诊断
垂体瘤通常不易发现或检出。在许多情况下,这是因为分泌激素的垂体瘤(称为功能性腺瘤)和较大肿瘤(称为大腺瘤)所引起的症状与其他医疗状况相似。还因为垂体瘤生长十分缓慢。不分泌激素的小垂体瘤(称为无功能性微腺瘤)通常不会引起症状。这类垂体瘤通常是在因其他原因而进行的影像学检查(如 MRI 或 CT)中发现。
检测和诊断垂体瘤时,医务人员可能询问个人和家族病史,并进行体格检查。用于检测垂体瘤的检查还可能包括:
-
血液检测。血液检测可显示体内某些激素的含量是否过高或过低。对于一些激素,如果血液检测结果显示其含量过高,医务人员就足以诊断垂体腺瘤。
对于其他激素(如皮质醇),如果血液检测结果显示其含量过高,可能还需要进行其他检测。这些检测可以揭示此前的结果是由垂体腺瘤还是其他健康问题所引起。
在检测结果显示激素水平过低的情况下,需要进行其他检查(通常是影像学检查),以确定这些检测结果是否由垂体腺瘤所致。
- 尿液检测。尿液检测可帮助诊断分泌过多 ACTH 激素的垂体腺瘤。ACTH 过多会使体内皮质醇含量增加,从而导致库欣病。
- MRI 扫描。磁共振成像(MRI)扫描利用磁场和计算机生成的无线电波生成人体器官和组织的详细图像。脑部 MRI 有助于检测垂体瘤,并显示其位置和大小。
- CT 扫描。计算机断层成像扫描(CT 扫描)是一种结合一系列 X 线来生成横截面图像的影像学检查。要检测和诊断垂体瘤,MRI 扫描比 CT 扫描更常用。但在医务人员认为必须切除垂体瘤的情况下,CT 扫描可能有助于进行手术规划。
- 视力检查。垂体瘤可能影响视力,尤其是侧面视力(外周视力)。视力检查可以确认您的视力状况,有助于医务人员确定是否需要进行其他检测垂体瘤的检查。
医务人员可能将您转诊给激素紊乱专科医生(内分泌科医生),以进行更多检查。
Pituitary tumor versus craniopharyngioma
Both pituitary tumors and craniopharyngiomas grow near the pituitary and can cause similar symptoms such as headaches and vision changes. And they both can affect hormones. These similarities can make it easy to confuse them, but they are not the same.
A pituitary adenoma begins in the pituitary's hormone-making cells. The adenoma may produce extra hormone. Many pituitary adenomas are treated with endoscopic surgery. Some types are treated with medicines.
A craniopharyngioma grows from leftover embryonic tissue near the pituitary stalk. This type of tumor often contains cysts. A craniopharyngioma does not make hormones, but it may change typical hormone function. Treatment for craniopharyngioma usually involves surgery and radiation. MRI and CT scans may be used to help tell them apart.
To check for a pituitary tumor, your healthcare professional will likely talk with you about your personal and family medical history and do a physical exam. Testing to detect a pituitary tumor also may include:
-
Blood tests. Blood tests can show whether your body has too much or too little of certain hormones. In some cases, a high hormone level may be enough for your healthcare professional to diagnose a pituitary tumor.
For other hormones, such as cortisol, more tests may be needed to confirm whether the high level is caused by a pituitary tumor or by another condition.
Results that show hormone levels are too low need to be followed with other tests, usually imaging exams, to see if a pituitary adenoma may be the cause of those test results.
- Urine tests. A urine test can help check for a type of pituitary adenoma that makes too much of the hormone ACTH. Too much ACTH leads to too much cortisol in the body and causes Cushing disease.
- Brain MRI scan. A magnetic resonance imaging scan, also called an MRI scan, takes detailed images of the body's organs and tissues. A brain MRI can help detect a pituitary tumor and show its location and size. During an MRI, a small amount of contrast is injected into a vein. The contrast travels in your blood and helps certain tissues show up more clearly.
