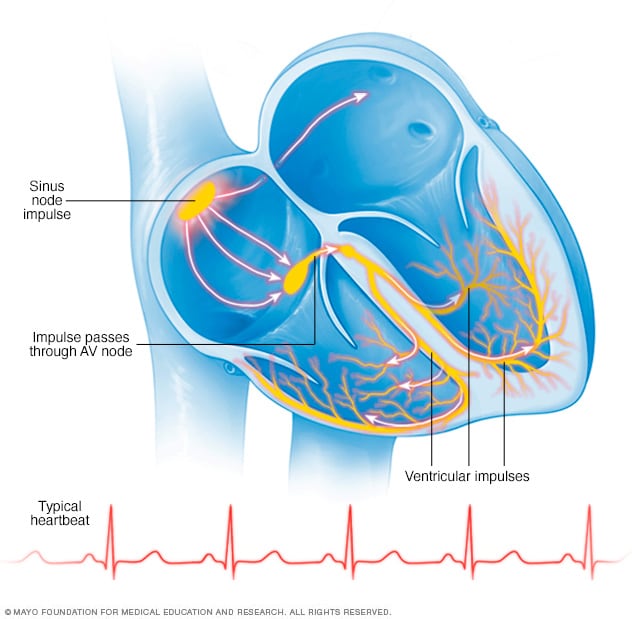
Typical heartbeat
In a typical heart rhythm, a tiny cluster of cells at the sinus node sends out an electrical signal. The signal then travels through the atria to the atrioventricular (AV) node and then passes into the ventricles, causing them to contract and pump out blood.
Bradycardia can be caused by:
- Heart tissue damage related to aging.
- Damage to heart tissues from heart disease or heart attack.
- A heart condition that you're born with, called a congenital heart defect.
- Inflammation of heart tissue, called myocarditis.
- A complication of heart surgery.
- An underactive thyroid gland, called hypothyroidism.
- Changes in the level of body minerals such as potassium or calcium.
- A sleep disorder called obstructive sleep apnea.
- Inflammatory disease, such as rheumatic fever or lupus.
- Certain medicines, including sedatives, opioids, and some used to treat heart and mental health conditions.
To better understand the causes of bradycardia, it may help to know how the heart typically beats. The typical heart has four chambers.
- The two upper chambers are called the atria.
- The two lower chambers are called the ventricles.
Within the heart's upper right chamber is a group of cells called the sinus node. The sinus node is the heart's natural pacemaker. It creates the signal that starts each heartbeat. Bradycardia happens when these signals slow down or are blocked.
Things that cause changes in heart signaling that can lead to bradycardia include:
- Bradycardia-tachycardia syndrome. In some people, problems in the sinus node at the top of the heart cause alternating slow and fast heart rates.
- Heart block, also called atrioventricular block. In this condition, the heart's electrical signals don't move correctly from the upper chambers to the lower chambers.
Risk factors
Bradycardia is often associated with damage to heart tissue from some type of heart disease. Anything that increases the risk of heart problems can increase the risk of bradycardia. Risk factors include:
- Older age.
- High blood pressure.
- Smoking.
- Heavy alcohol use.
- Illegal drug use.
- Stress and anxiety.
Complications
Possible complications of bradycardia include:
- Frequent fainting.
- Heart failure.
- Sudden cardiac arrest or sudden cardiac death.
Prevention
Preventing heart disease may help lower the risk of bradycardia.
The American Heart Association recommends these steps:
- Get regular exercise. Ask your healthcare team about how much and what type of exercise is best for you.
- Eat nutritious foods. Eat a healthy diet that's low in salt and solid fats and rich in fruits, vegetables and whole grains.
- Keep a healthy weight. Being overweight increases the risk of heart disease. Talk with your care team to set realistic goals for body mass index (BMI) and weight.
- Control blood pressure and cholesterol. High blood pressure and high cholesterol increase the risk of heart disease. Make lifestyle changes and take medicines as directed to manage high blood pressure or high cholesterol.
- Don't smoke or use tobacco. If you smoke and can't quit on your own, talk to a healthcare professional about methods or programs to help.
- Limit or do not drink alcohol. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Manage stress. Intense emotions may affect the heart rate. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to reduce and manage stress.
- Get good sleep. Poor sleep may increase the risk of heart disease and other chronic conditions. Adults should aim to get 7 to 9 hours of sleep daily. Go to bed and wake at the same time every day, including on weekends. If you have trouble sleeping, talk to a healthcare professional about strategies that might help.
It's important to have regular health checkups. If you already have heart disease, take these steps to lower your risk of irregular heartbeats:
- Follow your treatment plan. Be sure you understand your treatment. Take all medicines as directed by your healthcare team.
- Tell your care team if your symptoms change. Also tell the healthcare team if you have new symptoms.
Dec. 13, 2024