Diagnosis
Your baby's healthcare professional will ask you questions about symptoms and do a physical exam.
Sometimes, an olive-shaped lump can be felt on the baby's belly. This lump is the enlarged pyloric muscle. This is more common in later stages of the condition.
Wavelike contractions may sometimes be visible when examining the baby's belly, particularly after feeding or before vomiting.
Imaging tests
Imaging tests may be used to diagnose pyloric stenosis or rule out other conditions. These tests include:
- Ultrasound. The standard diagnostic tool for pyloric stenosis is an ultrasound exam. This generally simple exam is done with a device placed on the baby's belly. The ultrasound image can show enlargement of the pyloric valve.
- X-ray: A specialized X-ray exam can create a brief video of the stomach in action. A special liquid fed to the baby is visible as it enters and exits — or tries to exit — the stomach. This test is used less often than ultrasound.
Blood tests
Your healthcare professional may order blood tests. The results can show signs of electrolyte imbalances and dehydration.
Treatment
Pyloromyotomy
Pyloromyotomy
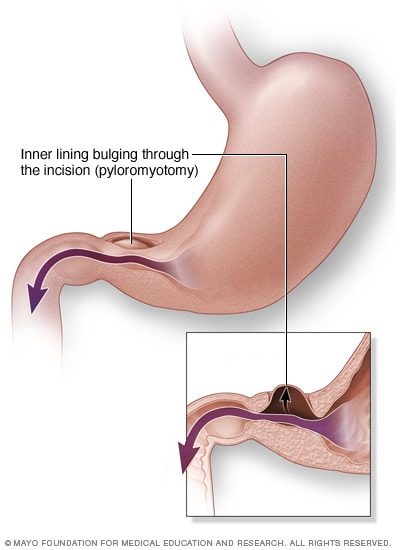
In a pyloromyotomy, the surgeon cuts into the ring-shaped muscle of the pyloric valve and separates the muscle tissue as far as the stomach lining. The lining bulges through the gap in the muscle. The loosened muscle works, but it allows food to pass through.
Surgery is needed to treat pyloric stenosis. Before surgery, fluids and electrolytes are given through a tube placed in a vein. Proper hydration and electrolyte balance are needed before the procedure. This may take 24 to 48 hours.
The procedure is called pyloromyotomy. In pyloromyotomy, the surgeon cuts into the thickened muscle of the pyloric valve. Then a device is used to spread the muscle apart down to the stomach lining tissues.
The pyloric muscle will still work, but this gap loosens the muscle and will allow food to move out of the stomach. The stomach lining will bulge into the open space, but the stomach contents won't leak out.
Most often the surgery is done through three small openings in the belly. One is used for a video camera, and two are for surgical tools. This is called laparoscopic surgery. In some cases, a doctor will do an open surgery through one larger opening. Laparoscopic surgery generally has a shorter recovery time.
After surgery:
- Your baby will be carefully watched for at least 24 hours.
- Recommendations for feeding after surgery may vary. In most cases, feeding can begin 12 to 24 hours after the procedure.
- Your healthcare team may recommend feeding when your baby is hungry, or they may recommend a schedule.
- Some vomiting may occur after surgery.
- During follow-up appointments, your care team will check your baby's weight, growth and development.
Possible complications from pyloric stenosis surgery include bleeding and infection. However, complications aren't common, and the results of surgery are generally excellent.
Treatment option
Rarely, if a baby has very high risks for surgery, a medicine may be used to treat pyloric stenosis. A medicine called atropine sulfate may help relax the pyloric muscle tissue.
This treatment is not as effective and requires longer hospital stays than surgery.
Preparing for your appointment
Your child's primary healthcare professional will likely do the exam and make a diagnosis, but you may be referred to a specialist in digestive disorders called a gastroenterologist. If the diagnosis is pyloric stenosis, you'll be referred to a pediatric surgeon.
What you can do
- Write down your baby's symptoms, including when and how often your baby vomits, whether the vomit is forcefully projected, and if the vomit appears to be most or just part of what the baby has eaten.
- Write down questions to ask your healthcare professional.
Questions to ask your doctor
- What's the most likely cause of my baby's symptoms?
- What tests does my baby need? Do they require any special preparation?
- Does my baby need surgery?
- Will there be any feeding restrictions after surgery?
In addition to the questions that you've prepared, don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your healthcare professional is likely to ask you a few questions. Being ready to answer them may leave time to go over points you want to spend more time on. You may be asked:
- When did your baby first begin experiencing symptoms?
- Are the symptoms continuous or occasional? Do they occur only after eating?
- Does your baby seem hungry after vomiting?
- Does the vomit come out forcefully, leaving your baby's shirt or bib mostly dry?
- What color is the vomit?
- How many wet diapers does your baby have a day?
- Is there blood in your baby's stool?
- What was your baby's last recorded weight?
Dec. 10, 2024