- Brain CT scan. A computerized tomography scan, also called a CT scan, combines multiple X-rays to create cross-sectional images. CT scans are not used as often as MRI scans for finding pituitary tumors. However, a CT scan may be helpful when planning surgery.
- Vision testing. Some pituitary tumors can affect your eyesight, especially your ability to see to the side. An eye exam can help check for this.
What does a pituitary tumor look like on MRI?
On a pituitary MRI, a small tumor called a microadenoma often shows up as a tiny spot. The tumor and the rest of the gland take up the contrast material differently. So right after the contrast is given, this tiny tumor spot usually looks a little darker on the images. A larger tumor, known as a macroadenoma, can make the pituitary gland look bigger and can push aside parts of the gland. It also may press on nearby areas, such as the nerves that help you see.
How can you see a pituitary tumor on MRI?
MRI scans take very detailed pictures of the brain using thin slices. A healthcare professional takes pictures before and after giving the contrast to help see the tumor. For very small tumors, a fast type of scan takes several pictures very quickly right after the contrast is injected. Microadenomas absorb the contrast more slowly, so they look darker than the rest of the gland right after the contrast is given.
Bigger tumors usually are easy to spot. The MRI shows how close the tumors are to the nerves that help you see and to nearby blood vessels. Seeing the tumor's location on MRI is necessary for surgical planning and for protecting your vision and overall health during treatment.
Blood tests for pituitary adenoma: What do they check?
Blood, urine and saliva tests look for two things:
- Extra hormone made by the tumor. Common tests look at prolactin, insulin-like growth factor-1 (IGF-1) for growth hormone, and thyroid tests such as TSH and free T4. Cortisol and ACTH tests measure how well the pituitary and adrenal glands make and control cortisol, a hormone linked to stress and metabolism.
- Low levels of pituitary hormones. Blood tests can check levels of cortisol, free T4 and TSH, sex hormones such as testosterone or estradiol with luteinizing hormone (LH) and follicle-stimulating hormone, and IGF-1 to look for hormone deficiencies that may need treatment.
Your healthcare professional may refer you to a specialist in hormone disorders, called an endocrinologist, for more testing.
治疗
多数垂体腺瘤无需治疗。它们不是癌症,所以如果不引起症状,只需长期观察。如果需要治疗,具体的治疗方法取决于肿瘤类型、大小、位置和随时间推移的生长情况。如果肿瘤导致体内某些激素过多或过少,也会影响到治疗。您的年龄和整体健康状况也是治疗计划需要考虑的因素。
治疗目标是:
- 使激素水平恢复到健康范围。
- 避免对垂体腺造成更多损害,使其恢复正常功能。
- 逆转由肿瘤压力引起的症状或防止其恶化。
如果垂体腺瘤需要治疗,治疗方法可能包括手术切除肿瘤。药物或放射疗法也可用于治疗垂体腺瘤。垂体腺瘤由医疗专家团队进行治疗。团队成员可能包括:
- 脑外科医生,也称为神经外科医生。
- 鼻窦外科医生,也称为 ENT 外科医生。
- 激素紊乱专科医生,也称为内分泌科医生。
- 放射治疗专家,也称为放射肿瘤科医生。
Can a pituitary tumor shrink on its own?
It's uncommon. Tumors called microprolactinomas have been observed to shrink or even go away on their own in rare cases. Prolactin-secreting tumors much more often shrink with medicine.
手术
治疗垂体瘤的手术涉及移除肿瘤。有时也称为肿瘤切除。如果垂体腺瘤符合以下情况,外科医生可能建议进行手术:
- 压迫视神经并影响视力。
- 导致头痛或面痛等其他症状。
- 由于垂体腺受压,导致体内激素水平降低。
- 导致体内部分激素分泌过多。
术后结果通常取决于腺瘤的类型、大小和位置,以及肿瘤是否已扩散到周围组织。
切除垂体瘤的手术包括内镜经鼻蝶手术和开颅术。
What size pituitary tumor should be removed?
