Jan. 08, 2019
Idiopathic subglottic stenosis (ISS) refers to narrowing of the upper trachea of unknown cause. The disease is rare, with an estimated incidence of 1 per 400,000 person-years. ISS accounts for approximately 19 percent of patients with laryngotracheal stenosis, with the majority having an identifiable cause such as an iatrogenic injury, neck or throat trauma, or an inflammatory connective tissue disease. The exact pathogenesis of ISS is unknown, but disordered inflammation, aberrant immune response to infection and gastroesophageal reflux are thought to play a role.
Patients with ISS are nearly universally women, and most are premenopausal. The most common presenting symptoms are progressive dyspnea and dysphonia; patients also can have stridor, cough or difficult-to-expectorate sputum.
Flow-volume loop of a patient with ISS
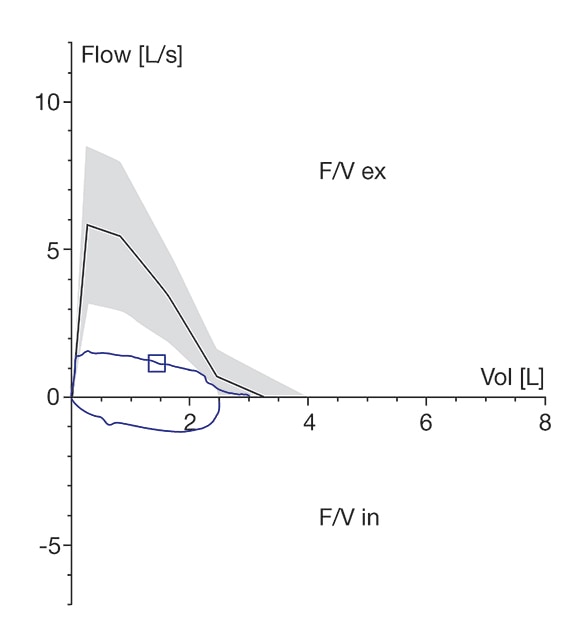
Flow-volume loop of a patient with ISS
Flattening of the inspiratory and expiratory limb of the flow-volume loop (blue) of a patient with idiopathic subglottic stenosis (ISS). The expected control is shown in black.
Rhinolaryngoscopy showing ISS
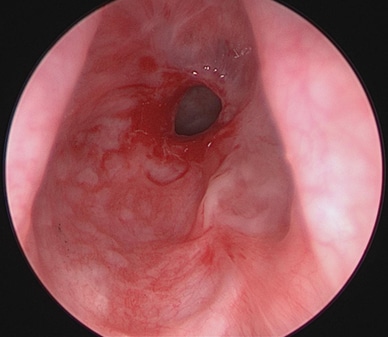
Rhinolaryngoscopy showing ISS
Rhinolaryngoscopy of a 56-year-old woman with idiopathic subglottic stenosis (ISS). Note the fibroinflammatory stenosis just below the vocal folds.
Pulmonary function testing can show obstruction, reduced peak expiratory flow, reduced maximum voluntary ventilation, or flattening of both the inspiratory and expiratory limb of the flow-volume curve.
Radiographic imaging is not necessary for the diagnosis of ISS, but when available it can show narrowing of the subglottic trachea in the anteroposterior or lateral dimension. Endoscopy, such as rhinolaryngoscopy or bronchoscopy, can definitively diagnose subglottic stenosis by demonstrating narrowing of the subglottic airway lumen. ISS lesions have varying degrees of inflammation, fibrosis, and web or stricture formation.
In addition to characterizing a patient's pulmonary function and visualizing the upper trachea, diagnostic workup for ISS includes an assessment for a secondary cause of airway stenosis, such as a history of trauma, difficult intubation, inhaled injuries, neck radiation or evidence of a connective tissue disease. The laboratory analysis should include urinalysis and testing for anti-neutrophil cytoplasmic antibodies (ANCAs) found in granulomatosis with polyangiitis, an important secondary cause of laryngotracheal stenosis.
Many patients with ISS are initially thought to have obstructive small-airways disease on the basis of their symptoms and are treated unsuccessfully with bronchodilators and inhaled or systemic glucocorticoids. At Mayo Clinic, once the subglottic airway is found to be stenotic, the treatment strategy has been a standardized combination of surgical intervention to improve airway patency and medical therapy to slow the rate of recurrence.
Postoperative appearance of the same stenosis
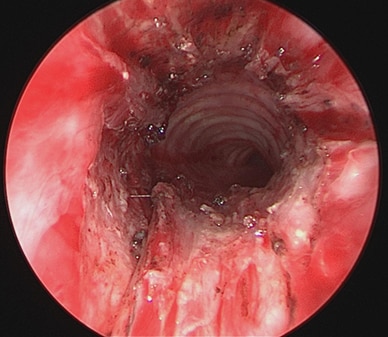
Postoperative appearance of the same stenosis
Postoperative appearance of the same stenosis following triamcinolone injection, CO2 laser vaporization and mitomycin C application.
Surgery for ISS involves injection of the stenotic mucosa with triamcinolone, followed by CO2 laser vaporization of the stenotic lesion, followed by application of mitomycin C. This approach was confirmed by research published in Laryngoscope in 2014. The surgery is done under general anesthesia and typically followed by same-day discharge.
Medical therapy for ISS is inhaled glucocorticoids, trimethoprim-sulfamethoxazole, and proton-pump inhibitors plus lifestyle modifications to limit gastroesophageal acid reflux. There is little randomized controlled data on treatment of this disease, but Mayo Clinic's experience with this combined approach suggests that ISS recurs less frequently for patients treated with this strategy than for patients treated with endoscopic therapy alone. For patients who have unrelenting recurrences or stenosis too thick and complex for endoscopic therapy, primary tracheal resection with end-to-end anastomosis is an option.
At Mayo Clinic, patients with known or suspected ISS are evaluated by subspecialists in otorhinolaryngology and pulmonology. Clinical trials are ongoing for patients with this disease, including specimen registry for tissue use in histopathologic studies and use of different pulmonary function techniques for diagnosis and monitoring of ISS patients.
For more information
To learn more about ISS-related research at Mayo Clinic, contact Dante N. Schiavo, M.D., at schiavo.dante@mayo.edu. To refer a patient, contact 800-533-1564 or 507-266-0416.
Maldonado F, et al. Idiopathic subglottic stenosis: An evolving therapeutic algorithm. Laryngoscope. 2014;124:498.