Aug. 21, 2018
Glial fibrillary acidic protein (GFAP) autoantibody-positive meningoencephalomyelitis is a newly described entity characterized by a corticosteroid-responsive meningoencephalomyelitis accompanied by immunoglobulin (GFAP-IgG). Some patients with GFAP autoantibody-positive meningoencephalomyelitis have been reported to have bilateral optic disk edema, which is often asymptomatic and was first recognized in this clinical phenotype of encephalomyelitis prior to discovery of GFAP-IgG.
John J. Chen, M.D., Ph.D., and a research team with Ophthalmology at Mayo Clinic's campus in Rochester, Minnesota, performed an observational case series of Mayo Clinic patients to better define the optic disk edema seen in GFAP autoantibody-positive meningoencephalomyelitis. The results were presented at the American Academy of Ophthalmology meeting in November 2017, leading to an award for best research presentation in neuro-ophthalmology, and published online in the Journal of Neuro-Ophthalmology in 2017.
The researchers reviewed all Mayo Clinic patients with GFAP-IgG meningoencephalitis from Jan. 1, 2000, until Dec. 31, 2016, and identified 10 patients with optic disk edema. The visual acuity was unaffected and the disk edema was bilateral in all cases. The optic disk edema resolved with corticosteroid treatment but resulted in mild optic atrophy in two patients. Nine of the 10 patients had radial perivascular enhancement on MRI. Other characteristics included the following:
- Median age was 39.5 years.
- Six patients (60 percent) were male.
- Mild vitreous cell was noted in three patients.
- Median lumbar puncture opening pressure was 144 mm H20 (range 84 to 298 mm H20).
- All patients had inflammatory cerebrospinal fluid.
- Fluorescein angiography was available for one patient with optic disk edema, which showed selective leakage from the venules.
"The clinical presentation of this disorder is quite broad and can range from subacute to chronic encephalitis with or without accompanying meningitis or myelitis. Patients can have characteristic radial perivascular enhancement on MRI, although other enhancement patterns may be encountered (leptomeningeal enhancement), and most have inflammatory cerebrospinal fluid," says Dr. Chen.
Although the optic disk edema was typically asymptomatic and mimicked papilledema, the opening pressure was normal in the majority of the patients. "Only two patients in our cohort of GFAP autoantibody-positive meningoencephalitis had a mildly elevated opening pressure, indicating that raised intracranial pressure is unlikely the primary cause for the optic disk edema in the majority of cases," says Dr. Chen. "The characteristic radial perivascular enhancement on MRI supports a venular process, which suggests that the optic disk edema may be a papillitis from an inflammatory vasculopathy as opposed to papilledema from raised intracranial pressure.
Selective involvement of the venules on fluorescein angiogram
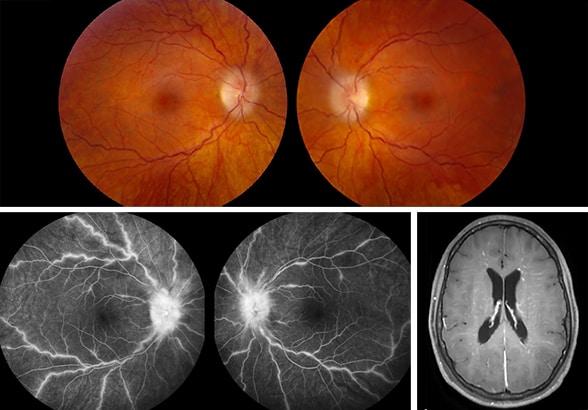
Selective involvement of the venules on fluorescein angiogram
A 29-year-old female with GFAP autoantibody-positive meningoencephalitis initially presented with severe headaches and bilateral optic disk edema. Fluorescein angiogram shows prominent leakage of the retinal venules and optic disks with sparing of the arterioles. T1-weighted MRI with contrast reveals the characteristic radial enhancement that is often seen in patients with GFAP meningoencephalitis. Image reprinted with permission from Journal of Neuro-Ophthalmology.
"In addition, the fluorescein angiogram had a similar appearance to frosted branch angiitis, which is caused by multiple etiologies — including infection, inflammation and neoplasm — where disk edema is the result of papillitis. The selective involvement of the venules on fluorescein angiogram was striking and clearly indicates that the development of optic disk edema is a process that primarily affects the veins as opposed to the arteries."
Dr. Chen notes that the clinical characteristics of GFAP autoantibody-positive meningoencephalitis are still being elucidated. "We recommend testing cerebrospinal fluid GFAP autoantibodies in patients with unexplained meningoencephalitis, particularly if they have bilateral optic disk edema, accompanying myelitis or radial perivascular enhancement on MRI," he says. "The optic disk edema is likely due to an inflammatory papillitis affecting the venules as opposed to elevated intracranial pressure."
For more information
Chen JJ, et al. Optic disc edema in glial fibrillary acidic protein autoantibody-positive meningoencephalitis. Journal of Neuro-Ophthalmology. 2017;1.10.1097/WNO.0000000000000593.