There isn't a rule for the exact size that requires removal. Surgery usually is recommended when the tumor:
- Presses on the optic nerves or affects vision.
- Causes the body to make too much of certain hormones.
- Pushes on your pituitary gland and lowers your hormone levels.
- Continues to grow after treatment.
- Bleeds and causes symptoms.
- Causes other symptoms, such as headache or facial pain.
Larger tumors are more likely to press on nearby structures. To decide whether surgery is the best treatment, healthcare teams consider a combination of factors. These factors include symptoms, hormone tests, growth and scan findings — not just size.
Results after surgery typically depend on the adenoma type, its size and location, and whether the tumor has grown into tissues around it.
Surgeries to remove a pituitary tumor include transnasal transsphenoidal surgery and craniotomy.
内镜经鼻蝶手术
内镜经鼻蝶手术
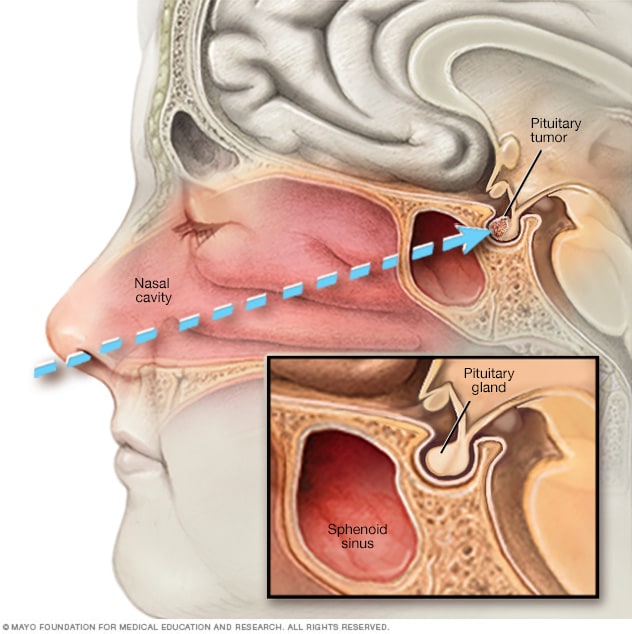
内镜经鼻蝶手术
在内镜经鼻蝶手术中,医生会将一种手术器械通过鼻孔沿着鼻中隔放入垂体瘤处。
这种手术又称腺瘤切除术,是切除垂体腺瘤最常用的手术。
在手术过程中,外科医生,通常是神经外科医生与鼻和鼻窦外科医生合作,通过鼻和鼻窦切除腺瘤。这种手术不需要在身体外部做任何切口,不会影响大脑的其他部位,不会造成明显的疤痕。
巨型大腺瘤可能很难通过这种手术切除,尤其是大腺瘤已经扩散到周围神经、血管或大脑的其他部位时。
经颅手术
这种手术也称为颅骨切开术。在垂体瘤的治疗中,这种手术的使用频率低于内镜经鼻蝶手术。在这项手术中,外科医生不仅能更容易地触及和切除尺寸较大的大腺瘤或者扩散到附近神经或脑组织的垂体瘤,还能更容易地看清肿瘤的范围以及肿瘤周围的脑部组织。在经颅手术过程中,外科医生会在头皮上做一个切口,经由颅骨上部切除肿瘤。
内镜经鼻蝶手术和经颅手术一般比较安全。并发症并不常见。但和所有手术一样,这两种手术也存在风险。垂体瘤手术的并发症可能包括:
- 出血。
- 感染。
- 对麻醉药物(使您在术中进入类似睡眠状态的药物)的反应。
- 短暂性头痛和鼻塞。
- 脑损伤。
- 复视或视力丧失。
- 垂体损伤。
What is the survival rate for pituitary tumor surgery?
