Jan. 08, 2019
Peripheral pulmonary nodules are a common abnormality seen by pulmonologists. In some cases, nodules are best managed by serial imaging to assess for interval growth. Alternatively, if the pretest probability of malignancy exceeds 70 percent, a lung nodule or mass may be surgically resected without biopsy.
However, there are many lesions of indeterminate probability for lung cancer or metastasis that require biopsy for treatment decisions. CT-guided biopsies are the gold standard for nonsurgical biopsy technique with a diagnostic rate around 90 percent. The drawback is the high rate of pneumothoraces, often quoted as high as 15 percent.
A preoperative intervention also may be required to help the thoracic surgeon localize the nodule while in the operating room to minimize the extent of normal parenchymal resection. A CT-guided transthoracic needle approach is often used for placement of localizing coils or injection of a radionucleotide tracer. These types of procedures usually take place in a separate room in a different part of the hospital.
Because of these limits of CT-guided transthoracic procedures, there have been substantial efforts to find a bronchoscopic technique that rivals CT-guided procedures without the drawbacks. Over the past 10 years there have been many new developments in navigational bronchoscopy, including electromagnetic navigation bronchoscopy, radial probe endobronchial ultrasound (EBUS) and other hybrid techniques.
Many of these modalities use virtual-guidance-based planning derived from a breath-hold CT scan, which potentially puts nodules in a different location within the chest than does bronchoscopy performed with sedation. The virtual nature of some of these bronchoscopic guidance technologies might partially explain diagnostic rates that are disappointingly low in the 60 to 70 percent range. However, the use of cone-beam CT (CBCT) for real-time bronchoscopic navigation has received increasing interest in the past year.
CBCT scanning technology is not new. It has been available for over 20 years and has been used by oral surgeons, orthopedic surgeons, vascular surgeons and interventional radiologists, among others.
Comparison of standard CT and CBCT
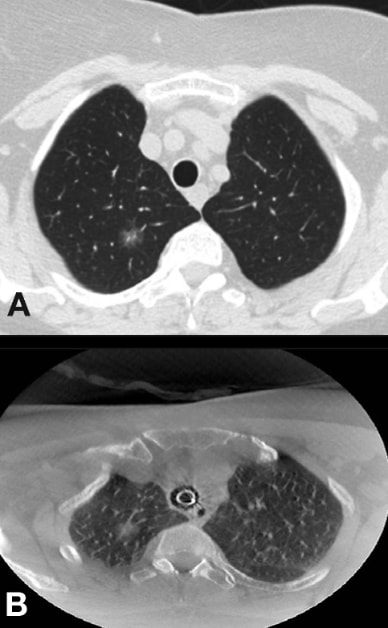
Comparison of standard CT and CBCT
Comparison of standard CT and cone-beam CT (CBCT) in the same patient. Note the same nodule looks to be in a different position. A. Pre-op standard breath-hold CT. B. Intra-op cone-beam CT.
CBCT fused with fluoroscopy for real-time guidance
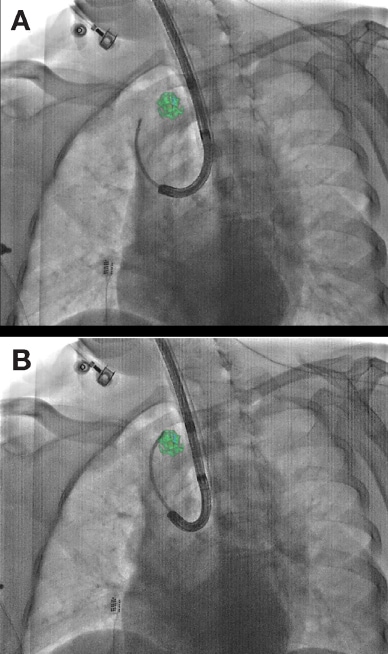
CBCT fused with fluoroscopy for real-time guidance
Cone-beam CT (CBCT) fused with fluoroscopy for real-time guidance. A. Navigation based on pre-op CT. B. Navigation based on intra-op cone-beam CT.
Surgical resected specimen
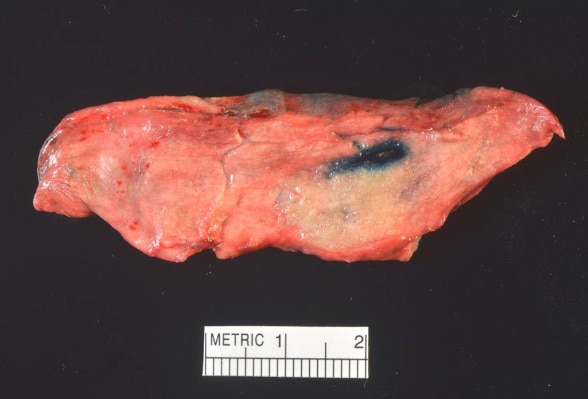
Surgical resected specimen
Surgical resected specimen from same patient showing dye-marked tumor in same configuration as image showing navigation based on intra-op cone-beam CT.
CBCT scanning essentially utilizes a fluoroscopy C-arm that rotates around the patient and provides a real-time CT image. The quality is not as high as that of a standard multidetector CT scan, but CBCT image quality is sufficient for localizing pulmonary nodules, with the added benefit of real-time 3D guidance to confirm a lesion has been accessed. A CBCT scan can also be fused with fluoroscopy to allow precise localization.
A study published in the Journal of Bronchology & Interventional Pulmonology in 2018 described the first large patient series using CBCT with augmented fluoroscopy combined with more conventional navigational bronchoscopy techniques to biopsy 93 lesions with a median size of 16.0 mm in 75 consecutive patients. The overall diagnostic yield was about 84 percent, approaching yields found with a CT-guided transthoracic needle approach.
At Mayo, interventional pulmonologists and thoracic surgeons are exploring the use of CBCT during bronchoscopy, in the hope that CBCT will allow improvements over existing navigational bronchoscopy techniques. In the near future, the use of this technology may allow bronchoscopic therapeutics for malignant lesions in the lungs.
For more information
Pritchett MA, et al. Cone-beam CT with augmented fluoroscopy combined with electromagnetic navigation bronchoscopy for biopsy of pulmonary nodules. Journal of Bronchology & Interventional Pulmonology. 2018;25:274.