Overview
Vaginal cancer
Vaginal cancer
Vaginal cancer begins as a growth of cells in the vagina. The vagina is the muscular tube that connects the uterus with the outer genitals.
Vaginal cancer is a growth of cells that starts in the vagina. The cells multiply quickly and can invade and destroy healthy body tissue.
The vagina is part of the female reproductive system. It's a muscular tube that connects the uterus with the outer genitals. The vagina is sometimes called the birth canal.
Cancer that begins in the vagina is rare. Most cancer that happens in the vagina starts somewhere else and spreads to the vagina.
Vaginal cancer that's diagnosed when it's confined to the vagina has the best chance for a cure. When the cancer spreads beyond the vagina, it's much harder to treat.
Products & Services
Symptoms
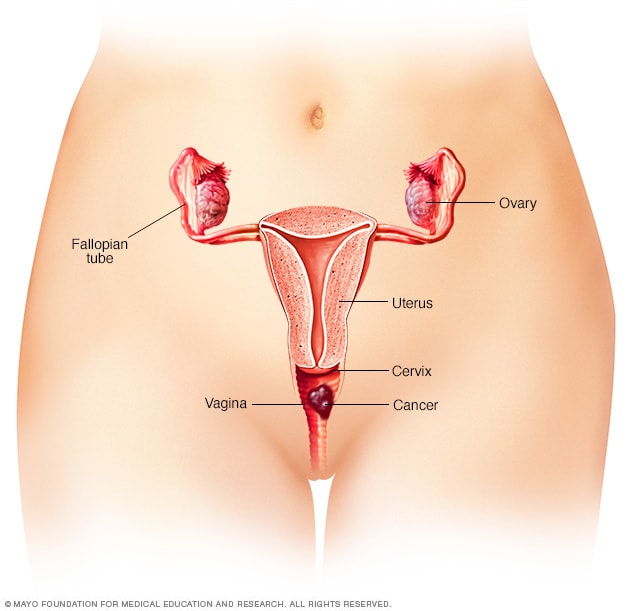
Female reproductive system
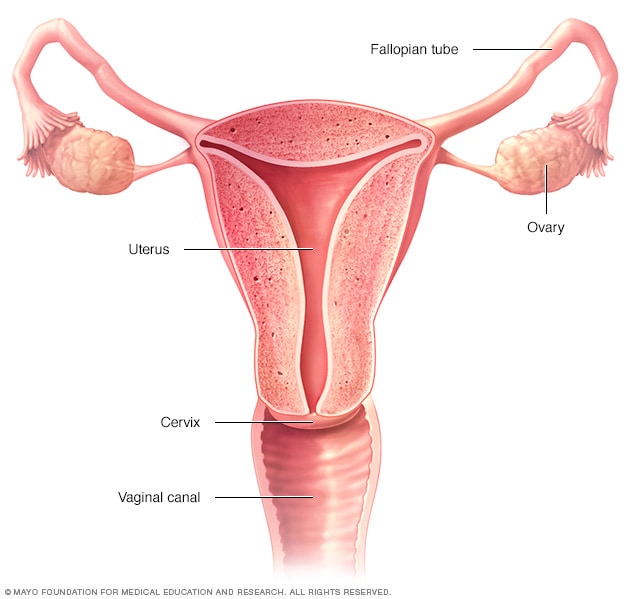
Female reproductive system
The ovaries, fallopian tubes, uterus, cervix and vagina, also called the vaginal canal, make up the female reproductive system.
Vaginal cancer may not cause any symptoms at first. As it grows, vaginal cancer may cause signs and symptoms, such as:
- Vaginal bleeding that isn't typical, such as after menopause or after sex.
- Vaginal discharge.
- A lump or mass in the vagina.
- Painful urination.
- Frequent urination.
- Constipation.
- Pelvic pain.
When to see a doctor
Make an appointment with a doctor or other healthcare professional if you have any persistent symptoms that worry you.
