June 21, 2022
This Q&A features Casey L. Swanson, P.A.-C., a physician assistant in Obstetrics and Gynecology specializing in hereditary ovarian cancer at Mayo Clinic's Minnesota campus. She answers questions medical professionals may have about patients who have learned they have an inherited gene increasing their ovarian cancer risk.
When do you see patients about genetic mutations and ovarian cancer risk? What is their situation?
A mutation in a gene may predispose to ovarian cancer
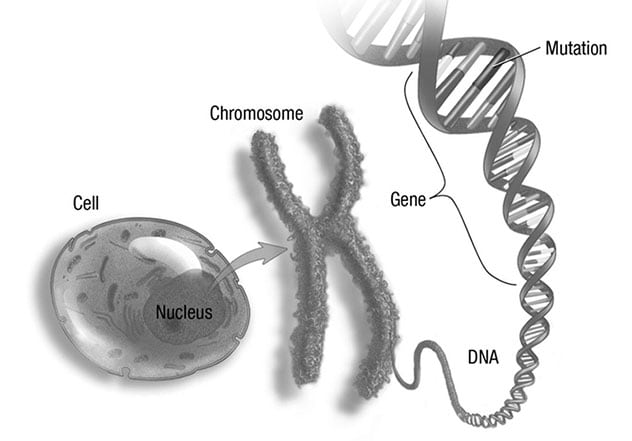
A mutation in a gene may predispose to ovarian cancer
Each cell has chromosomes in its nucleus. Chromosomes are long chains of DNA that contain genes that may include a mutation.
There are several pathways that lead patients to undergo genetic testing. Often, patients learn about a genetic mutation after health care providers discover they have cancer and subsequently pursue genetic testing. Other patients may have a relative with a hereditary ovarian cancer gene, and these patients obtain testing for the same gene. Occasionally, patients see me due to results of genetic testing performed for their personal interest.
Recently, investigators for Tapestry DNA Sequencing Research Study, a Mayo Clinic Center for Individualized Medicine genomic sequencing study, have referred patients after finding they have a mutation known to increase their ovarian cancer risk.
What ages are the individuals who have these mutations?
All women with a germline mutation for ovarian cancer are born with the mutation. However, medical professionals often defer genetic testing until a woman is 18 years of age.
The women I see with a hereditary ovarian cancer mutation vary greatly by age. They can be in their 20s to their 80s.
How many mutations have been identified? How often are mutations involved in ovarian cancer?
Currently, there are 11 genes recognized by the National Comprehensive Cancer Network (NCCN) that increase the risk of developing ovarian cancer. These include: BRCA1, BRCA2, BRIP1, MLH1, MSH2, MSH6, PMS2, EPCAM, PALB2, RAD51C and RAD51D.
Patients diagnosed with epithelial ovarian cancer have a 20% chance of having an underlying germline mutation.
What is the emotional state of these individuals when you meet?
Most women are fearful with the thought of developing and dying of ovarian cancer. Ovarian cancer is the fifth most common cause of cancer death in women. Many have witnessed family members who have undergone treatment for ovarian cancer and very possibly passed away from this cancer.
What do you recommend to these patients so they do not live in fear?
I spend time talking to patients about their ovarian cancer risks at their current ages and about strategies to decrease the risk of developing ovarian cancer. We talk about risk-reducing surgery to remove their ovaries and fallopian tubes at the recommended age based on their specific mutations.
I inform my patients that there are support groups and societies for them to meet other women with similar mutations. This can help them not feel alone, and they learn about how others have lived with the mutation. I also let them know that therapists can provide help regarding cancer fear.
Who should be tested in a family with an identified genetic mutation?
After someone tests positive for a germline mutation linked to ovarian cancer, it is recommended that all first-degree relatives — parents, siblings and children — meet with a genetic counselor to discuss testing. Then, any of these relatives testing positive for the gene should recommend genetic counseling to their offspring.
What are the benefits of a genetic counselor and determining if a mutation is present?
Genetic counselors are essential to genetic testing at Mayo Clinic. They assist patients by helping them make genetic testing decisions, preparing them for positive and negative test results, helping interpret genetic testing results, discussing insurance concerns and helping navigate insurance approval. They also help patients talk to their family members about their test results if testing identifies a germline mutation.
What do you suggest when a patient's family member is unwilling to have genetic testing?
I let them know I understand it is a personal decision to undergo genetic testing. I share with them my thoughts about why it would be important to know if they have a hereditary genetic mutation so they can screen for certain cancers and consider risk-reducing surgeries.
How elevated is ovarian cancer risk if genetic testing reveals mutation?
The 11 genetic mutations associated with ovarian cancer each carry a different lifetime risk of developing ovarian cancer. This risk ranges from 3% to 45%, depending on the mutation.
What reduces ovarian cancer risk for these individuals?
The only way to decrease the risk of dying from ovarian cancer is to have an oophorectomy and a salpingectomy.
There are other things shown to decrease the chance of developing ovarian cancer, such as use of combined oral contraceptive pills, tubal ligation, salpingectomy, hysterectomy, breastfeeding and having had children. However, investigators have not shown these factors to decrease risk of dying from ovarian cancer.
What do you recommend for patients who learn they have a genetic mutation elevating their ovarian cancer risk?
My recommendations are to some degree individualized for patients based on age, mutation, childbearing status and any ongoing cancer treatment. I follow the NCCN guidelines for the specific mutation to determine at what age to recommend surgery to remove ovaries and fallopian tubes. Some of these mutations also put patients at higher risk of uterine cancer; therefore, sometimes I am also recommending hysterectomy.
What do you tell women with these genetic mutations who want to have children?
I let them know I never want them to feel rushed to have their ovaries removed if they want to have children naturally. They should attempt to have children when it fits into their lives. For my younger patients, I remind them of their low risk of developing ovarian cancer at their current age.
Women have a 50% chance of passing on the germline mutation to their offspring. For those concerned about this possibility, I let them know I can refer them to Reproductive Endocrinology and Infertility, where they can discuss preimplantation genetic testing.
Do you take referrals from other medical centers?
Yes, outside providers do refer patients to Mayo Clinic. The Breast Clinic and our group often collaborate in seeing these patients.
Why should a physician refer a patient to Mayo Clinic if a genetic mutation is discovered?
Here are a few considerations:
- Clinical proficiency. Clinicians at Mayo Clinic are very familiar with genetic abnormalities and can discuss surgery, symptoms and lifestyle modifications.
- Radiological expertise. Mayo Clinic has radiologists specialized in gynecological imaging. They can help identify features on pelvic imaging that may be concerning for cancer in patients at high risk.
- Multidisciplinary. In conjunction with the Women's Health Clinic and other specialists, Mayo Clinic has great resources for concerns that patients with genetic mutations may have.
- Surgical and pathology skill. Mayo Clinic Gynecologic Oncology surgeons perform hysterectomy, oophorectomy, salpingectomy and salpingo-oophorectomy routinely and operate on ovarian cancer cases frequently. Pathologists have considerable experience in tissue sample examination and know what to expect.
I would suggest that physicians send to Mayo Clinic their patients who learn a first-degree relative has a genetic mutation. We can follow them through this journey with elevated cancer risk due to genetic mutation, freeing referring physicians to take care of patients' other medical concerns.
For more information
Tapestry DNA Sequencing Research Study. Center for Individualized Medicine. Mayo Clinic.
Refer a patient to Mayo Clinic.