Overview
Labor induction means getting the uterus to contract before labor begins on its own. It's sometimes used for a vaginal birth.
The main reason to induce labor is concern for the health of the baby or the health of the pregnant person. If a healthcare professional suggests labor induction, it's most often because the benefits are greater than the risks. If you're pregnant, knowing why and how labor induction is done can help you prepare.
Products & Services
Why it's done
To decide if you need labor induction, a healthcare professional looks at several factors. These include your health. They also include the baby's health, gestational age, weight estimate, size and position in the uterus. Reasons to induce labor include:
- Diabetes. This can be diabetes that came on during pregnancy, called gestational diabetes, or diabetes that was present before pregnancy. If you use medicine for your diabetes, delivery is suggested by 39 weeks. Sometimes delivery may be earlier if diabetes is not well controlled.
- High blood pressure.
- A medical condition such as kidney disease, heart disease or obesity.
- An infection in the uterus.
Other reasons for labor induction include:
- Labor that hasn't started on its own one or two weeks after the due date. At 42 weeks from the day of the last period, this is called a postterm pregnancy.
- Labor that doesn't begin after the water breaks. This is called premature rupture of membranes.
- Problems with the baby, such as poor growth. This is called fetal growth restriction.
- Too little amniotic fluid around the baby. This is called oligohydramnios.
- Problems with the placenta, such as the placenta peeling away from the inner wall of the uterus before delivery. This is called placental abruption.
Asking for labor induction when there isn't a medical need is called elective induction. People who live far from a hospital or a birthing center might want this type of induction. So might those who have a history of fast deliveries. For them, scheduling an elective induction might help avoid giving birth without medical help.
Before an elective induction, a healthcare professional makes sure that the baby's gestational age is at least 39 weeks or older. This lowers the risk of health problems for the baby.
People with low-risk pregnancies may choose labor induction at 39 to 40 weeks. Research shows that inducing labor during this time lowers several risks. Risks include having a stillbirth, having a large baby and getting high blood pressure during pregnancy. It's important that you and your healthcare professional share in the decision to induce labor at 39 to 40 weeks.
Risks
Uterine incisions used during C-section
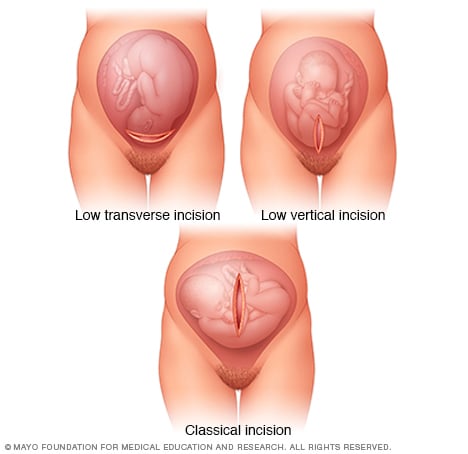
Uterine incisions used during C-section
A C-section includes two surgical cuts, called incisions. After the first cut through the skin, a cut is made through the wall of the uterus. The images above show how the cut through the uterus might be made. Low transverse incisions, shown at the top left, are the most common.
Labor induction carries risks, including:
- Failed induction. An induction might fail if proper ways to induce don't result in a vaginal delivery after 24 or more hours. Then a C-section might be needed.
- Low fetal heart rate. Medicines used to induce labor might cause too many contractions or contractions that are out of the ordinary. This can lessen the baby's oxygen supply and lower or change the baby's heart rate.
- Infection. Some methods of labor induction, such as rupturing the membranes, might increase the risk of infection for both you and your baby.
- Uterine rupture. This is a rare but serious complication. The uterus tears along the scar line from an earlier C-section or major surgery on the uterus. If uterine rupture happens, an emergency C-section is needed to prevent life-threatening complications. The uterus might need to be removed. That procedure is called a hysterectomy.
- Bleeding after delivery. Labor induction raises the risk that the uterine muscles won't contract the way they should after giving birth. This condition, called uterine atony, can lead to serious bleeding after a baby is born.
Labor induction isn't for everyone. It might not be an option if:
- You've had a C-section with a vertical cut, called a classic incision, or major surgery on your uterus.
- The placenta is blocking the cervix, called placenta previa.
- The umbilical cord drops into the vagina ahead of the baby, called umbilical cord prolapse.
- Your baby is lying buttocks first, called breech, or is lying sideways.
- You have an active genital herpes infection.
How you prepare
Labor induction most often is done in a hospital or birthing center. That's because both you and the baby can be watched there. And you have access to labor and delivery services.
What you can expect
During the procedure
There are a number of ways to induce labor. The healthcare team might use one of the following ways or a mix of them to help start labor. During and after these procedures, a member of your care team watches your contractions and the baby's heart rate.
Your healthcare professional might:
-
Ripen the cervix. The cervix most often begins to soften before delivery. This is called ripening. It also thins and opens. But sometimes the cervix isn't ready for induction. Prostaglandins, versions of chemicals the body makes, might be placed inside the vagina or taken by mouth. This helps ripen the cervix.
Or a small tube, called a catheter, with a balloon on the end is put into the cervix. Filling the balloon with saline and resting it against the inside of the cervix can help the cervix ripen.
- Sweep the membranes of the amniotic sac. With sweeping the membranes, also called stripping them, a healthcare professional sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall.
-
Rupture the amniotic sac. With this technique, also known as an amniotomy, a healthcare professional makes a small opening in the amniotic sac. The hole causes the water to break.
An amniotomy is done only if the cervix is partially opened, called dilated, and thinned, and the baby's head is deep in the pelvis.
- Put a medicine into a vein. In the hospital, a healthcare professional might inject oxytocin (Pitocin), a hormone that causes the uterus to contract. Oxytocin is not as good at cervical ripening as it is at speeding up labor that has already begun.
How long it takes for labor to start depends on how ripe the cervix is when the induction starts, how labor is induced and how the body responds. It can take minutes to several hours.
After the procedure
Most often, labor induction leads to a vaginal birth. A failed induction, one in which the procedure doesn't lead to a vaginal birth, might lead to another induction or a C-section.