Diagnosis
Diagnosis involves the steps that your healthcare professional takes to find out if you have acromegaly. Your healthcare professional asks about your health history and does a physical exam. You also may need the following tests:
-
IGF-1 measurement. The IGF-1 blood test measures the level of insulin-like growth factor 1 (IGF-1) in your blood. A high IGF-1 level can mean that the level of growth hormone also is high. IGF-1 is a hormone made in the liver in response to the growth hormone. A high IGF-1 level is an important marker for diagnosing acromegaly. But IGF-1 also can be elevated due to other conditions such as diabetes, liver or kidney disease, or pregnancy.
Because of this, healthcare professionals usually confirm the diagnosis with a second test, such as an oral glucose tolerance test (OGTT), and an MRI scan of the pituitary gland to check for a tumor.
It helps confirm an acromegaly diagnosis. The OGTT measures your growth hormone level before and after you drink a type of sugar water called glucose. In people who don't have acromegaly, the glucose drink typically causes the growth hormone level to fall. But if you have acromegaly, your growth hormone level tends to stay high.
- MRI and other imaging tests. An MRI scan of the pituitary gland is the main imaging test for acromegaly. It shows the location and size of a pituitary tumor. If no pituitary tumor is found, your healthcare professional may order other scans to look for tumors elsewhere in the body. X-rays of the hands and feet also may be used to check for changes in bone growth caused by excess growth hormone.
More Information
Treatment
Acromegaly is not always curable, but treatment can often control the disease. The goal of treatment is to improve symptoms, prevent complications, and bring growth hormone (GH) and insulin-like growth factor 1 (IGF-1) levels back to healthy levels. Keeping these hormone levels under control can improve quality of life and lower long-term health risks.
Treatment options for acromegaly include:
- Pituitary tumor surgery to remove the tumor causing the symptoms. This is often the first treatment when acromegaly is due to a pituitary tumor.
- Medicines that lower GH or block its effects. These may be used if surgery doesn't bring hormone levels within the healthy range.
- Radiation therapy to target the tumor and reduce hormone production. This may be recommended if surgery isn't possible, if it can't remove the whole tumor or if medicines don't help enough.
Some people need a mix of these treatments. Your treatment plan depends on factors such as tumor size and location, the severity of symptoms, and your age and overall health.
Treatment can improve some physical features, such as swelling of soft tissues or changes in skin. However, bone enlargement usually cannot be reversed.
If you also have other health conditions related to acromegaly, such as diabetes, sleep apnea or heart disease, you may need additional treatments to manage them.
Pituitary tumor surgery or other procedures
Endoscopic transnasal transsphenoidal surgery
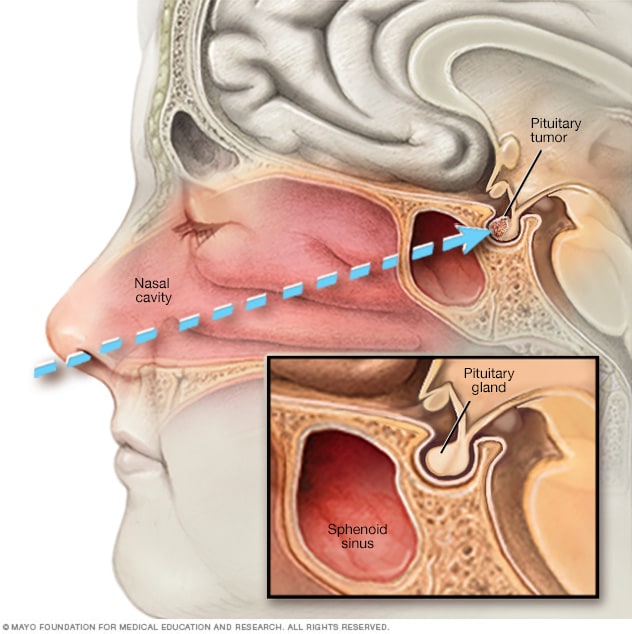
Endoscopic transnasal transsphenoidal surgery
In transnasal transsphenoidal endoscopic surgery, a surgical instrument is placed through the nostril and alongside the nasal septum to access a pituitary tumor.
The main surgical treatment for acromegaly is transsphenoidal surgery. In this procedure, a neurosurgeon removes the pituitary tumor through the nose and a hollow space behind the nasal passages, called the sphenoid sinus. This approach avoids opening the skull and is the most common way surgeons treat acromegaly. If the tumor causing symptoms isn't located on the pituitary gland, the surgeon may recommend another type of surgery to remove the tumor.
Pituitary surgery for acromegaly often returns growth hormone to the right level, especially if the tumor is small. If the tumor was putting pressure on the tissues around the pituitary gland, removing the tumor also can help relieve headaches and vision changes.
Sometimes surgeons can't remove the whole tumor, especially if it has grown close to important nerves or blood vessels. When this happens, growth hormone levels may still be too high after surgery. Additional treatment with another surgery, medicines or radiation therapy may be needed.
Medicines
Medicines for acromegaly can help lower growth hormone (GH) and insulin-like growth factor 1 (IGF-1) levels. Some medicines may block the effects of these hormones. Your healthcare professional may recommend one or more of the following:
- Somatostatin analogues. Somatostatin is a natural brain hormone that limits GH production. The medicines octreotide (Mycapssa, Sandostatin) and lanreotide (Somatuline Depot) lower GH and IGF-1 levels and may shrink the tumor. Taking one of these medicines signals the pituitary gland to make less growth hormone. Mycapssa is a capsule taken by mouth twice a day. The others are monthly injections. In September 2025, the Food and Drug Administration in the U.S. approved a new somatostatin called paltusotine (Palsonify) for the treatment of acromegaly. This is a capsule taken by mouth once a day. Unlike octreotide or lanreotide, which are peptides, paltusotine is not a peptide. That means it is not made of amino acids like proteins are. Instead, it is a small molecule designed to mimic somatostatin's action, with a chemical structure that makes it easier to absorb and able to stay in the bloodstream longer than peptide medicines. Somatostatins are the first line treatment for acromegaly if surgery doesn't improve symptoms.
