June 27, 2020
Although rare, moyamoya disease can have devastating consequences, triggering strokes and seizures in children and adults. Mayo Clinic's approach utilizes a multidisciplinary moyamoya clinic to provide timely evaluation and treatment for this complex disorder.
"The moyamoya clinic is a one-stop shop where patients can be seen in a single day by experts in vascular neurology and vascular neurosurgery. During the same clinic visit, these specialists discuss the diagnosis and generate a treatment plan," says Rabih G. Tawk, M.D., a neurosurgeon and co-director of the moyamoya clinic at Mayo Clinic in Jacksonville, Florida.
As a high-volume center, Mayo Clinic has experience and expertise in rare conditions. Moyamoya disease is a progressive disorder characterized by blockage in the distal internal carotid artery and adjacent blood vessels. The name moyamoya means "puff of smoke" in Japanese, and describes the appearance of the tangle of tiny blood vessels formed to compensate for the blockage.
Moyamoya disease can occur at any age, but symptoms are most common in children ages 5 to 10 and adults ages 30 to 50. The first symptom is usually stroke or recurrent transient ischemic attack, especially in children, whose symptoms might be mistakenly attributed for months.
"It can be devastating for a young patient when stroke happens, especially when that person is at risk of recurrent stroke or even cerebral hemorrhage," says Michelle P. Lin, M.D., M.P.H., a stroke neurologist and co-director of the moyamoya clinic at Mayo's campus in Florida.
The cause of moyamoya disease is unknown, although the disease is most common in East Asia and a genetic component is suspected. Some patients have moyamoya syndrome, defined as moyamoya caused by an underlying condition such as vasculitis, atherosclerosis or a blood-clotting disorder. Moyamoya syndrome is usually unilateral.
To facilitate current and future research, Mayo Clinic has a biobank with blood samples collected from patients with rare disorders, including moyamoya. "We have a long-term commitment to understanding moyamoya disease and to improving treatment for patients," Dr. Tawk says.
Finding subtle indicators of disease
Early diagnosis and treatment of moyamoya disease are essential to prevent debilitating stroke and seizures. But diagnosis is challenging, as moyamoya disease has many mimics. "Unless you're an expert, moyamoya is difficult to detect. The indicators of disease can be subtle," Dr. Tawk says.
Physicians should consider referring a patient to moyamoya specialists if the patient has had recurrent strokes and has signs of large vessel cerebrovascular disease. Other signs — which can be especially helpful in a patient whose stroke has gone undiagnosed — include unilateral vasculopathy, headache and cognitive decline.
Conventional angiogram, which is the diagnostic test of choice, might show the extent of occlusive disease and the characteristic puff of smoke appearance of small blood vessels. "These findings are suggestive of moyamoya disease. But further testing is needed to determine if the patient has moyamoya or a mimic," Dr. Lin says.
Mayo Clinic uses several state-of-the-art diagnostic tests, starting with comprehensive cerebral angiogram. The imaging is evaluated by specialists with experience in this rare condition. "We have seen several patients in our clinic who had imaging done elsewhere and were managed for prolonged periods, but moyamoya was missed," Dr. Tawk says.
High-resolution MRI of the cerebral blood vessel walls is also performed, to help differentiate moyamoya from vasculitis and atherosclerosis. That distinction is crucial, as the treatment pathways for moyamoya disease differ significantly from the approaches to vasculitis and atherosclerosis.
"Each of these diseases has a very distinct pattern on the vessel walls," Dr. Lin says. "The spatial resolution in our MRI is so high that we can literally see different layers of the blood vessel walls — it's almost like looking at a slide through a microscope."
In addition, the moyamoya clinic routinely performs functional MRI with carbon dioxide challenge, to evaluate changes in cerebral hemodynamics. "It's like a stress test to the brain," Dr. Lin says.
Patients with impaired cerebrovascular reserve who "fail" the stress test are at higher risk of stroke or recurrent stroke. "These are important pieces of individualized clinical findings that help guide timing of bypass surgery versus medical treatment," Dr. Lin says.
Personalized treatment
MRI scans show ischemic lesions in the left hemisphere of the brain
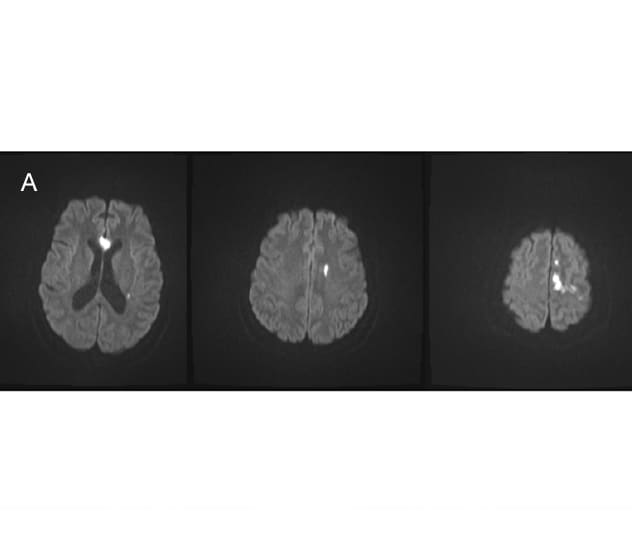
MRI scans show ischemic lesions in the left hemisphere of the brain
A. MRI scans show ischemic lesions in the left hemisphere of the brain of a 35-year-old woman who presented with left hemispheric stroke.
