Oct. 22, 2019
Permanent hypoparathyroidism is an uncommon complication after total thyroidectomy, but can have significant consequences for affected patients. It can occur in up to 6% of patients and leads to lifelong dependency on calcium supplements and calcitriol. Patients will often have symptoms of numbness and tingling periorally, as well as in their fingertips, that can be difficult to manage.
Recombinant parathyroid hormone injection therapy also has been used in these patients, but it can be expensive, inconvenient and poorly tolerated secondary to side effects. It also carries a potential risk of osteosarcoma.
Recently, indocyanine green fluorescence angiography has been used as an adjunct to visual identification of parathyroid glands to assess blood flow and viability after total thyroidectomy.
Indocyanine green fluorescence angiography assessment of parathyroid blood supply
Indocyanine green fluorescence angiography assessment of parathyroid blood supply
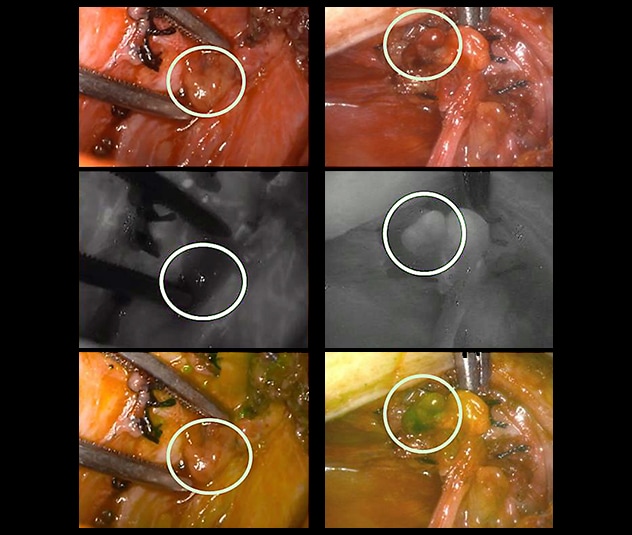
The images on the left show a parathyroid gland that appears to be well vascularized but is poorly perfused based on indocyanine green fluorescence angiography, leading to auto-transplantation. On the right, a parathyroid gland that appears to have vascular congestion has avid uptake on indocyanine green fluorescence angiography, showing that it is well vascularized and will function normally postoperatively.
In a study published in 2019 in the World Journal of Surgery, researchers with Endocrine Surgery at Mayo Clinic in Rochester, Minnesota, found indocyanine green fluorescence angiography to be a useful adjunct in assessing parathyroid blood supply compared with visual inspection alone.
"Indocyanine green fluorescence angiography has been a game changer in thyroid surgery," says Melanie L. Lyden, M.D., senior author of the manuscript. "For decades, visual inspection and incising the parathyroid gland to see if it bleeds have been the only ways to validate parathyroid presence and function. Now we have real-time data that help us identify parathyroid glands and ensure that they are functioning. If they have a compromised blood supply, we can auto-transplant them to minimize the incidence of long-term dysfunction.
"Visual inspection was found to be inaccurate 15% of the time, which means that viable parathyroid glands were excised and auto-transplanted when they didn't need to be and nonviable glands were not auto-transplanted when they should have been. We also found that when fluorescent imaging confirms well-vascularized parathyroid glands, we can be reassured that their parathyroid hormone level is adequate."
To perform angiography after a total thyroidectomy, specialists inject patients with 3 to 4 mL of indocyanine green and the vascularity is evaluated using a Pinpoint camera — a fluorescent imaging camera that uses white light. Well-perfused parathyroid glands take up the indocyanine green and display a visible fluorescence, while glands that may have been compromised during total thyroidectomy have weak or no fluorescence, prompting auto-transplantation.
Patients with well-perfused parathyroid glands are given a score of 2, which has been predictive of normal parathyroid function immediately after thyroid surgery. Those with a compromised blood supply are given a score of 1 or 0, which may lead to auto-transplantation to preserve long-term parathyroid function.
Benzon M. Dy, M.D., a consultant with Endocrine Surgery at Mayo Clinic in Rochester, Minnesota, concludes: "It is difficult to know in the early stages of this new technology if long-term hypoparathyroidism will be prevented, given its overall low incidence. However, this objective assessment also helps to identify patients who may be at risk of short-term hypocalcemia, and allows us to initiate treatment sooner. Overall, indocyanine green fluorescence angiography is a safe and inexpensive adjunct that provides real-time data to the surgeon and may have other implications in the future as its use is expanded in patients with bulky central compartment lymphadenopathy and invasive thyroid cancers."
For more information
Rudin AV, et al. Evaluation of parathyroid glands with indocyanine green fluorescence angiography after thyroidectomy. World Journal of Surgery. 2019;43:1538.