Prognosis and success rate depends on tumor type, size, where it extends, and the experience of the team performing the surgery. Many people with small, hormone-secreting tumors go into hormone remission after surgery. For Cushing disease, about 70% to 90% of people achieve remission when they have surgery in an experienced surgical center.
Vision often improves after surgery to remove a tumor that was pressing on the nerves that help you see. About 70% to 90% of people with vision issues see improvement. But full recovery is less likely if the nerves were compressed for a long time. Some tumors, especially larger or invasive ones, need medicines or focused radiation after surgery. Sometimes both medicines and radiation are needed.
放射疗法
放射疗法使用高能放射源来治疗垂体瘤。放射疗法可以在术后进行,或者如果不选择手术时,可以单独进行。
对于以下情况的垂体瘤,放射疗法可能会有所帮助:
- 不能通过手术完全切除。
- 术后复发。
- 导致药物无法缓解的症状。
垂体腺瘤放射疗法的目标是控制腺瘤生长或阻止腺瘤分泌激素。
可用于治疗垂体瘤的放射疗法包括:
- 立体定向放射外科治疗。这种放射疗法通常以单次高剂量方式精确地将辐射束集中在肿瘤上。虽然名字中有“外科”这个词,但不需要切开皮肤,而是借助脑成像技术,根据肿瘤大小和形状将射束投照到肿瘤上。因此这种疗法需要在颅骨上连接一个头部支架。治疗后会立即移除支架。几乎没有辐射会接触肿瘤周围健康组织,减少对健康组织的损伤。
- 外部光束放射治疗(分割放射治疗)。该疗法在一段时间内,以少量多次的方式输送辐射。一个疗程通常需要持续 4 到 6 周,每周 5 次。
- 调强放射治疗。这类放疗简称 IMRT,使用一台计算机调节辐射束形状,从多个角度包围肿瘤。辐射束的强度可能受到限制,这样可以降低对健康组织产生副作用的风险。
- 质子束疗法。另一种放射疗法是质子束疗法,它使用带正电荷的离子(质子)靶向肿瘤,质子束会在肿瘤内释放能量后停止运动。也就是说,可以控制质子束靶向垂体腺瘤,减少对健康组织针对副作用的风险。这种类型的放射疗法需要特殊设备,尚未广泛使用。
垂体腺瘤放射疗法的潜在副作用和并发症包括:
- 垂体损伤会限制其分泌激素的能力。
- 垂体周围的健康组织损伤。
- 视神经受损引起的视力变化。
- 垂体周围的其他神经损伤。
- 患脑肿瘤的风险略有增加。
放射肿瘤科医生会评估您的状况,并与您讨论放射疗法对您病情的益处和风险。这种放射疗法的最大益处通常需要数月到数年才能显现出来。放射疗法的副作用和并发症通常也不会立马显现出来。请务必要长期坚持定期随访护理,以检测放射疗法可能引起的激素问题。
药物
药物治疗可能有助于管理垂体腺瘤。药物可能有助于降低身体因肿瘤产生的激素量。一些药物还可能缩小某些类型的垂体瘤。
分泌催乳素的垂体瘤
以下药物用于减少垂体腺瘤分泌的催乳素。它们通常也可以缩小肿瘤。
- 卡麦角林。