Causes
Layers of vaginal tissue
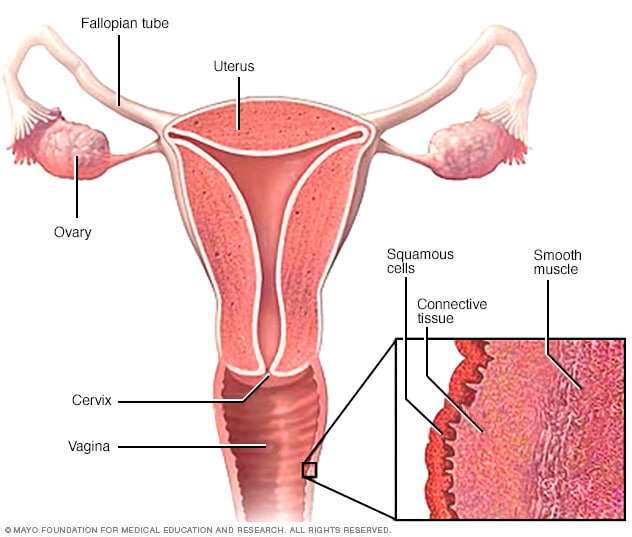
Layers of vaginal tissue
Vaginal cancer most commonly begins in the thin, flat squamous cells that line the surface of the vagina. Other types of vaginal cancer may occur in other cells on the surface of the vagina or in the deeper layers of tissue.
Vaginal cancer begins when cells in the vagina develop changes in their DNA. A cell's DNA holds the instructions that tell a cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells might form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
Most DNA changes that lead to vaginal cancers are thought to be caused by human papillomavirus, also called HPV. HPV is a common virus that's passed through sexual contact. For most people, the virus never causes problems. It usually goes away on its own. For some, though, the virus can cause changes in the cells that may lead to cancer.
Types of vaginal cancer
Vaginal cancer is divided into different types based on the type of cells affected. Vaginal cancer types include:
- Vaginal squamous cell carcinoma, which begins in thin, flat cells called squamous cells. The squamous cells line the surface of the vagina. This is the most common type.
- Vaginal adenocarcinoma, which begins in the glandular cells on the surface of the vagina. This is a rare type of vaginal cancer. It's linked to a medicine called diethylstilbestrol that was once used to prevent miscarriage.
- Vaginal melanoma, which begins in the pigment-producing cells, called melanocytes. This type is very rare.
- Vaginal sarcoma, which begins in the connective tissue cells or muscles cells in the walls of the vagina. This type is very rare.
Risk factors
Factors that may increase your risk of vaginal cancer include:
Increasing age
The risk of vaginal cancer increases with age. Vaginal cancer happens most often in older adults.
Exposure to human papillomavirus
Human papillomavirus, also called HPV, is a common virus that's passed through sexual contact. HPV is thought to cause many types of cancer, including vaginal cancer. For most people, HPV infection goes away on its own and never causes any problems. But for some, HPV can cause changes in the cells of the vagina that increase the risk of cancer.
Smoking
Smoking tobacco increases the risk of vaginal cancer.
Exposure to miscarriage prevention medicine
If your parent took a medicine called diethylstilbestrol while pregnant, your risk of vaginal cancer might be increased. Diethylstilbestrol, also called DES, was once used to prevent miscarriage. It's linked to a type of vaginal cancer called clear cell adenocarcinoma.
Complications
Vaginal cancer can spread to other parts of the body. It most often spreads to the lungs, liver and bones. When cancer spreads, it's called metastatic cancer.
Prevention
There is no sure way to prevent vaginal cancer. However, you may lower your risk if you:
Seek out regular pelvic exams and Pap tests
Regular pelvic exams and Pap tests are used to look for signs of cervical cancer. Sometimes vaginal cancer is found during these tests. Ask your healthcare team how often you should undergo cervical cancer screening tests and which tests are best for you.
Consider the HPV vaccine
Receiving a shot to prevent HPV infection may lower the risk of vaginal cancer and other HPV-related cancers. Ask your healthcare team whether an HPV vaccine is right for you.