- Dopamine agonists. Cabergoline and bromocriptine (Cycloset, Parlodel) are medicines taken by mouth that may help lower GH and IGF-1 levels, especially when levels are only slightly high. They also may shrink the tumor. Because higher doses are often needed, side effects such as nausea, tiredness, dizziness, sleep problems or mood changes can occur.
- Growth hormone receptor antagonist. Pegvisomant (Somavert) blocks the effect of growth hormone on the body's tissues, which lowers IGF-1 levels. It does not shrink tumors or reduce GH levels. Pegvisomant is given as a daily shot and may be used when other medicines do not work well enough. Because pegvisomant may affect the liver, regular blood tests are needed to monitor liver function.
Therapies
Radiation therapy for acromegaly is usually used after surgery to destroy leftover tumor cells. It also gradually lowers growth hormone levels, but it may take months or even years before you notice improvement.
Radiation also can lower levels of other pituitary hormones, not just growth hormone levels. If you receive radiation, you'll need lifelong follow-up to monitor your hormone levels and pituitary function.
Types of radiation therapy include:
- Stereotactic radiosurgery. This approach uses 3D imaging to deliver a high dose of radiation precisely to the tumor while limiting exposure to healthy tissue. It is usually given in a single dose. Growth hormone levels may return to a healthy range within several years. The most common technique is called Gamma Knife. This radiosurgery technique does not involve a surgical knife.
- Proton beam radiation. This type of radiation uses tiny particles called protons that target the tumor. It may cause less damage to the pituitary gland and the tissue that surrounds it than does conventional radiosurgery.
- Conventional radiation therapy. This type of radiation involves receiving small doses of radiation over 4 to 6 weeks. The risk of damage to the pituitary gland is higher than it is with proton beam radiation and stereotactic radiosurgery. The full effect of the treatment may take 10 years or more to appear.
Acromegaly prognosis and life expectancy
What is the life expectancy of people with acromegaly?
In the past, people with untreated acromegaly often had a shorter life expectancy because of complications such as heart disease, diabetes, sleep apnea and cancer. Today, with earlier diagnosis and better treatments, the life expectancy with treatment for acromegaly is close to that of people without acromegaly. Many people with acromegaly can live a typical lifespan if their GH and IGF-1 levels are lowered and maintained at healthy levels with treatment.
What is the prognosis for acromegaly?
The prognosis for acromegaly depends on how early the condition is diagnosed and how well the treatment controls hormone levels. Surgery used to completely remove small pituitary tumors may cure acromegaly. Large tumors are harder to remove completely. But medicines and radiation therapy can usually bring GH and IGF-1 levels down to safe ranges.
Even after treatment, some physical changes — such as bone growth in the jaw, hands or feet — may not fully reverse. But controlling hormone levels improves symptoms and reduces the risk of serious complications. Regular follow-up is important to keep hormone levels in check and monitor for any return of tumor growth.
More Information
Preparing for your appointment
You'll likely first see your primary healthcare professional. Or you may be referred right away to a doctor called an endocrinologist who finds and treats hormone conditions.
It's good to prepare for your appointment. Here's some information to help you get ready and to know what to expect from your healthcare professional.
What you can do
- Be aware of any restrictions before the appointment. When you make the appointment, ask if there's anything you need to do to prepare for tests. For instance, you may be asked to stop eating for a certain number of hours before a test. This is called fasting.
- Write down your symptoms. Keep track of anything that causes you discomfort or concern. This may include headaches, vision changes or discomfort in your hands. Write down all of your symptoms, even if they don't seem related to the reason for which you made the appointment.
- Write down key personal information, including any changes in your sex life or menstrual cycle.
- Make a list of all medicines, vitamins and supplements you're taking and the doses.
- Take along old pictures that your healthcare professional can use to compare with your appearance today. Your healthcare professional likely will be interested in photos from 10 years ago through the present.
- Take along a family member or friend if you can. This person may remember something that you miss or forget.
- Write down questions to ask your healthcare professional.
Making a list of questions helps you make the most of your time with your healthcare professional. For acromegaly, some basic questions to ask include:
- What's the most likely cause of my symptoms? Are there other possible causes?
- What tests do I need? And should I see a specialist?
- What treatments are available for this condition? Which approach do you recommend?
- How long will I need treatment before my symptoms improve? Could treatment help me look and feel as I did before I developed symptoms of acromegaly?
- Will I have long-term complications from this condition?
- I have other health conditions. How can I best manage the conditions together?
- Are there brochures or other printed material I can take with me? What websites do you recommend?
Feel free to ask any other questions you have.
What to expect from your doctor
Your healthcare professional is likely to ask you questions such as:
- What are your symptoms, and when did they start?
- Have you noticed any changes in how you look?
- How much would you say your features have changed over time? Do you have old photos I can use for comparison?
- Have you noticed changes in your sleep or your sex life? Do you have headaches or joint pain, vision changes, or more sweating than usual?
- Does anything seem to make your symptoms better or worse?
- Do your old shoes and rings still fit? If not, how much has the fit changed over time?
- Have you had a colon cancer screening test?
Oct. 22, 2025