- 溴隐亭(Parlodel、Cycloset)。
可能的副作用包括:
有些人在服用这些药物期间会产生强迫行为,例如赌博问题。这类行为又称为冲动控制障碍。
分泌促肾上腺皮质激素的垂体瘤
制造促肾上腺皮质激素的肿瘤,也称为 ACTH,会使身体产生过多皮质醇。这种状况称为库欣病。以下药物有助于减少身体产生的皮质醇量:
- 酮康唑。
- 美替拉酮(Metopirone)。
- 奥唑司他(Isturisa)。
这些药物的潜在副作用包括可能导致严重心跳不规则的心脏问题。
另一种叫做米非司酮(Korlym、Mifeprex)的药物可用于治疗伴有 2 型糖尿病或葡萄糖不耐症的库欣病患者。米非司酮并不能减少身体产生的皮质醇量,而是阻止皮质醇对身体组织的影响。
米非司酮的副作用包括:
药物帕瑞肽(Signifor)通过减少垂体腺瘤产生的 ACTH 发挥作用。这是一种注射药物,每天注射两次。手术切除腺瘤无效时,医务人员通常会建议使用帕瑞肽。无法通过手术切除腺瘤时,也可使用这种药物。
可能的副作用包括:
生长激素型垂体瘤
两种药物可以治疗生长激素型垂体瘤。当手术切除垂体腺瘤未能使体内生长激素恢复到健康水平时,医务人员通常会开具这些药物。
垂体激素替代治疗
垂体控制着人体的生长、甲状腺功能、肾上腺功能、生殖功能和体内水分平衡。由于垂体可引起激素水平变化,因此垂体腺瘤或其手术治疗或放射治疗可能会损害上述部分或全部功能。如果您的激素水平下降到异常水平,您可能需要接受激素替代治疗,使激素水平恢复正常水平。
等待观察
在观察等待期,也称为观察期、期待疗法或延迟疗法,您可能需要接受定期复诊检查,确定肿瘤是否增长或激素水平是否变化。如果腺瘤没有引起任何症状或引发其他健康问题,或许可以选择观察等待。请向医务人员咨询就您的情况而言观察等待与治疗的益处和风险。
临床试验
探索 Mayo Clinic 的研究 测试新的治疗、干预与检查方法,旨在预防、检测、治疗或控制这种疾病。
妥善处理与支持
您在垂体瘤诊治过程中有问题要问是一件很自然的事。该过程可能让人崩溃,有时让人恐惧万分。这就是尽可能多地了解自己的病情很重要的原因。您对治疗了解得越多越好。
您可能会发现与跟自己有着相同处境的人分享您的感受会有所帮助。查看您所在地区是否有垂体瘤患者的互助小组。医院经常赞助这些互助小组。医务人员或许可以帮助您找到您所需的情感支持。
准备您的预约
您可能需要先去看初级保健医生。如果医生认为您可能患有垂体瘤,接下来可能需要与专科医生约诊。这些专科医生可能包括鼻和鼻窦外科医生、脑外科医生(神经外科医生)或内分泌科医生(专门治疗激素分泌紊乱的医生)。
以下信息可以帮助您做好就诊准备。
您能做些什么
请在约诊时询问是否需要提前进行任何准备,例如在某项检查前禁食。请列出以下内容:
- 您的症状,包括可能看似与您的约诊原因无关的任何症状。
- 关键的个人信息,包括重大压力、近期的生活变化和家族病史。
- 您服用的药物、维生素或补充剂,包括剂量。
- 要向医务人员咨询的问题。
尽可能让家人或朋友陪同您就诊,以帮助您记住所获得的信息。
对于垂体瘤,可向医务人员咨询的问题包括:
- 我的症状或状况可能是由于什么造成的?
- 还有其他可能的原因吗?
- 我应该看什么专科医生?
- 我需要做哪些检查?
- 最佳治疗方案是什么?
- 除了您建议的治疗方法,还有什么替代方案?
- 我还有其他健康状况。如何同时进行管理?
- 我需要遵守哪些注意事项?
- 有没有可以供我参考的手册或其他印刷材料?您推荐哪些网站?
如果还有其他问题,请随时提出。
医生可能做些什么
医务人员可能会向您询问一些问题,包括:
- 您何时开始出现症状?
- 症状是持续存在还是偶尔出现?
- 您的症状有多严重?
- 有没有什么情况似乎会改善您的症状?
- 有没有什么情况似乎会加重您的症状?
- 您以前有没有因为任何原因做过头部影像学检查?
Dec. 23, 2025