Angiogram showing complete middle cerebral artery occlusion with moyamoya collaterals
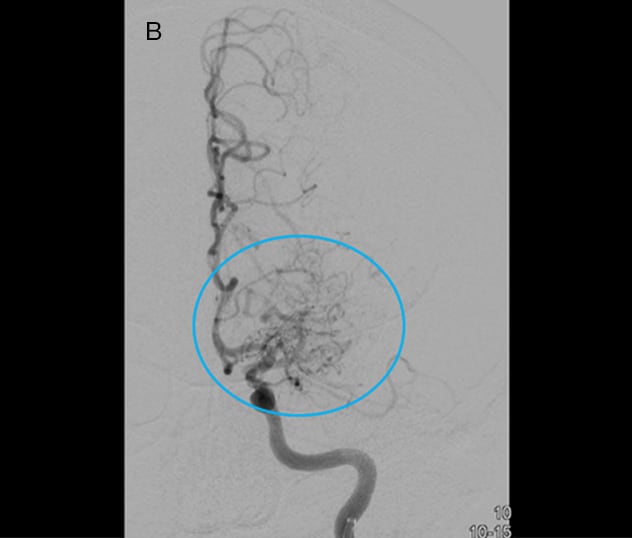
Angiogram showing complete middle cerebral artery occlusion with moyamoya collaterals
B. Angiogram of the left carotid artery shows complete middle cerebral artery occlusion with moyamoya collaterals (blue circle). Angiogram of the right carotid artery (not shown) found evidence of early disease involving the distal internal carotid and middle cerebral arteries.
Angiogram three months after bypass surgery showing a large area of the brain supplied by the bypass
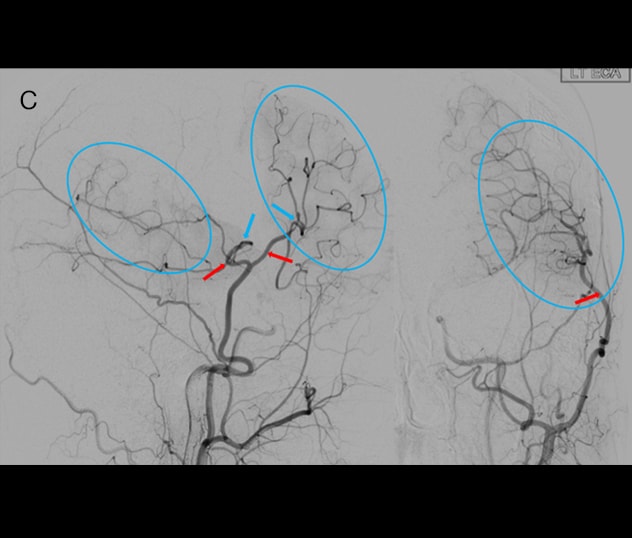
Angiogram three months after bypass surgery showing a large area of the brain supplied by the bypass
C. Angiogram three months after bypass surgery shows donor vessels (red arrows), recipient vessels (blue arrows) and the brain area that became vascularized by the bypass graft (blue circle).
Test results and the clinical work-up are used to generate an individual treatment plan (Figure). "The presentation of moyamoya disease varies, and management has to be individualized to each patient," Dr. Tawk says.
Medical management includes the use of blood thinners, blood pressure medications, cholesterol lowering medications and immunosuppressants. "We're treading a very fine line," Dr. Lin says. "As stroke neurologists, it's important to individualize each patient's stroke and bleeding risks, particularly in patients with moyamoya, as they are at increased risk of both."
For example, patients who are poor metabolizers of the blood thinner clopidogrel — an estimated 14% of the population — have an increased risk of stroke. "At our moyamoya center, we routinely check if a patient is a clopidogrel responder versus a nonresponder, and titrate the blood thinness with the anti-platelet level," Dr. Lin says.
Surgery involves direct or indirect revascularization. Mayo Clinic neurosurgeons are able to perform combined direct and indirect revascularization to provide optimal surgical outcomes while minimizing complications. "Patients do best when the surgery is individualized to meet their needs," Dr. Tawk says.
Collaboration between neurosurgeons and stroke neurologists is also key, particularly for patients with moyamoya syndrome. In one recent case, Dr. Lin identified thyrotoxicosis in a patient with moyamoya.
"We performed unilateral bypass surgery, which immediately reduced the patient's risk of stroke," Dr. Tawk says. "Then, by treating the underlying pathology, we stopped additional injuries to the blood vessels on the contralateral brain."
Individuals with moyamoya disease require lifelong care. The moyamoya clinic performs regular follow-up imaging to determine if a patient's vascular bypass has matured. If a bypass regresses and patients continue to have symptoms, additional surgery might be needed. Patients can receive initial or follow-up care at any Mayo Clinic campus, as all three academic campuses have cerebrovascular specialists with experience in moyamoya.
"Mayo is unique in that our colleagues throughout the system help one another," Dr. Tawk says. "Patients have the expertise of not just an individual physician but many experts who come together to recommend what can best help that individual."